Abstract
Purpose
Given the biological differences between females and males, sex-specific evaluations should be carried out to obtain better cancer prevention, diagnosis, and treatment strategies. To this purpose, our aim was to evaluate sex differences for toxicity in a cohort of colorectal cancer (CRC) patients undergoing chemotherapy.
Methods
We performed a retrospective study in 329 CRC patients. Differences between males and females were tested performing the Mann-Whitney U test or the Fisher exact test. Multivariate logistic regression models were computed to evaluate the association between sex and risk of chemotherapy agent-related toxicity.
Results
According association sex toxicity, significant differences were observed in the median number of episodes of nausea (p = 0.044), vomit (p = 0.007), heartburn (p = 0.022), thrombocytopenia (p = 0.005), mucositis (p = 0.024). Moreover, statistically significant differences between males and females were observed in the distribution of the highest toxicity grades of nausea (p = 0.024), heartburn (p = 0.016), and thrombocytopenia (p = 0.034). Females have an increased risk of vomit (p = 0.002), alopecia (p = 0.035), heartburn (p = 0.005), mucositis (p = 0.003), and lower risk for thrombocytopenia (p = 0.005).
Conclusion
According to the association of sex chemotherapy agent-related toxicities, females resulted on average at a significant increased risk of more common adverse events (constipation, dysgeusia, alopecia, heartburn, vomit, asthenia, nausea, pain events, and mucositis). Sex-tailored CRC chemotherapy treatment is necessary to obtain efficacy avoiding toxicity, based on patients’ biological and genetic characteristics, a vision that would change CRC setting, a stable disease but still orphan of a real tailored approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aside from gender-specific tumors (breast, prostate, ovarian cancer), recent studies demonstrate gender-specific incidence, progression, and severity of different tumors. Differences have to be investigated in a parameter such as body weight, fat distribution, hormonal profile, metabolism, immune response, and genetics [1, 2]. Among other physiological factors, different metabolic enzymes and specific liver and kidney transporters concur to modulate pharmacokinetics and pharmacodynamics according to gender. Women have a slower gastric emptying time and a bigger distribution volume for lipophilic drugs. Chemotherapeutical compounds show, thus, a 1.7-fold increase in adverse effects in women, although the longer half-life provides a benefit in terms of survival rate [3,4,5,6,7,8]. Analogously, women are more sensitive to toxicity, especially at the gastrointestinal and mucosal level, when treated with 5-fluorouracile. Moreover, nausea and vomit are increased because of the lower efficacy of antiemetic drugs [9, 10].
A gender analysis, therefore, is necessary for the equity of care in clinical settings such as oncology, where extensive and very toxic drugs are widely used [11,12,13]. Sex-specific analyses are of primary importance to establish targeted anti-cancer drug agents. In our study, we explored the effect of sex on reported toxicity in a cohort of colorectal cancer (CRC) patients undergoing different chemotherapy treatments, also considering concomitant administered drugs.
Materials and methods
We performed a retrospective study of CRC-diagnosed patients, enrolled at the Medical Oncology Unit of the Molinette Hospital, AOU City of Health and Science of Turin, from October 2016 to July 2018. The database was prepared with collected data from the TrakCare® Hospital System Medical Records. Inclusion criteria were CRC diagnosis, undergoing active therapy, age ≥ 18 years old, and Day Hospital exclusive affiliation. The following variables were collected: sex, age, TNM classification, comorbidities, drugs taken at home and during chemotherapy treatment, chemotherapy cycle scheme, gastrointestinal toxicity (mucositis, nausea, vomiting, diarrhea, constipation), neurological toxicity (peripheral or central neuropathy), skin toxicity (alopecia, hand-foot syndrome), hematological toxicity (thrombocytopenia, neutropenia, anemia), other toxicities (asthenia, dysgeusia, epistaxis, fever, and hyporessia), pain, epigastralgia, recurrence, visual disturbances, proteinuria, hypertension, and hypotension. Common Terminology Criteria for Adverse Events (CTCAE version 4.0) scoring system was used to detect toxicities. Data were collected for each day of hospital access. Based on the treatment schemes, toxicities have been attributed to several chemotherapy agents at the same time.
In Supplementary Table 1, we reported information on treatment schemes (chemotherapy agents). Patients included had a stable disease and therefore on average characterized by low Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1.
Considering the statistical analysis, the age was described using mean and standard deviations (SD). Categorical variables (tumor classification, reported comorbidities, and type of chemotherapy agent) were described using frequencies and percentages. Gender differences in tumor classification, reported comorbidities, and type of chemotherapy agent were tested performing the Fisher exact test. The distribution of toxicity episodes per patient and the distribution of toxicity grades in the different sex group were evaluated using the Fisher exact test, considering all the therapy agents together. Multivariate logistic regression models, adjusted by age, were computed to evaluate the association between sex and risk of toxicity considering all the treatment and topoisomerase inhibitors, antimetabolite pyrimidine analogues, DNA binding drugs, and grow inhibitor monoclonal antibodies schemes separately. Since the analysis was carried out at the visit level, the Huber-White estimator was used to adjust the correlation between multiple observations on the same patient. Odds ratios (OR) and their 95% confidence intervals (95% CI) were reported. Firth’s correction was applied to reduce the bias of the estimates due to a small number of events. Statistical analyses were performed using R version 3.4.0. The level of significance was set at 0.05.
These data were routinely recorded during daily clinical practice as a quality assurance measure and in order to explore improvements in the quality of services. Ethics committee approval was not required but the research project was the same submitted to the local ethics committee (Prot. N° 0092030, approved). Confidentiality was guaranteed in data collection, analysis, and dissemination phase, by presenting the results in aggregate form.
Results
Study population
We enrolled 329 CRC diagnosed patients, for a total hospital accesses of 10,355 days. Demographics characteristics along with clinical and pharmacological information were reported in Table 1 stratified by sex. Statistically significant differences have been observed on the prevalence of metabolic (12.2% females vs 22.0% males, p = 0.028), endocrine (13.5% females vs 2.9% males, p = 0.001), and renal (3.8% females vs 13.9% males, p = 0.003) comorbidities. Describing chemotherapy regimens, statistically significant differences have been observed in the proportion of females and males treated with topoisomerase inhibitors (respectively 11.5% and 13.9%, p < 0.001), tyrosine kinase inhibitor (0.4% and 1.2%, p < 0.001), and antibiotics (0.5% and 0.1%, p = 0.002).
Association between sex and toxicity
The distribution of the number of toxicity episodes per patient and of the highest toxicity grade stratified by sex is shown in Table 2. Statistically significant differences between females and males were observed in the median number of episodes of nausea (3 [IQR: 0–8] in females and 1 [IQR: 0–6] in males, p = 0.044), vomit (0 [IQR: 0–1] in females and 0 [IQR: 0–0] in males, p = 0.007), heartburn (0 [IQR: 0–1] in females and 0 [IQR: 0–0] in males, p = 0.022), thrombocytopenia (0 [IQR: 0–0] in females and 0 [IQR: 0–1] in males, p = 0.005), mucositis (0 [IQR: 0–2] in females, and 0 [IQR: 0–1] in males, p = 0.024).
Moreover, statistically significant differences between males and females were observed in the distribution of the highest toxicity grades of nausea (p = 0.024), heartburn (p = 0.016), and thrombocytopenia (p = 0.034).
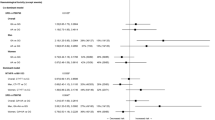
In Table 3, the association between sex and presence/absence of toxicity adjusted by age is shown. Females have an increased risk of vomit (OR: 2.057, 95%CI: 1.306–3.238, p = 0.002), alopecia (OR: 2.120, 95%CI: 1.053–4.268, p = 0.035), heartburn (OR: 1.889, 95%CI: 1.214–2.939, p = 0.005), and mucositis (OR: 1.901, 95%CI: 1.241–2.910, p = 0.003). Instead, females resulted significantly at lower risk for thrombocytopenia (OR: 0.466, 95%CI: 0.273–0.796, p = 0.005).
Association between sex and chemotherapy regimen-related toxicities
In Table 4, the association between sex and chemotherapy regimen-related toxicities adjusted by age is reported. Considering topoisomerase inhibitor regimen, females resulted at a significant increase risk of constipation (OR: 1.529, 95%CI: 1.085–2.334), dysgeusia (OR: 1.687, 95%CI: 1.06–2.685), alopecia (OR: 2.243, 95%CI: 1.616–3.112), and heartburn (OR: 3.406, 95%CI: 1.323–8.766). In patients treated with antimetabolite and pyrimidine analogues, females showed an increased risk of vomit (OR: 1.944, 95%CI: 1.207–3.683), constipation (OR: 1.624, 95%CI: 1.281–2.059), alopecia (OR: 2.833, 95%CI: 2.088–3.845), asthenia (OR: 1.24, 95%CI: 1.094–1.406), heartburn (OR: 2.33, 95%CI: 1.401–3.875), and mucositis (OR: 1.891, 95% CI: 1.149–3.114). Among patients treated with DNA binding drugs, females were at higher risk of nausea (OR: 1.466, 95%CI: 1.008–2.131), vomit (OR: 2.422, 95%CI: 1.091–5.375), constipation (OR: 1.814, 95%CI: 1.261–2.609), alopecia (OR: 3.07, 95%CI: 21.706–5.524), asthenia (OR: 1.383, 95%CI: 1.161–1.648), and heartburn (OR: 2.891, 95%CI: 1.577–5.301). Moreover, for both topoisomerase inhibitor and DNA binding groups chemotherapy regimens, females showed a lower risk of thrombocytopenia (OR: 0.002, 95%CI: 0–0.014 and OR: 0.158, 95%CI: 0.031–0.81, respectively). Finally, for growth inhibitor and monoclonal antibody, females showed an increased risk of asthenia (OR: 1.281, 95%CI: 1.066–1.539) and pain (OR: 2.319, 95%CI: 1.282–4.197) events and a lower risk of dysgeusia (OR: 0.703, 95%CI: 0.495–0.999).
Association between sex and concomitant medication
In the Supplementary Table 2, we described the concomitant medications stratified by sex. Anti-rheumatic agents (1.7% females vs 0 males, p = 0.001), hormones, and anti-hormones (2.2% females vs 0.2% males, p = 0.001) were more frequently used by females.
Discussion
Sex differences in CRC prognosis can be explained by pathophysiological differences between males and females and sex specificity of screening tools, which suggests a potential delay in diagnosis for women. Supporting these pieces of evidence, in our analysis, gender-specific differences have been reported.
As observed in our analysis on topoisomerase inhibitor, antimetabolite and pyrimidine analogues, and DNA binding drugs, a different study reported that more women experienced alopecia compared to men when receiving 5-fluorouracil-based treatment [14,15,16,17,18,19,20,21]. Recently, Tejpar and colleagues, evaluating CRC patients undergoing 5-fluorouracyl/leucovorin/irinotecan (FOLFIRI) scheme, observed that baseline neutrophil count, sex, age, poor performance status, and body surface area were associated with an increased incidence of grade III–IV neutropenia; instead, the main predictors for diarrhea were sex and age [22]. A study conducted by Cristina et al., in a population of 2974 CRC patients undergoing FOLFIRI regimen, reported in female population the following toxic events: a higher rates of nausea, as we observed with DNA binding drugs, vomiting, as reported in our patients treated with antimetabolite and pyrimidine analogues and DNA binding drugs regimens, constipation, as observed with topoisomerase inhibitor, antimetabolite and pyrimidine analogues and DNA binding drugs schemes, cramping, stomatitis, cholinergic syndrome, lethargy, alopecia, in line with topoisomerase inhibitor, antimetabolite and pyrimidine analogues and DNA binding drugs in our results, leukopenia, neutropenia, and anemia [23]. All these results were confirmed by the largest study on CRC patients undergoing 5-fluorouracyl single agent (plus folinic acid), with or without oxaliplatin, capecitabine as a single agent or in combination with oxaliplatin and FOLFIRI regimens: female experienced clinically and statistically significant higher toxicity than males, above all severe neutropenia and leukopenia [24]. Evaluating thrombocytopenia, it is already known that women have a larger platelet count than men [25]. A recent Japan study on antibiotic-induced thrombocytopenia reports that there is a higher drug-induced thrombocytopenia in male patients treated with six different drugs, compared with females [26], as we report for topoisomerase inhibitor and DNA binding drugs. In addition, we observed that the female sex is a negative predictor of dysgeusia in those undergoing topoisomerase inhibitor, growth inhibitor, and monoclonal antibody chemotherapy. Female gender is a risk factor for neurosensory disorders in the head and neck, probably due to the sex hormone receptors in the cranial nerve V complex which lead to hypoactivity of the ganglionic inhibitory system [27]. This could be also the explanation for the more frequent pain in female treated with growth inhibitor and monoclonal antibody. In general, there are pieces of evidence that female perceived more pain than males, considering both clinical pain than those reported in animal models [28]. Considering heartburn, while this disease is more common in man [29], we observed a high frequency in a woman undergoing topoisomerase inhibitor, antimetabolite and pyrimidine analogues, and DNA binding drug chemotherapy. Eventually, pieces of evidence in the literature about asthenia and chemotherapy which separately evaluated sexes are lacking; here, we showed a higher percentage of a female with this side effect, during antimetabolite and pyrimidine analogues and DNA binding drugs, growth inhibitor, and monoclonal antibody schemes.
To better tolerate chemotherapy and to reduce the related adverse events, a large use of concomitant drugs is often required. As reported in the literature, sex is one of the several factors able to influence interpatient variability in the drugs dose effect, affecting both pharmacokinetics and pharmacodynamics [5, 30]. In our analysis, anti-rheumatic agents, hormones, and anti-hormones concomitant drugs were more frequently used by a woman (Supplementary table). Coadministered drugs could differently affect chemotherapy response in male and female patients, giving different outcomes and adverse events.
To confirm the reported results, larger prospective studies, incorporating also genetic markers and female hormonal status data, are warranted. Another important limitation of our study was the lack of pharmacokinetic information. Eventually, since we decided to evaluate the single therapeutic agents and not the schemes taken by each patient, the comparison with previous studies was more difficult; a new study protocol, based on a single chemotherapy scheme, is necessary to confirm our results. Individual dose adjustment, based on therapeutic drug monitoring, could lead to significantly improved response rate, survival rate, and toxicities control [31].
Conclusions
Given the biological and socio-cultural differences between genders, gender-specific analyses should be conducted to provide optimal cancer prevention strategies, to reduce the number of new CRC cases and to better provide treatment both in men and women, a vision that would change the oncology setting of CRC, a stable disease but still orphan of a real tailored approach.
References
Ghosh S, Klein RS (2017) Sex drives dimorphic immune responses to viral infections. J Immunol 198(5):1782–1790. https://doi.org/10.4049/jimmunol.1601166
Takahashi T, Iwasaki A (2021) Sex differences in immune responses. Science 371(6527):347–348. https://doi.org/10.1126/science.abe7199
Buoncervello M, Marconi M, Carè A, Piscopo P, Malorni W, Matarrese P (2017) Preclinical models in the study of sex differences. Clin Sci (Lond) 131(6):449–469. https://doi.org/10.1042/CS20160847
Anderson GD (2008) Gender differences in pharmacological response. Int Rev Neurobiol 83:1–10. https://doi.org/10.1016/S0074-7742(08)00001-9
Gandhi M, Aweeka F, Greenblatt RM, Blaschke TF (2004) Sex differences in pharmacokinetics and pharmacodynamics. Annu Rev Pharmacol Toxicol 44:499–523. https://doi.org/10.1146/annurev.pharmtox.44.101802.121453
Nicolson TJ, Mellor HR, Roberts RR (2010) Gender differences in drug toxicity. Trends Pharmacol Sci 31(3):108–114. https://doi.org/10.1016/j.tips.2009.12.001
Franconi F, Brunelleschi S, Steardo L, Cuomo V (2007) Gender differences in drug responses. Pharmacol Res 55(2):81–95. https://doi.org/10.1016/j.phrs.2006.11.001
Wagner AD, Oertelt-Prigione S, Adjei A, Buclin T, Cristina V, Csajka C, Coukos G, Dafni U, Dotto GP, Ducreux M, Fellay J, Haanen J, Hocquelet A, Klinge I, Lemmens V, Letsch A, Mauer M, Moehler M, Peters S, Ozdemir BC (2019) Gender medicine and oncology: report and consensus of an ESMO workshop. Ann Oncol 30(12):1914–1924. https://doi.org/10.1093/annonc/mdz414
Gabriele L, Buoncervello M, Ascione B, Bellenghi M, Matarrese P, Carè A (2016) The gender perspective in cancer research and therapy: novel insights and on-going hypotheses. Ann Ist Super Sanita 52(2):213–222. https://doi.org/10.4415/ANN_16_02_13
Schmetzer O, Flörcken A (2012) Sex differences in the drug therapy for oncologic diseases. Handb Exp Pharmacol 214:411–442. https://doi.org/10.1007/978-3-642-30726-3_19
Oliver JS, Martin MY, Richardson L, Kim Y, Pisu M (2013) Gender differences in colon cancer treatment. J Womens Health (Larchmt) 22(4):344–351. https://doi.org/10.1089/jwh.2012.3988
Sloan JA, Goldberg RM, Sargent DJ, Vargas-Chanes D, Nair S, Cha SS, Novotny PJ, Poon MA, O’Connell MJ, Loprinzi CL (2002) Women experience greater toxicity with fluorouracil-based chemotherapy for colorectal cancer. J Clin Oncol 20(6):1491–1498. https://doi.org/10.1200/JCO.2002.20.6.1491
van der Geest LG, Portielje JE, Wouters MW, Weijl NI, Tanis BC, Tollenaar RA, Struikmans H, Nortier JW, Netherlands ANHitLRotCCCT (2013) Complicated postoperative recovery increases omission, delay and discontinuation of adjuvant chemotherapy in patients with Stage III colon cancer. Colorectal Dis 15(10):e582-591. https://doi.org/10.1111/codi.12288
Park HC, Shin A, Kim BW, Jung KW, Won YJ, Oh JH, Jeong SY, Yu CS, Lee BH (2013) Data on the characteristics and the survival of korean patients with colorectal cancer from the Korea central cancer registry. Ann Coloproctol 29(4):144–149. https://doi.org/10.3393/ac.2013.29.4.144
Hansen IO, Jess P (2012) Possible better long-term survival in left versus right-sided colon cancer - a systematic review. Dan Med J 59(6):A4444
Pal SK, Hurria A (2010) Impact of age, sex, and comorbidity on cancer therapy and disease progression. J Clin Oncol 28(26):4086–4093. https://doi.org/10.1200/JCO.2009.27.0579
Slattery ML, Potter JD, Curtin K, Edwards S, Ma KN, Anderson K, Schaffer D, Samowitz WS (2001) Estrogens reduce and withdrawal of estrogens increase risk of microsatellite instability-positive colon cancer. Cancer Res 61(1):126–130
West DW, Slattery ML, Robison LM, Schuman KL, Ford MH, Mahoney AW, Lyon JL, Sorensen AW (1989) Dietary intake and colon cancer: sex- and anatomic site-specific associations. Am J Epidemiol 130(5):883–894. https://doi.org/10.1093/oxfordjournals.aje.a115421
Brenner H, Hoffmeister M, Arndt V, Haug U (2007) Gender differences in colorectal cancer: implications for age at initiation of screening. Br J Cancer 96(5):828–831. https://doi.org/10.1038/sj.bjc.6603628
Borugian MJ, Sheps SB, Whittemore AS, Wu AH, Potter JD, Gallagher RP (2002) Carbohydrates and colorectal cancer risk among Chinese in North America. Cancer Epidemiol Biomarkers Prev 11(2):187–193
McMichael AJ, Potter JD (1985) Diet and colon cancer: integration of the descriptive, analytic, and metabolic epidemiology. Natl Cancer Inst Monogr 69:223–228
Tejpar S, Yan P, Piessevaux H, Dietrich D, Brauchli P, Klingbiel D, Fiocca R, Delorenzi M, Bosman F, Roth AD (2018) Clinical and pharmacogenetic determinants of 5-fluorouracyl/leucovorin/irinotecan toxicity: Results of the PETACC-3 trial. Eur J Cancer 99:66–77. https://doi.org/10.1016/j.ejca.2018.05.009
Cristina V, Mahachie J, Mauer M, Buclin T, Van Cutsem E, Roth A, Wagner AD (2018) Association of patient sex with chemotherapy-related toxic effects: a retrospective analysis of the PETACC-3 trial conducted by the EORTC Gastrointestinal Group. JAMA Oncol 4(7):1003–1006. https://doi.org/10.1001/jamaoncol.2018.1080
Wagner AD, Grothey A, Andre T, Dixon JG, Wolmark N, Haller DG, Allegra CJ, de Gramont A, VanCutsem E, Alberts SR, George TJ, O’Connell MJ, Twelves C, Taieb J, Saltz LB, Blanke CD, Francini E, Kerr R, Yothers G, Seitz JF, Marsoni S, Goldberg RM, Shi Q (2021) Sex and adverse events of adjuvant chemotherapy in colon cancer: an analysis of 34 640 patients in the ACCENT Database. J Natl Cancer Inst 113(4):400–407. https://doi.org/10.1093/jnci/djaa124
Ranucci M, Aloisio T, Di Dedda U, Menicanti L, de Vincentiis C, Baryshnikova E, Surgical and Clinical Outcome REsearch (SCORE) Group (2019) Gender-based differences in platelet function and platelet reactivity to P2Y12 inhibitors. PLoS One 14(11):e0225771. https://doi.org/10.1371/journal.pone.0225771
Asai Y, Yamamoto T, Abe Y (2021) Evaluation of the expression profile of antibiotic-induced thrombocytopenia using the Japanese Adverse Drug Event Report Database. Int J Toxicol 40(6):542–550. https://doi.org/10.1177/10915818211048151
Hovan AJ, Williams PM, Stevenson-Moore P, Wahlin YB, Ohrn KE, Elting LS, Spijkervet FK, Brennan MT (2010) Dysgeusia Section OCSG, M.ltinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO). A systematic review of dysgeusia induced by cancer therapies. Support Care Cancer 18(8):1081–1087. https://doi.org/10.1007/s00520-010-0902-1
Palmeira CC, Ashmawi HA, Posso IeP (2011) Sex and pain perception and analgesia. Rev Bras Anestesiol 61(6):814–828. https://doi.org/10.1016/S0034-7094(11)70091-5
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Prevalence of gastro-oesophageal reflux symptoms and the influence of age and sex. Scand J Gastroenterol. 2004 Nov;39(11):1040-5.
Deenen MJ, Cats A, Beijnen JH, Schellens JH (2011) Part 1: background, methodology, and clinical adoption of pharmacogenetics. Oncologist 16(6):811–819. https://doi.org/10.1634/theoncologist.2010-0258
Gamelin E, Delva R, Jacob J, Merrouche Y, Raoul JL, Pezet D, Dorval E, Piot G, Morel A, Boisdron-Celle M (2008) Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: results of a multicenter randomized trial of patients with metastatic colorectal cancer. J Clin Oncol 26(13):2099–2105. https://doi.org/10.1200/JCO.2007.13.3934
Author information
Authors and Affiliations
Contributions
Conceptualization of the study was devised by Silvia De Francia, Maria Valentina Mussa, Silvia Racca, and Libero Ciuffreda; methodology (data collection and curation) was performed by Tiziana Armando, Silvana Storto, Maria Rosaria Caiaffa, Maria Valentina Mussa, Giulia Soave, and Andrea Elio Sprio; formal analysis was performed by Paola Berchialla and Veronica Sciannameo; writing and preparation of the original draft was done by Silvia De Francia, Maria Valentina Mussa, Paola Berchialla, and Sarah Allegra. All the authors have read and agreed on the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Prot. N° 0092030.
Competing interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
De Francia, S., Berchialla, P., Armando, T. et al. Colorectal cancer chemotherapy: can sex-specific disparities impact on drug toxicities?. Eur J Clin Pharmacol 78, 1029–1038 (2022). https://doi.org/10.1007/s00228-022-03298-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03298-y