Abstract
Purpose
In response to a large trial, the World Health Organization broadened their recommendation on tranexamic acid to be used for post-partum hemorrhage. A 2013 French periodic safety update report warned of an abnormally high rate of renal cortical necrosis associated with tranexamic acid and other drugs for severe post-partum hemorrhage. We aimed to identify the reporting incidence of adverse thrombo-embolic events among women in child-bearing age who received tranexamic acid, with a focus on renal vascular and ischemic conditions.
Methods
We analyzed individual case safety reports (ICSRs) on renal vascular and ischemic conditions, pulmonary thrombotic and embolic conditions, and peripheral embolism and thrombosis from the database of the World Health Organization – Uppsala Monitoring Centre (WHO-UMC). ICSRs were restricted to reports including tranexamic acid as a suspected drug, sex reported as female, and reported age between 18 and 44 years. Reporting odds ratios (RORs) and 95% confidence intervals (95% CIs) were calculated by comparing ICSRs on tranexamic acid to all other drugs in VigiBase.
Results
Within 2245 included ICSRs on tranexamic acid, we identified 29 reports of adverse renal vascular and ischemic conditions, 42 reports of pulmonary thrombotic and embolic conditions, and 41 reports of peripheral embolism and thrombosis. RORs were statistically significant by 32.6-fold (32.62, 95% CI: 22.50–47.29), 2.5-fold (2.52, 95% CI: 1.85–3.42), and 2.7-fold (2.67, 95% CI: 1.96–3.64), respectively, when compared to any other drug within VigiBase.
Conclusion
Tranexamic acid might bear an increased risk for renal ischemic adverse drug events in women of child-bearing age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tranexamic acid, an inhibitor of fibrinolysis, was recently recommended by the World Health Organization (WHO) for post-partum hemorrhage [1]. This was an update to the 2012 WHO recommendations where use was restricted to situations of failure of uterotonics or to a birth trauma as a cause of bleeding [2]. The updated recommendations broadening the indication followed the WOMAN (World Maternal Antifibrinolytic) trial [3], which was a large multicenter trial in high-resource as well as in low-resource settings. The trial revealed a significant reduction in hemorrhage-related mortality with early use of tranexamic acid (1 to 3 h) and no increase of adverse drug events.
A recent review of post-partum hemorrhage guidelines from developed countries and organizations around the globe found that the Royal College of Obstetricians and Gynaecologists (RCOG) was the only official obstetric body recommending, in 2017, against the use of tranexamic acid [4]. However, a 2019 RCOG document on maternal collapse now recommends the use of tranexamic acid, which is in line with clinical practice in the UK that shifted to using tranexamic acid [5]. The meta-analysis by Gayet-Ageron and colleagues [3, 6] and the WOMAN trial [3] support the efficacy of tranexamic acid for treating post-partum hemorrhage, while a randomized controlled trial by Sentilhes and colleagues [7] did not find a benefit of prophylactic tranexamic acid after vaginal delivery.
Although the efficacy of tranexamic acid is widely appreciated, less is known about the safety. A meta-analysis on randomized controlled trials (RCTs) concluded that tranexamic acid was not associated with an increased risk of adverse events compared to placebo or no treatment [8]. However, the number of obstetric trials in this analysis was low (6%) and included only 3251 patients. A French periodic safety update report (PSUR) in 2013 warned of an abnormally high rate of unexplained kidney failure after administration of tranexamic acid together with other drugs for severe post-partum hemorrhage [9]. Three years later, another French study reported 18 cases of renal cortical necrosis in women with post-partum hemorrhage who had received tranexamic acid [10]. At 6 months after delivery, none had recovered normal renal function and eight of the 18 patients (44%) were dialysis dependent. Length of exposure to tranexamic acid was the only risk factor which was associated with poorer kidney outcomes—in contrast to other studied variables such as blood loss volume, disseminated intravascular coagulation, hemodynamic instability, and exposition with other nephrotoxins.
In light of the limited evidence, we sought to assess renal ischemic adverse events associated with the use of tranexamic acid for post-partum hemorrhage reported to the World Health Organization – Uppsala Monitoring Centre (WHO-UMC) database on spontaneous reports of adverse drug events. We aimed to identify the reporting incidence of adverse thrombo-embolic events among women in child-bearing age who received tranexamic acid with a focus on renal vascular and ischemic conditions.
Methods
Database and study population
Data on individual case safety reports (ICSRs) were retrieved from WHO-UMC VigiBase. VigiBase contains spontaneous reports on adverse drug events sent by member countries of the WHO Programme for International Drug Monitoring. The original reports, submitted by clinicians, manufacturers, and patients to national pharmacovigilance centers, are amended with the standard terminology MedDRA® for the reported adverse events [11]. The included drugs are given their WHO Anatomical Therapeutical Chemical (ATC) classification [12]. Aggregated data on ICSRs available through the interface VigiLyze contain variables on identifiers, report properties, reporter qualification, patient age and sex, reported adverse events, reported outcomes, and reported drug regimen (substance, dose, regimen, route, starting, and stopping date). Causality and clinical assessments are handled differently by the various national pharmacovigilance centers.
All ICSRs with tranexamic acid (ATC: B02AA02) reported as a suspected, concomitant, or interacting drug were identified among those with sex reported as female. ICSRs were then restricted to reports describing tranexamic acid as suspected drug with patients’ age reported between 18 and 44 years. ICSRs with missing sex or age were excluded.
Adverse events of interest were defined as the preferred terms included within the MedDRA® high-level terms “renal vascular and ischemic conditions,” “pulmonary thrombotic and embolic conditions,” and “peripheral embolism and thrombosis.” Number of events was defined as the number of unique ICSRs, as identified by the WHO-UMC report ID.
Statistical analysis
Demographic characteristics of the ICSRs were summarized using means and standard deviations and counts and proportions where appropriate, stratified by the three terms of interest. For renal vascular and ischemic conditions, we additionally investigated dosing of tranexamic acid and outcomes of reported events.
As a measure of disproportionality within the database, reporting odds ratios (RORs) with corresponding 95% confidence intervals (95% CIs) were calculated [13]. RORs compare the number of reports mentioning the drug of interest and the adverse drug event of interest to the reports for the outcome of interest among all other drugs in the database [14]. For this study, the ratio of reports on “renal vascular and ischemic conditions,” “pulmonary thrombotic and embolic conditions,” and “peripheral embolism and thrombosis” with tranexamic acid to with any other drug built the nominator, while the ratio of reports on any other event with tranexamic acid to with any other drug built the denominator. All analyses were performed in RStudio, version 1.2.5019 or later [15], running R, version 3.6.0 or later [16], and the packages data.table [17], dplyr [18], tidyr [19], and lubridate [20].
Results
Pharmacovigilance database
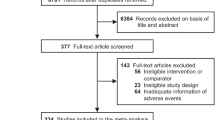
Data on tranexamic acid were extracted on October 21, 2019. ICSRs on tranexamic acid and female sex amounted to 5328 ICSRs from first database entry (June 30, 1972) until date retrieved (latest: October 19, 2019). The dataset was reduced to 5261 ICSRs by restriction to reports describing tranexamic acid as suspected drug and, finally, to 2245 ICSRs by restriction to reported ages 18 to 44 years. The original dataset of 5328 ICSRs contained 328 missing values on age (6.2%), which were excluded.
Table 1 summarizes report characteristics stratified by the three terms of interest. We identified 29 reports of adverse renal vascular and ischemic conditions (1.3%), 42 reports of pulmonary thrombotic and embolic conditions (1.9%), and 41 reports of peripheral embolism and thrombosis (1.8%). Overall, the reported mean age was 33.4 years (standard deviation: 7.3). Mean age was highest for peripheral embolism and thrombosis (37.3 ± 5.6 years) and lowest for renal vascular and ischemic conditions (32.3 ± 5.0 years). Year of first database entry was different for all three terms of interest and ranged from 1980 for peripheral embolism and thrombosis to 2014 for renal vascular and ischemic conditions. Reported mortality was highest for pulmonary thrombotic and embolic conditions. Figure 1 shows the top three of reported concomitant medication and reported reactions, stratified by all and the three events of interest. Reported medication regimen was different for renal vascular and ischemic conditions, pulmonary thrombotic and embolic events, and peripheral embolism and thrombosis, respectively.
Top three reported concomitant medication and reported reactions within individual case safety reports (ICSRs) on tranexamic acid in VigiBase, stratified by all and the events of interest. ICSRs were filtered for tranexamic acid reported as suspected drug, female sex, and reported age 18 to 44 years. Numbers may not add up to 100%: An ICSR may report more than one concomitant medication
Among the 29 reports on renal vascular and ischemic conditions, dosing of tranexamic acid was available for 17 reports (59%): in one ICSR 500 mg, in eight ICSRs 1 g, in five ICSRs 2 g, in two ICSRs 3 g, and in one ICSR 5 g were mentioned, respectively. Twenty-eight (97%) ICSRs reported patient outcome: One patient died, three did not recover, five did recover with a sequela, three were still recovering at the time of report, five recovered, and 11 had an unknown outcome.
Statistical analysis
The results from the disproportionality analyses are presented in Table 2. Calculations showed a statistically significant signal for outcomes among users of tranexamic acid compared to any other drug in the database. A 32.6-fold increase in odds of reporting for renal vascular and ischemic conditions (ROR: 32.62, 95% CI: 22.50–47.29), a 2.5-fold increase for pulmonary thrombotic and embolic conditions (ROR: 2.52, 95% CI: 1.85–3.42), and a 2.7-fold increase for peripheral embolism and thrombosis (ROR: 2.52, 95% CI: 1.85–3.42) were observed.
Discussion
In this analysis of spontaneous reports of adverse events, we identified that thrombo-embolic events accounted for approximately 5% of all reported outcomes for tranexamic acid among women of child-bearing age (18 to 44 years). Within 2245 included ICSRs on tranexamic acid, we identified 29 (1.3%) reports of adverse renal vascular and ischemic conditions, 42 (1.9%) reports of pulmonary thrombotic and embolic events, and 41 (1.8%) reports of peripheral embolism and thrombosis. Additionally, a signal of disproportionate reporting for renal vascular and ischemic conditions was observed with a reported median dose of 1 g of tranexamic acid.
We purposefully selected thrombo-embolic events as additional events of interest, alongside renal vascular and ischemic conditions, to put the calculated RORs into perspective. Because of its mechanism of action as a competitive inhibitor of fibrinolysis [21], tranexamic acid may be expected to increase the rates of thrombo-embolic events. In our disproportionality analysis, we observed increased odds of reporting for peripheral embolism and thrombosis and pulmonary thrombotic and embolic conditions of 2.7-fold (ROR: 2.67, 95% CI: 1.96–3.64) and 2.5-fold (ROR: 2.52, 95% CI: 1.85–3.42), respectively. A 32.6-fold (ROR: 32.62, 95% CI: 22.50–47.29) increase in odds of reporting for renal vascular and ischemic conditions, hence, marks an additional disproportionality.
Renal cortical necrosis is an ischemic destruction of the renal cortex caused by reduced arterial perfusion due to vascular spasm, microvascular injury, or intravascular coagulation [22, 23]. With its antifibrinolytic properties, tranexamic acid may harm the kidneys by favoring the formation of blood clots affecting kidney vessels and causing cortical necrosis. Hemorrhages and shock are characterized by hypovolemia and hypotension, which are risk factors for prerenal etiologies of kidney failure by themselves. The combination of fibrinolysis inhibition, hypovolemia, fibrinogen concentrates, and pregnancy-related coagulopathy [24] potentially has an adverse impact on the renal endothelium. Pregnant women and post-partum women are generally in a hypercoagulable state [25] and at an increased risk for thrombo-embolic events altogether [26, 27] due to elevated levels of factors VII, X, VIII, fibrinogen, and von Willebrand; an increase in prothrombin fragments and thrombin-antithrombin complexes; a reduction in protein S activity; and an acquired activated protein C resistance [28]. In our data, sixteen ICSRs (55%) additionally received sulprostone (Fig. 1), for which the product information labels adverse effects on renal function [29]. The concomitant use of the prostaglandin E2 analogue sulprostone may act as a mediating factor as it would impair the renal elimination of tranexamic acid [21] and increase tranexamic acid exposure.
The cases of renal corticosis as reported by Frimat et al. were observed with doses from 2 to 11 g in patients with post-partum hemorrhage (median 5 g) [10]. A recent RCT administered 1 g of tranexamic acid prophylactically to 1918 women, whereof 90% did not have post-partum hemorrhage [7]. There were no reported untoward thrombo-embolic events, including renal events or failure, potentially indicating dose-dependent effects and an interplay of disease and drug effects. Currently, doses of up to 2 g are recommended for the off-label treatment of post-partum hemorrhage [4, 21]. In our analysis, the median dose was 1 g, and 14 of the 17 ICSRs, that reported kidney damage and dosing of tranexamic acid, mentioned doses lower or equal to 2 g. We, therefore, feel that clinicians should be aware of renal complications even at low doses of tranexamic acid.
Limitations
Analyses of pharmacovigilance data are prone to inherent limitations and need to be interpreted with care. Firstly, the calculated ORs are directly influenced by the number of reports sent to the database [14]. Health care professionals may be biased by current publications and discussions. Secondly, the quality of individual reports and clinical details provided may vary [30]. The reporters are primarily responsible for entering temporal relationships and initial assessments of causality; governance by national health authorities should, in theory, assure quality. Clinical details (e.g., lab values, comorbidities) are, if provided at all, restricted to the original reports and are not available through VigiBase. Hence, renal insufficiency was not available for our assessment, a predisposing factor for kidney failure and an important determinant for the renally excreted tranexamic acid exposure [31]. Thirdly, aggregated data on ICSRs does not include information on concomitant diagnoses, hindering assessments of potential confounding by diseases. Fourthly, the used ICSRs and numbers may have described incidents where the drugs were not used in obstetrics or for post-partum hemorrhage (e.g., menorrhagia, postoperative hemorrhage). Contrary to adverse reactions, indications are not amended by codes and are, hence, not possible to effectively process in VigiBase. We aimed to generate relevance for the obstetric population by restricting the search to female patients between 18 and 44 years of age. However, different indications may have been present in our final dataset. In culmination, our results should only be used as one singular piece of evidence and a safety signal to raise awareness. Disproportionality measures of spontaneous reports are not suited for causal inferences [32].
Conclusion
We hereby report a disproportionality in reporting for tranexamic acid and renal vascular and ischemic conditions (e.g., renal cortical necrosis) in women aged 18 to 44 years. There is a need for observational studies investigating the causal relationship between tranexamic acid and rare adverse drug reactions. Until then, the benefits of tranexamic acid in acute situations such as post-partum hemorrhage should be weighed against its potential risks. This benefit-risk ratio may change with delays in treatment and may be different for prophylactic use.
Data availability
The data that support the findings of this study are available from WHO-UMC but restrictions apply to the availability of these data, which were used under special access for the current study, and so are not publicly available.
References
Vogel JP, Oladapo OT, Dowswell T, Gülmezoglu AM (2018) Updated WHO recommendation on intravenous tranexamic acid for the treatment of post-partum haemorrhage. Lancet Glob Health 6:e18–e19. https://doi.org/10.1016/S2214-109X(17)30428-X
World Health Organization WHO. (2012) WHO recommendations for the prevention and treatment of postpartum haemorrhage. www.who.int.
Shakur H, Roberts I, Fawole B et al (2017) Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet 389:2105–2116. https://doi.org/10.1016/S0140-6736(17)30638-4
Shaylor R, Weiniger CF, Austin N et al (2017) National and international guidelines for patient blood management in obstetrics: a qualitative review. Anesth Analg 124:216–232. https://doi.org/10.1213/ANE.0000000000001473
O’Sullivan J, Mansfield R, Talbot R, Cairns AE (2018) Major obstetric haemorrhage of 2000 ml or greater: a clinical audit. J Obstet Gynaecol 38:1065–1072. https://doi.org/10.1080/01443615.2018.1449820
Gayet-Ageron A, Prieto-Merino D, Ker K et al (2018) Effect of treatment delay on the effectiveness and safety of antifibrinolytics in acute severe haemorrhage: a meta-analysis of individual patient-level data from 40 138 bleeding patients. Lancet 391:125–132. https://doi.org/10.1016/S0140-6736(17)32455-8
Sentilhes L, Winer N, Azria E et al (2018) Tranexamic acid for the prevention of blood loss after vaginal delivery. N Engl J Med 379:731–742. https://doi.org/10.1056/NEJMoa1800942
Yates J, Perelman I, Khair S et al (2019) Exclusion criteria and adverse events in perioperative trials of tranexamic acid: a systematic review and meta-analysis. Transfusion (Paris) 59:806–824
Bouet P-E, Ruiz V, Legendre G et al (2015) High-dose tranexamic acid for treating postpartum haemorrhage after vaginal delivery. BJA Br J Anaesth 114:339–341. https://doi.org/10.1093/bja/aeu468
Frimat M, Decambron M, Lebas C et al (2016) Renal cortical necrosis in postpartum hemorrhage: a case series. Am J Kidney Dis 68:50–57. https://doi.org/10.1053/j.ajkd.2015.11.022
International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. (2019) MedDRA®: Medical Dictionary for Regulatory Activities terminology (22nd ed.). https://www.meddra.org/
Uppsala Monitoring Centre (2019) UMC | Know more about VigiBase. In: UMC Know More VigiBase. https://www.who-umc.org/vigibase/vigibase/know-more-about-vigibase/. Accessed 23 Apr 2019
van Puijenbroek EP, Bate A, Leufkens HGM et al (2002) A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol Drug Saf 11:3–10. https://doi.org/10.1002/pds.668
Rothman KJ, Lanes S, Sacks ST (2004) The reporting odds ratio and its advantages over the proportional reporting ratio. Pharmacoepidemiol Drug Saf 13:519–523. https://doi.org/10.1002/pds.1001
RStudio Team (2019) RStudio: integrated development for R. RStudio, Boston
Core Team R (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Dowle M, Srinivasan A, Gorecki J, et al (2019) data.table: extension of “data.frame”
Wickham H, François R, Henry L, et al (2019) dplyr: a grammar of data manipulation
Wickham H, Henry L (2019) RStudio tidyr: Tidy Messy Data
Spinu V, Grolemund G, Wickham H, et al (2018) lubridate: make dealing with dates a little easier
Lexicomp (2018) Tranexamic acid: drug information
Fakhouri F, Vercel C, Frémeaux-Bacchi V (2012) Obstetric nephrology: AKI and thrombotic microangiopathies in pregnancy. Clin J Am Soc Nephrol CJASN 7:2100–2106. https://doi.org/10.2215/CJN.13121211
Prakash J, Vohra R, Wani IA et al (2007) Decreasing incidence of renal cortical necrosis in patients with acute renal failure in developing countries: a single-centre experience of 22 years from Eastern India. Nephrol Dial Transplant 22:1213–1217. https://doi.org/10.1093/ndt/gfl761
Hellgren M (2003) Hemostasis during normal pregnancy and puerperium. Semin Thromb Hemost 29:125–130. https://doi.org/10.1055/s-2003-38897
Marik PE, Plante LA (2008) Venous thromboembolic disease and pregnancy. N Engl J Med 359:2025–2033. https://doi.org/10.1056/NEJMra0707993
Heit JA, Kobbervig CE, James AH et al (2005) Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med 143(10):697–706
Pomp ER, Lenselink AM, Rosendaal FR, Doggen CJM (2008) Pregnancy, the postpartum period and prothrombotic defects: risk of venous thrombosis in the MEGA study. J Thromb Haemost 6:632–637. https://doi.org/10.1111/j.1538-7836.2008.02921.x
Brenner B (2004) Haemostatic changes in pregnancy. Thromb Res 114:409–414. https://doi.org/10.1016/j.thromres.2004.08.004
Bayer Switzerland (2018) Swiss product information Nalador® (Sulprostone)
Caster O, Juhlin K, Watson S, Norén GN (2014) Improved statistical signal detection in pharmacovigilance by combining multiple strength-of-evidence aspects in vigiRank. Drug Saf 37:617–628. https://doi.org/10.1007/s40264-014-0204-5
Andersson L, Eriksson O, Hedlund P-O et al (1978) Special considerations with regard to the dosage of tranexamic acid in patients with chronic renal diseases. Urol Res 6:83–88. https://doi.org/10.1007/BF00255578
Beau-Lejdstrom R, Crook S, Spanu A et al (2019) Adverse drug reaction risk measures: a comparison of estimates from drug surveillance and randomised trials. Pharm Med 33:331–339. https://doi.org/10.1007/s40290-019-00287-y
Acknowledgments
MedDRA® trademark is owned by IFPMA on behalf of ICH. The information presented here does not represent the opinion of the UMC or the WHO.
Funding
Open Access funding provided by Swiss Federal Institute of Technology Zurich. The study was enabled by funds from the ETH Zurich; no external sources of funding were used to assist in the conduct of this study or the preparation of this article.
Author information
Authors and Affiliations
Contributions
Dominik Stämpfli: conceptualization, methodology, formal analysis, visualization, writing—original draft. Stefan Weiler: methodology, data curation, writing—review & editing. Carolyn F Weiniger: writing—review & editing. Andrea M Burden: conceptualization, methodology, supervision, writing—review & editing. Michael Heesen: conceptualization, supervision, writing—original draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest relevant to the content of this study. SW is a member of the Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA). The views expressed in this article are the personal views of the authors and may not be understood or quoted as being made on behalf of or reflecting the position of the European Medicines Agency or one of its committees or working parties.
The authors declare that they performed their research in compliance with the caveat document “Statement of reservations, limitations and conditions relating to data released from VigiBase, the WHO global database of individual case safety reports (ICSRs)” by the WHO Collaborating Centre for International Drug Monitoring, Uppsala Monitoring Centre, published 2018-11-20 on www.who-umc.org.
Ethics approval
This was an observational study with anonymous pharmacovigilance data.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
The unformatted code used during the current study is available from the corresponding author on reasonable request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stämpfli, D., Weiler, S., Weiniger, C.F. et al. Renal ischemic adverse drug events related to tranexamic acid in women of child-bearing age: an analysis of pharmacovigilance data. Eur J Clin Pharmacol 77, 913–919 (2021). https://doi.org/10.1007/s00228-020-03064-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-03064-y