Abstract
Purpose
No study has been evaluated pharmacokinetic (PK) and pharmacodynamic (PD) properties of β-lactam antibiotics in patients with acute kidney injury (AKI), not requiring renal replacement therapy (RRT). We evaluated the time that plasma concentrations remain above four times the MIC (ft > 4MIC) and PK parameters of meropenem in this population.
Methods
In this prospective, randomized clinical trial (RCT), all patients received standard dose (3 g daily) of meropenem for 48 h, then randomly allocated in standard or adjusted groups. The standard group received meropenem without dose adjustment. In the adjusted group, the meropenem dose was adjusted based on the Cockcroft-Gault(C-G) equation. Meropenem concentrations were measured at the peak and trough times on the 2nd and 5th days of the study.
Results
On the 2nd day of the study, 3 out of 10 (30%) of patients attained the PD target (≥ 80%ft > 4MIC). In the 5th day of the study, the PD target was attained in 2 out of 10 (20%) and 1 out of 5 (20%) of patients who received standard and adjusted doses of meropenem, respectively (p = 1). In all samples, increased volume of distribution (Vd) (median; IQR) (46.04; 23.06–103.18 L), terminal half-life (T1/2) (4.51; 2.67–8.88 h) and decreased clearance (6.52; 4.43–10.16 L/h) have been shown.
Conclusion
In critically ill patients with AKI, who not receive RRT, standard doses, and adjusted according to renal function of meropenem failed to achieve PD target of ≥ 80%ft > 4MIC. Higher doses are required for this target.
Retrospectively registered
The study protocol with registered retrospectively and approved on January 19, 2019, with the number of IRCT20160412027346N5.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is one of the common problems in critically ill patients, especially subjects with sepsis [1]. In this phenomenon, pathological factors alter pharmacokinetic (PK) and pharmacodynamic (PD) properties of medications, including antimicrobial agents; therefore, antibiotics’ dosing can be complicated in patients with AKI [2]. The main focus of studies on dosing of antimicrobials in patients with AKI was in critically ill patients with sepsis and AKI, who were receiving renal replacement therapy (RRT); however, specific PK/PD data about antibiotics in patients with AKI, not requiring RRT, are rare [2, 3]. Also, there is no specific guideline in antimicrobial dosing in patients with AKI, and recommended dose adjustment for antibiotics in patients with impaired renal function is derived from studies in chronic kidney injury (CKD). This problem is too important in sepsis-related AKI, as the main cornerstone of treatment is the appropriate selection and dosing of antimicrobials, and it is proven that inappropriate dosing of antibiotics could significantly increase the sepsis-related mortality and treatment complications [3].
In 2010, the organization of Kidney Disease: Improving Global Outcomes (KDIGO) held a conference to investigate the drug dosage approach in patients with renal impairment. The consensus about dosing adjustment of hydrophilic antibiotics, including β-lactam in AKI, is the administration of high loading doses and suggested that the maintenance dose of antibiotics should be initiated at normal or near-normal dosage regimens [4]. Despite this recommendation, to the best of our knowledge, no study has been evaluated PK/PD properties of β-lactam antibiotics with recommended doses in patients with AKI, not requiring RRT.
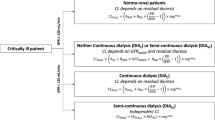
Meropenem is a broad-spectrum β-lactam antibiotic, which is frequently used for empiric treatment of nosocomial infections in critically ill patients [5]. The PD activity of meropenem is time-dependent. Minimum plasma concentrations (Cmin) higher than the minimum inhibitory concentration (MIC) for an adequate percentage of time in a dosing interval (%ft > MIC), must be maintained for bactericidal efficacy [6, 7], and prolonged infusions rather than increasing the dose, could optimize the effect of this antibiotic [8,9,10]. Meropenem undergoes extensive renal elimination, with a clearance (CL) of approximately 10–12 L/h in most studies [6, 8], and in subjects with normal renal function, the elimination half-life (T1/2) of meropenem is approximately 1 h. The plasma protein binding of meropenem is approximately 2% and the volume of distribution (Vd) at steady-state is around 15–20 L[11]. A 3-h infusion of 1 g of meropenem in healthy persons produce a mean peak plasma concentration (Cmax) of 25 μg/mL[11]. Considering these PK/PD characteristics in the dosing of antimicrobials could maximize efficacy, minimize the antimicrobial resistance, and concentration-related adverse effects [3].
The primary objective of the current study was the evaluation of the time that plasma concentrations remain above four times the MIC (ft > 4MIC) as an index for meropenem efficacy in critically ill patients with AKI, not receiving RRT, with two dosing regimens, adjusted based on calculated creatinine clearance (CrCl) by the Cockcroft-Gault (C-G) formula, compared to the standard dosing regimen. As a secondary goal, we evaluated the PK parameters of meropenem is this setting.
Materials and methods
Settings
The present prospective, randomized clinical trial (RCT), was conducted in a 30-bed medical-surgical intensive care unit (ICU) of Imam Hossein Medical Center, affiliated with Shahid Beheshti University of Medical Sciences (SBMU) in Tehran, Iran, from July 2018 to August 2019. This study has been approved by the Institutional Review Boards of the Ethics Committee of SBMU (IR.SBMU.PHNM.1397.38). Also, the study protocol was registered, reviewed, and approved by the Iranian Registry of Clinical Trials (IRCT), with the registry number of IRCT20160412027346N5.
Study population
All patients older than 18 years, who developed AKI based on Acute Kidney Network (AKIN) and/or Risk, Injury, Failure, Loss, End-stage renal disease (RIFLE) criteria [12], and treated with standard dose of meropenem((1 gram (g) every 8 h (3 g daily)) based on the physician in charge decision, were included in the study. Patients with one of the following criteria were excluded: CKD, RRT, pregnancy, lactation, and receiving an adjusted dose of meropenem before recruitment.
Interventions
All patients admitted to the ICU were evaluated according to the AKIN and RIFLE criteria on the first day of admission. All patients who were included in the study received standard dose of meropenem (1 g every 8 h (3 g daily)), based on the diagnosis (empiric or culture-based) for 48 h. Each dose of meropenem was infused over 4 h. After 48 h (classified as the early phase), blood samples were obtained at the following times: 1 h after the end of infusion (peak concentration (Cpeak)), and 30 min before the start of the next dose (trough concentration (Ctrough)) [13]. Then, patients were enrolled in two treatment groups: standard or adjusted. The standard group received meropenem without dose adjustment, but in another group adjusted doses were administered to the patients based on calculated CrCl by the C-G equation as follows: CrCl ≥ 50 ml/min: no dosage adjustment, CrCl: 25–50 ml/min: recommended dose every 12 h, CrCl: 10–25 ml/min: one-half recommended dose every 12 h, CrCl < 10 ml/min: one-half recommended dose every 24 h [14]. Sampling was repeated on the fifth day after the administration of meropenem (classified as the late phase) for the measurement of Cpeak and Ctrough. Blood samples were immediately centrifuged for 15 min at 4000g, and serum was stored at − 80 °C for later analysis.
For all patients, the following variables were recorded: age, sex, ideal body weight (IBW), baseline serum creatinine (Scr), stage of AKIN and RIFLE criteria in the recruitment day, Scr and estimated CrCl by the C-G equation in the recruitment day, and duration of antibiotic therapy.
Meropenem assay
Serum concentrations were determined by high-performance liquid chromatography (HPLC) with an ultraviolet (UV) detector. Then, 950 μl of plasma was precipitated with 1000-μl acetonitrile, containing 50 μl of acetaminophen as the internal standard. After vortexing and centrifugation at 4000g for 10 min, 20 μl was injected into the HPLC-UV system. The mobile phase consisted of water-ammonium acetate-acetonitrile (60%, 31%, 9%) at pH 4 with an injection rate of 1 ml/min. The separation was performed on an analytical C18 column (250 mm × 4.6 mm with 5-μm spherical particles). The UV detection was at 298 nm. The calibration curve was constructed by linear regression of analyte-internal standard area ratios; the method was validated over the concentration range of 2.5–80 μg/mL. The limit of quantitation (LOQ) was 1.25 μg/mL [15].
Definition
CrCl calculated according to the Cockcroft-Gault formula as:
We used IBW for calculating CrCl with the C-G formula. Thus, participants’ heights were estimated (for those without this record), based on the length of the ulna (Malnutrition Universal Screening Tool (MUST) equation) [16].
The PK parameters for plasma meropenem concentration were calculated according to Eqs. 1 to 5:
“CL” is the clearance of meropenem, “K” is the elimination rate constant, “Vd” is the volume of distribution, and “T1/2” is terminal half-life. Cpeak and Ctrough are the concentrations measured at the 1 h after the end of infusion, and 30 min before the start of the next infusion, and “t” is the time interval between the measurements. Css ave is the average steady-state concentrations of meropenem and “Ƭ” is the dosing interval [13].
PD end-point
In this study, the efficacy of meropenem therapy was assessed by calculating the time above four times the target MIC (ft > 4MIC). The ft > 4MIC was calculated using series of pharmacokinetic formulas in appendix 1. The optimal goal of ft was considered ≥ 80% for meropenem in Gram-negative bacterial infections [17]. In our study, measured concentrations were compared to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) of susceptible breakpoints for the Gram-negative organism, 2 μg/mL for meropenem.
Sample size
The sample size of the study was calculated with Minitab software using the sample size for 2 sample t test function considering type I error of 0.05, power of 0.8, ft > 4MIC in adjusted group 58.83% ± 21.2% [7] and in standard group 88%. The sample size was calculated as 10 patients in each group.
Statistical analysis
All statistical analyses were performed, using SPSS for Windows (Version 21.0; SPSS Inc., Chicago, IL, USA). Quantitative data were tested for normality of distributions by the Shapiro–Wilk test, and then compared by unpaired student’s t test and Mann–Whitney U test for normal and nonnormal data, respectively. Qualitative data were analyzed by the chi squared test, and a P value of < 0.05 was considered significant.
Baseline characteristics and PK/PD data are presented as mean ±standard deviation (SD) or median (interquartile range (IQR)) for normal and nonnormal distribution, respectively, and range (Min–Max) based on the parameters. A Spearman correlation coefficient was computed to assess the relationship between variables.
Results
Baseline characteristics
During the 13-month of the study period, 1334 patients were admitted to the ICU, 171 patients suffered from AKI and 43 patients recruited, and finally, 16 patients (7 and 9 in standard and adjusted arms of the study) completed the study. Details are shown in Fig. 1. There was no statistically significant difference between the two groups in all measured baseline characteristics and parameters related to renal function. The results are shown in Tables 1 and 2.
At total, we obtained 25 paired samples (Cpeak and Ctrough); 10 and 15 pairs in the early and late phases of the study, respectively.
Pharmacokinetic/pharmacodynamic data
The mean ± SD or median (IQR), and the range of meropenem’s PK parameters for two groups in the early and late phases of meropenem treatment are shown in Table 3. In a comparison of PK parameters between the two groups, there were no statistically significant differences in all measured PK parameters.
The mean ± SD of the dose and ft > 4MIC of meropenem in the late phase was 3 g/day vs 2.17 ± 0.94 g/day (t (8) = 2.67, p = 0.028) and 54.81 ± 27.24 % vs 54.64 ± 27.19 % (t (13) = 0.011, p = 0.991) in standard and adjusted group.
In all 25 paired samples, CrCl based on the C-G was (median 42.59 ml/min; IQR 28.12–59.44 ml/min), ft > 4MIC was (median 61.06%; IQR 41.49–76.11%), also PK parameters were as follows: Cpeak (median 19.32 μg/mL; IQR 14.91–31.39 μg/mL), Ctrough (median 11.02 μg/mL; IQR 7.13–17.23 μg/mL), CL of meropenem (median 6.52 L/h; IQR 4.33–10.16 L/h), K (median 0.0025 min−1 ; IQR 0.0013–0.0043 min−1), Vd (median 46.04 L; IQR 23.06–103.18 L), T 1/2 (median 4.51 h; IQR 2.67–8.88 h).
Meropenem plasma concentrations
All measured concentrations (Cpeak and Ctrough) based on the dose and CrCl calculated by the C-G formula are shown in Fig. 2. The large variety of concentrations was seen in patients with different CrCl in a similar dose of meropenem. Table 4 shows the meropenem concentrations in each dose at the early and late phases of administration, regardless of the groups.
Also, Fig. 3 shows the mean meropenem concentrations for two groups in the two phases of study.
In the early phase, all patients were treated with 3-g meropenem daily, and there were not statistically significant differences between the mean concentrations in the adjusted and standard groups (Cpeak: 33.02 ± 19.75 μg/mL vs 21.11 ± 12.31 μg/mL (p = 0.319) and Ctrough: 17.27 ± 13.78 μg/mL vs 12.36 ± 5.50 μg/mL (p = 0.670) in adjusted and standard arms of the study respectively). Also the mean CrCl was not statistically different between two arms of the study (35.09 ± 17.66 ml/min vs 53.02 ± 48.28 ml/min (p = 1)).
In the late phase, although the mean dose of meropenem in the adjusted group was lower than the standard group (2.17 ± 0.94 g vs 3 g (p = 0.028)), the mean concentrations were not statistically significant differences (Cpeak: 20.68 ± 7.28 μg/mL vs 19.40 ± 11.31 μg/mL (p = 0.793) and Ctrough: 12.29 ± 6.34 μg/mL vs 11.10 ± 7.63 μg/mL (p = 0.746) in adjusted and standard arms of the study, respectively). The mean CrCl was not statistically different between two groups (52.22 ± 28.74 ml/min vs 54.39 ± 36.09 ml/min (p = 0.899)).
Meropenem concentrations and renal function
We evaluated the correlation of Ctrough with measured and calculated predictors of renal function, including Scr and CrCl calculated with C-G in patients who treated with 3 g daily of meropenem in the current study .We could not find significant correlation between Ctrough with Scr (r = 0.114, n = 20, p = 0.632). However, the correlation between Ctrough and calculated CrCl, using the C-G formula was statistically significant (r = − 0.484, n = 20, p = 0.031).
Also, we assessed the relationship between the clearance of meropenem with C-G in this subgroup. There was a significant correlation between two variables (r = 0.453, n = 20, p = 0.047).
PD end-point
In the early phase, 3 out of 10 (30%) patients attained the desired PD target, and one patient achieved 100%ft > 4MIC. In the late phase, the desired PD target was attained in 2 out of 10 (20%) and 1 out of 5 (20%) of patients who received standard and adjusted doses of meropenem, respectively (x2(1, N = 15) = 0.000, p = 1). One patient that received a standard dose (3 g daily) attained 100%ft > 4MIC. We reported the PD target in each dose at two phases of the study, regardless of the groups, in Table 4.
Discussion
The main results of the present study were (i) increase of Vd and T1/2 and decrease of clearance of meropenem, as shown in critically ill patients with AKI, who did not receive RRT (ii) plasma concentrations varied between patients with different CrCl in a similar dose of meropenem (iii) fail to reach the PD parameter of ≥ 80%ft > 4MIC in 75 and 80% of patients who received standard and adjusted dose (iv) significant correlation between calculated CrCl by the C-G equation with plasma concentration and clearance of meropenem.
PK/PD properties of antibiotics in critically ill patients, especially in AKI conditions, were different in comparison with healthy volunteers and CKD patients; therefore, approaches to antimicrobial dose adjustment in patients with AKI are controversial [3]. In critically ill patients with sepsis, several factors such as vasoplegia and capillary leak, administration of large volume of fluid and blood can lead to increases in Vd and proportionally prolonged the T1/2 [18]. The Vd of meropenem in healthy volunteers is 15–20 L [11], and in the CKD patients, moderate to severe renal impairment without receiving RRT (CrCl: 6.1–17.1 ml/min), is 19.65–26.71 L [19]. Also, several studies in the critically ill patients have shown that Vd increased (21.7–34.4 L) [18, 20, 21], and the results of our study corroborate the finding of these studies, indicating that Vd increased in critically ill patients with AKI (median 46.04 L; IQR 23.06–103.18 L). The T1/2 reported in CKD patients was 4–5-fold higher than those obtained in healthy volunteers (4.59–5.73 h vs 1 h) [19] and T1/2 is 2.22–2.52 h in critically ill patients [9, 20, 21]. T1/2 reported in our study was prolonged, compared to the healthy volunteers (median 4.51 h; IQR 2.67–8.88 h).
Several studies in septic ICU patients reported high clearance of antibiotics due to hyperdynamic conditions and as a consequence of augmented renal perfusion, following aggressive fluid load and use of inotropic therapy [3, 18, 22]. Nowadays, this phenomenon named augmented renal clearance (ARC), and it is a reason for the increase of clearance and low concentrations of antimicrobial agents in critically ill patients with normal Scr [22].
Jaruratanasirikul et al. [21] evaluated the PK parameters of meropenem in the early phase of severe sepsis and septic shock in ICU patients without a history of CKD, and showed that clearance of meropenem was lower than the values obtained from healthy volunteers (7.82 L/h vs. 12.97 ± 0.18 L/h) [8, 21]. They concluded that renal clearance may be decreased with organ dysfunctions, which can occur with severe sepsis and septic shock [21]. Consistent with the noted study, the clearance of meropenem was lower in comparison with healthy volunteers in our study (median 6.52 L/h; IQR 4.33–10.16 L/h). The clearance of meropenem in the moderate to severe CKD patients was 2.52–4.62 L/h [19].
The observed significant and positive correlation between the clearance of meropenem and C-G, and significant and the negative correlation of meropenem serum concentration with C-G, can prove the relationship between renal function and clearance of drugs [19, 20]. This is also consistent with evidence from an observational study conducted by Petersson et al. [22], showing that measured CrCl is better than Scr in predicting serum concentration of meropenem.
The study population is the most significant difference in our study compared with other studies about meropenem PK/PD parameters in critically ill patients. In other studies, AKI patients specifically are not the target population or are conducted in AKI patients receiving RRT, or these studies excluded the patients with renal impairment [9, 21, 22], but what was special about our study was the critically ill AKI population, not receiving RRT.
The threshold of PD target for maximal β-lactam activity is still controversial. PD targets like concentration above four times of MIC for at least 40% dosing interval (40%ft > 4MIC) have been suggested [7, 20, 23]. According to this target, in the early phase, with standard dosing of meropenem, all patients attained target and in the late phase, 33% of patients failed to achieve the target, whereas two patients received a standard dose and three patients received an adjusted dose of meropenem. Clinical studies in critically ill patients with severe sepsis and septic shock suggested to maximize the effect of β-lactam antibiotics, it may be necessary to maintain the concentration four times the MIC for the entire dosing interval [17], therefore we considered the ≥ 80%ft > MIC as optimal target attainment for meropenem in Gram-negative bacterial infections, so 75 and 80% of patients who received standard and adjusted dose fail to receive this goal.
There are no approved dosage regimen modification guidelines in AKI patients, as described for use in CKD patients. The reviewed literature, according to the studies of the PK/PD of antibiotics in critically ill patients, proposed that as the Vd of the antimicrobial drugs is increased, the standard nonAKI doses should be used in the first 24–48 h of initiation of the therapy [3, 4]. As mentioned in the systematic review by Blot and colleagues [3] in the first 24–48 h of therapy, the concentrations of time-dependent antibiotics in critically ill patients with increased Vd will be lower than in patients with a normal Vd and suggested after that time, dose reduction should occur according to the renally adjusted doses [3]. Also, the KDIGO consensus recommended administration of high loading doses and the maintenance dose of antibiotics should be initiated at normal or near-normal dosage regimens [4].
Consistent with the mentioned literature, we recommend, initial doses of meropenem do not require adjustment in septic critically ill patients with AKI, not receiving RRT, for the first 48 h. It also suggested that in the settings with a high prevalence of β-lactam-resistant strains bacteria, initiated with higher than the recommended standard doses of meropenem. After than time, maintenance dose administered higher than adjusted dose according to CrCl, as a standard dose, or also higher than the standard dose in the sepsis and severe sepsis patients with AKI infected with a resistant strain of Gram-negative bacteria.
In the future, we suggested the evaluation of PK/PD parameters and safety of higher doses of meropenem in this population.
Conclusion
In conclusion, recommended standard doses of meropenem, 1 g every 8 h infused over 4 h, and adjusted according to renal function failed to achieve ≥ 80%ft > 4MIC in critically ill patients with AKI, who not receive RRT. Higher doses, i.e., 6 g daily with intermittent infusion are required for this PD target. Also, because of PK/PD variability observed, we strongly suggest using therapeutic drug monitoring (TDM) to be sure that target drug exposure is attained.
Limitation of the study
One limitation of our study was the calculation of Css ave with Eq. 5.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author, MS. The data are not publicly available due to the containing information that could compromise the privacy of research participants.
References
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. Jama 294(7):813–818. https://doi.org/10.1001/jama.294.7.813
Eyler RF, Mueller BA (2011) Antibiotic dosing in critically ill patients with acute kidney injury. Nat Rev Nephrol 7:226–235. https://doi.org/10.1038/nrneph.2011.12
Blot S, Lipman J, Roberts DM, Roberts JA The influence of acute kidney injury on antimicrobial dosing in critically ill patients: are dose reductions always necessary? Diagn Microbiol Infect Dis 79(1):77–84. https://doi.org/10.1016/j.diagmicrobio.2014.01.015
Matzke GR, Aronoff GR, Atkinson AJ Jr, Bennett WM, Decker BS, Eckardt K-U, Golper T, Grabe DW, Kasiske B, Keller F, Kielstein JT, Mehta R, Mueller BA, Pasko DA, Schaefer F, Sica DA, Inker LA, Umans JG, Murray P Drug dosing consideration in patients with acute and chronic kidney disease—a clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 80(11):1122–1137. https://doi.org/10.1038/ki.2011.322
Kees MG, Minichmayr IK, Moritz S, Beck S, Wicha SG, Kees F, Kloft C, Steinke T (2016) Population pharmacokinetics of meropenem during continuous infusion in surgical ICU patients. J Clin Pharmacol 56(3):307–315. https://doi.org/10.1002/jcph.600
Nicolau DP (2008) Pharmacokinetic and pharmacodynamic properties of meropenem. Clin Infect Dis 47(Suppl 1):S32–S40. https://doi.org/10.1086/590064
Taccone FS, Laterre P-F, Dugernier T, Spapen H, Delattre I, Wittebole X, De Backer D, Layeux B, Wallemacq P, Vincent J-L, Jacobs F (2010) Insufficient β-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care 14(4):R126. https://doi.org/10.1186/cc9091
Jaruratanasirikul S, Sriwiriyajan S (2003) Comparison of the pharmacodynamics of meropenem in healthy volunteers following administration by intermittent infusion or bolus injection. J Antimicrob Chemother 52(3):518–521. https://doi.org/10.1093/jac/dkg378
Mattioli F, Fucile C, Del Bono V, Marini V, Parisini A, Molin A, Zuccoli ML, Milano G, Danesi R, Marchese A, Polillo M, Viscoli C, Pelosi P, Martelli A, Di Paolo A (2016) Population pharmacokinetics and probability of target attainment of meropenem in critically ill patients. Eur J Clin Pharmacol 72(7):839–848. https://doi.org/10.1007/s00228-016-2053-x
Crandon JL, Ariano RE, Zelenitsky SA, Nicasio AM, Kuti JL, Nicolau DP (2011) Optimization of meropenem dosage in the critically ill population based on renal function. Intensive Care Med 37(4):632–638. https://doi.org/10.1007/s00134-010-2105-0
Wiseman LR, Wagstaff AJ, Brogden RN, Bryson HM (1995) Meropenem. Drugs 50(1):73–101
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120(4):c179–c184
Winter ME (2010) Basic clinical pharmacokinetics. Wolters Kluwer/Lippincott Williams & Wilkins Health
Chambers HF, Eliopoulos GM, Gilbert DN, Saag MS (2016) The Sanford guide to antimicrobial therapy 2016. Antimicrobial Therapy
Elkhaïli H, Niedergang S, Pompei D, Linger L, Leveque D, Jehl F (1996) High-performance liquid chromatographic assay for meropenem in serum. J Chromatogr B Biomed Sci Appl 686(1):19–26. https://doi.org/10.1016/S0378-4347(96)00205-8
Madden A, Tsikoura T, Stott D (2012) The estimation of body height from ulna length in healthy adults from different ethnic groups. J Hum Nutr Diet 25(2):121–128
Kothekar AT, Divatia JV, Myatra SN, Patil A, Krishnamurthy MN, Maheshwarappa HM, Siddiqui SS, Gurjar M, Biswas S, Gota V (2020) Clinical pharmacokinetics of 3-h extended infusion of meropenem in adult patients with severe sepsis and septic shock: implications for empirical therapy against Gram-negative bacteria. Ann Intensive Care 10(1):4
Gonçalves-Pereira J, Póvoa P (2011) Antibiotics in critically ill patients: a systematic review of the pharmacokinetics of β-lactams. Crit Care 15(5):R206
Leroy A, Fillastre J, Borsa-Lebas F, Etienne I, Humbert G (1992) Pharmacokinetics of meropenem (ICI 194,660) and its metabolite (ICI 213,689) in healthy subjects and in patients with renal impairment. Antimicrob Agents Chemother 36(12):2794–2798
Kitzes-Cohen R, Farin D, Piva G, De Myttenaere-Bursztein SA (2002) Pharmacokinetics and pharmacodynamics of meropenem in critically ill patients. Int J Antimicrob Agents 19(2):105–110. https://doi.org/10.1016/S0924-8579(01)00474-5
Jaruratanasirikul S, Thengyai S, Wongpoowarak W, Wattanavijitkul T, Tangkitwanitjaroen K, Sukarnjanaset W, Jullangkoon M, Samaeng M (2015) Population pharmacokinetics and Monte Carlo dosing simulations of meropenem during the early phase of severe sepsis and septic shock in critically ill patients in intensive care units. Antimicrob Agents Chemother 59(6):2995–3001
Petersson J, Giske C, Eliasson E (2016) Standard dosing of piperacillin and meropenem fail to achieve adequate plasma concentrations in ICU patients. Acta Anaesthesiol Scand 60(10):1425–1436
Thalhammer F, Traunmüller F, Frass M, Hollenstein U, Locker G, Staudinger T, Burgmann H (2000) Continuous infusion versus intermittent administration of meropenem in critically ill patients: a pilot study. In: Critical Careed. BioMed Central, pp 1-2
Acknowledgments
The authors thank Nahid Shahsavari (Clinical Pharmacy laboratory, faculty of Pharmacy, Shahid Beheshti University of Medical Science (SBMU)) for her skilled technical assistance during the setup of HPLC method, also thank all the nurses of the intensive care unit (ICU) of Imam Hossein medical center for helping us during sample gathering.
Author information
Authors and Affiliations
Contributions
MS, ShZ, and MK designed the study. Literature review, drafting of the proposal, and searching were done by MS, ShZ, and RH. RH, EP, MMM, SPS, AAK, and SS helped to gather the data. FK and FN set up and interpreted the HPLC method. MS and RH analyzed and interpreted data. All authors helped to manuscript improvement and finalize the article for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethics approval
This study has been approved by institutional review boards of the ethics committee of Shahid Beheshti University of Medical Science (SBMU) in Tehran, Iran (IR.SBMU.PHNM.1397.38).
Consent to participate
Written informed consent was obtained from patients or a person’s parents or legal guardians before enrollment in the study. They acknowledged that not to be identified via the paper; and that we have fully anonymized them.
Consent for publication
The authors have authorized MS to act as the corresponding author for submission and during the review process.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Hassanpour, R., Ziaie, S., Kobarfard, F. et al. Evaluation of pharmacokinetic and pharmacodynamic parameters of meropenem in critically ill patients with acute kidney disease. Eur J Clin Pharmacol 77, 831–840 (2021). https://doi.org/10.1007/s00228-020-03062-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-03062-0