Abstract
Purpose
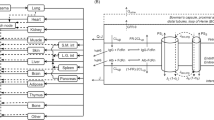
This study aimed to predict the presence and mechanism of busulfan drug-drug interactions (DDIs) in hematopoietic stem cell transplantation (HSCT) using pharmacokinetic interaction (PKI) network–based molecular structure similarity and network pharmacology.
Methods
Logistic function models were established to predict busulfan DDIs based on the assumption that an approved drug tends to interact with the drug used in HSCT (DH) if structurally similar to the drugs in the PKI network of the DH. The PKI network of the DH represented the association between drugs and the proteins related to the PK of the DH. The most appropriate model was applied to predict busulfan DDIs in HSCT. Candidate targets for busulfan DDIs and their interacting were identified by network pharmacology.
Results
Six of the top ten predicted busulfan DDIs were clinically relevant and involved voriconazole, fludarabine, itraconazole, cyclophosphamide, metronidazole, and melphalan. Candidate targets for these DDIs were CYP450s (3A4, 2B6, 2C9, and 2C19), GSTs (GSTA1, GSTP1, GSTT1, and GSTM1), and ABC transporters (ABCB1, ABCC1, ABCC2, and ABCC3), in the targets of drug-induced liver injury (DILI). The networks of interacting proteins and candidate targets indicated the regulatory potential of pregnane X receptor (PXR), as a nuclear receptor. Enrichment analysis showed the metabolism of drugs and xenobiotics, glutathione metabolism, and bile secretion associated with busulfan DDIs and DILI.
Conclusions
This study has successfully predicted busulfan DDIs in HSCT through PKI-based molecular structure similarity. The mechanism of busulfan DDI and DILI was attributed mostly to CYP450s, GSTs, and ABC transporters, and PXR was identified as a potential target.



Similar content being viewed by others
References
Barriga F, Ramírez P, Wietstruck A, Rojas N (2012) Hematopoietic stem cell transplantation: clinical use and perspectives. Biol Res 45(3):307–316. https://doi.org/10.4067/S0716-97602012000300012
Ciurea SO, Andersson BS (2009) Busulfan in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 15(5):523–536. https://doi.org/10.1016/j.bbmt.2008.12.489
Ansari M, Théoret Y, Rezgui MA, Peters C, Mezziani S, Desjean C, Vachon MF, Champagne MA, Duval M, Krajinovic M, Bittencourt H (2014) Association between busulfan exposure and outcome in children receiving intravenous busulfan before hematopoietic stem cell transplantation. Ther Drug Monit 36(1):93–99. https://doi.org/10.1097/FTD.0b013e3182a04fc7
Andersson BS, Thall PF, Madden T, Couriel D, Wang X, Tran HT, Anderlini P, de Lima M, Gajewski J, Champlin RE (2002) Busulfan systemic exposure relative to regimen-related toxicity and acute graft-versus-host disease: defining a therapeutic window for i.v. BuCy2 in chronic myelogenous leukemia. Biol Blood Marrow Transplant 8(9):477–485. https://doi.org/10.1053/bbmt.2002.v8.pm12374452
Hong KT, Kang HJ, Choi JY, Hong CR, Cheon JE, Park JD, Park KD, Song SH, Yu KS, Jang IJ, Shin HY (2018) Favorable outcome of post-transplantation cyclophosphamide haploidentical peripheral blood stem cell transplantation with targeted busulfan-based myeloablative conditioning using intensive pharmacokinetic monitoring in pediatric patients. Biol Blood Marrow Transplant 24(11):2239–2244. https://doi.org/10.1016/j.bbmt.2018.06.034
Sweiss K, Quigley JG, Oh A, Lee J, Ye R, Rondelli D, Patel P (2019) A novel drug interaction between busulfan and blinatumomab. J Oncol Pharm Pract 25(1):226–228. https://doi.org/10.1177/1078155217729745
Hassan M, Ljungman P, Ringdén O, Hassan Z, Oberg G, Nilsson C, Békassy A, Bielenstein M, Abdel-Rehim M, Georén S et al (2000) The effect of busulphan on the pharmacokinetics of cyclophosphamide and its 4-hydroxy metabolite: time interval influence on therapeutic efficacy and therapy-related toxicity. Bone Marrow Transplant 25(9):915–924. https://doi.org/10.1038/sj.bmt.1702377
Myers AL, Kawedia JD, Champlin RE, Kramer MA, Nieto Y, Ghose R, Andersson BS (2017) Clarifying busulfan metabolism and drug interactions to support new therapeutic drug monitoring strategies: a comprehensive review. Expert Opin Drug Metab Toxicol 13(9):901–923. https://doi.org/10.1080/17425255.2017.1360277
Vilar S, Harpaz R, Uriarte E, Santana L, Rabadan R, Friedman C (2012) Drug-drug interaction through molecular structure similarity analysis. J Am Med Inform Assoc 19(6):1066–1074. https://doi.org/10.1136/amiajnl-2012-000935
Trevisan DD, Silva JB, Oliveira HC, Secoli SR, Lima MH (2015) Prevalence and clinical significance of potential drug-drug interaction in hematopoietic stem cell transplantation. Cancer Chemother Pharmacol 75(2):393–400. https://doi.org/10.1007/s00280-014-2657-8
Guastaldi RB, Reis AM, Figueras A, Secoli SR (2011) Prevalence of potential drug-drug interactions in bone marrow transplant patients. Int J Clin Pharm 33(6):1002–1009. https://doi.org/10.1007/s11096-011-9574-2
Carreras E, Dufour C, Mohty M, Kröger N (2019) The EBMT handbook: hematopoietic stem cell transplantation and cellular therapies. Springer. https://doi.org/10.1007/978-3-030-02278-5
Leather HL (2004) Drug interactions in the hematopoietic stem cell transplant (HSCT) recipient: what every transplanter needs to know. Bone Marrow Transplant 33(2):137–152. https://doi.org/10.1038/sj.bmt.1704316
Takeda T, Hao M, Cheng T, Bryant SH, Wang Y (2017) Predicting drug-drug interactions through drug structural similarities and interaction networks incorporating pharmacokinetics and pharmacodynamics knowledge. J Cheminform 9:16. https://doi.org/10.1186/s13321-017-0200-8
Dhere V, Edelman S, Waller EK, Langston A, Graiser M, Connolly EC, Switchenko JM, Esiashvili N, Khan MK (2018) Myeloablative busulfan/cytoxan conditioning versus reduced-intensity fludarabine/melphalan conditioning for allogeneic hematopoietic stem cell transplant in patients with acute myelogenous leukemia. Leuk Lymphoma 59(4):837–843. https://doi.org/10.1080/10428194.2017.1361027
Andersson BS, de Lima M, Thall PF, Wang X, Couriel D, Korbling M, Roberson S, Giralt S, Pierre B, Russell JA, Shpall EJ, Jones RB, Champlin RE (2008) Once daily i.v. busulfan and fludarabine (i.v. Bu-Flu) compares favorably with i.v. busulfan and cyclophosphamide (i.v. BuCy2) as pretransplant conditioning therapy in AML/MDS. Biol Blood Marrow Transplant 14(6):672–684. https://doi.org/10.1016/j.bbmt.2008.03.009
Bouligand J, Richard C, Valteau-Couanet D, Orear C, Mercier L, Kessari R, Simonnard N, Munier F, Daudigeos-Dubus E, Tou B, Opolon P, Deroussent A, Paci A, Vassal G (2016) Iron overload exacerbates busulfan-melphalan toxicity through a pharmacodynamic interaction in mice. Pharm Res 33(8):1913–1922. https://doi.org/10.1007/s11095-016-1927-z
Yeh RF, Pawlikowski MA, Blough DK, McDonald GB, O’Donnell PV, Rezvani A, Deeg HJ, McCune JS (2012) Accurate targeting of daily intravenous busulfan with 8-hour blood sampling in hospitalized adult hematopoietic cell transplant recipients. Biol Blood Marrow Transplant 18(2):265–272. https://doi.org/10.1016/j.bbmt.2011.06.013
Perkins JB, Kim J, Anasetti C, Fernandez HF, Perez LE, Ayala E, Kharfan-Dabaja MA, Tomblyn MR, Sullivan DM, Pidala JA, Field TL (2012) Maximally tolerated busulfan systemic exposure in combination with fludarabine as conditioning before allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 18(7):1099–1107. https://doi.org/10.1016/j.bbmt.2011.12.584
Bonin M, Pursche S, Bergeman T, Leopold T, Illmer T, Ehninger G, Schleyer E, Bornhauser M (2007) F-ara-A pharmacokinetics during reduced-intensity conditioning therapy with fludarabine and busulfan. Bone Marrow Transplant 39(4):201–206. https://doi.org/10.1038/sj.bmt.1705565
Nilsson C, Aschan J, Hentschke P, Ringden O, Ljungman P, Hassan M (2003) The effect of metronidazole on busulfan pharmacokinetics in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 31(6):429–435. https://doi.org/10.1038/sj.bmt.1703896
Glotzbecker B, Duncan C, Alyea E 3rd, Campbell B, Soiffer R (2012) Important drug interactions in hematopoietic stem cell transplantation: what every physician should know. Biol Blood Marrow Transplant 18(7):989–1006. https://doi.org/10.1016/j.bbmt.2011.11.029
Buggia I, Zecca M, Alessandrino EP, Locatelli F, Rosti G, Bosi A, Pession A, Rotoli B, Majolino I, Dallorso A, Regazzi MB (1996) Itraconazole can increase systemic exposure to busulfan in patients given bone marrow transplantation. Anticancer Res 16(4A):2083–2088
Brewer CT, Chen T (2016) PXR variants: the impact on drug metabolism and therapeutic responses. Acta Pharm Sin B 6(5):441–449. https://doi.org/10.1016/j.apsb.2016.07.002
Pejčić A, Janković SM, Opančina V, Babić G, Milosavljević M (2018) Drug–drug interactions in patients receiving hematopoietic stem cell transplantation. Expert Opin Drug Metab Toxicol 15(1):49–59. https://doi.org/10.1080/17425255.2019.1552256
Uppugunduri CR, Rezgui MA, Diaz PH, Tyagi AK, Rousseau J, Daali Y, Duval M, Bittencourt H, Krajinovic M, Ansari M (2014) The association of cytochrome P450 genetic polymorphisms with sulfolane formation and the efficacy of a busulfan-based conditioning regimen in pediatric patients undergoing hematopoietic stem cell transplantation. Pharmacogenomics J 14(3):263–271. https://doi.org/10.1038/tpj.2013.38
Kusama M, Kubota T, Matsukura Y, Matsuno K, Ogawa S, Kanda Y, Iga T (2006) Influence of glutathione S-transferase A1 polymorphism on the pharmacokinetics of busulfan. Clin Chim Acta 368(1–2):93–98. https://doi.org/10.1016/j.cca.2005.12.011
Pirmohamed M (2003) Cytochrome P450 enzyme polymorphisms and adverse drug reactions. Toxicology 192(1):23–32. https://doi.org/10.1016/s0300-483x(03)00247-6
Bahar MA, Setiawan D, Hak E, Wilffert B (2017) Pharmacogenetics of drug-drug interaction and drug-drug-gene interaction: a systematic review on CYP2C9, CYP2C19 and CYP2D6. Pharmacogenomics 18(7):701–739. https://doi.org/10.2217/pgs-2017-0194
Moriyama B, Kadri S, Henning SA, Danner RL, Walsh TJ, Penzak SR (2015) Therapeutic drug monitoring and genotypic screening in the clinical use of voriconazole. Curr Fungal Infect Rep 9(2):74–87. https://doi.org/10.1007/s12281-015-0219-0
Beata S, Donata UK, Jaroslaw D, Tomasz W, Anna WH (2017) Influence of CYP2C19*2/*17 genotype on adverse drug reactions of voriconazole in patients after allo-HSCT: a four-case report. J Cancer Res Clin Oncol 143(6):1103–1106. https://doi.org/10.1007/s00432-017-2357-y
Zgheib NK, Alameddine R, Massoud R, Nasr R, Zahreddine A, El Cheikh J, Mahfouz R, Bazarbachi A (2020) The role of candidate genetic polymorphisms in the interaction between voriconazole and cyclosporine in patients undergoing allogeneic hematopoietic cell transplantation: an explorative study. Curr Res Transl Med 68(2):51–58. https://doi.org/10.1016/j.retram.2020.02.001
Czerwinski M, Gibbs JP, Slattery JT (1996) Busulfan conjugation by glutathione S-transferases alpha, mu, and pi. Drug Metab Dispos 24(9):1015–1019
Hassan M, Ehrsson H (1987) Metabolism of 14C-busulfan in isolated perfused rat liver. Eur J Drug Metab Pharmacokinet 12(1):71–76. https://doi.org/10.1007/BF03189864
Hassan M, Andersson BS (2013) Role of pharmacogenetics in busulfan/cyclophosphamide conditioning therapy prior to hematopoietic stem cell transplantation. Pharmacogenomics 14(1):75–87. https://doi.org/10.2217/pgs.12.185
Kühne A, Sezer O, Heider U, Meineke I, Muhlke S, Niere W, Overbeck T, Hohloch K, Trümper L, Brockmöller J, Kaiser R (2008) Population pharmacokinetics of melphalan and glutathione S-transferase polymorphisms in relation to side effects. Clin Pharmacol Ther 83(5):749–757. https://doi.org/10.1038/sj.clpt.6100336
Johnson GG, Lin K, Cox TF, Oates M, Sibson DR, Eccles R, Lloyd B, Gardiner LJ, Carr DF, Pirmohamed M, Strefford JC, Oscier DG, Gonzalez de Castro D, Else M, Catovsky D, Pettitt AR (2013) CYP2B6*6 is an independent determinant of inferior response to fludarabine plus cyclophosphamide in chronic lymphocytic leukemia. Blood 122(26):4253–4258. https://doi.org/10.1182/blood-2013-07-516666
Murayama N, Imai N, Nakane T, Shimizu M, Yamazaki H (2007) Roles of CYP3A4 and CYP2C19 in methyl hydroxylated and N-oxidized metabolite formation from voriconazole, a new anti-fungal agent, in human liver microsomes. Biochem Pharmacol 73(12):2020–2026. https://doi.org/10.1016/j.bcp.2007.03.012
Walsky RL, Astuccio AV, Obach RS (2006) Evaluation of 227 drugs for in vitro inhibition of cytochrome P450 2B6. J Clin Pharmacol 46(12):1426–1438. https://doi.org/10.1177/0091270006293753
Tarantino G, Di Minno MN, Capone D (2009) Drug-induced liver injury: is it somehow foreseeable? World J Gastroenterol 15(23):2817–2833. https://doi.org/10.3748/wjg.15.2817
Daly AK (2017) Are polymorphisms in genes relevant to drug disposition predictors of susceptibility to drug-induced liver injury? Pharm Res 34(8):1564–1569. https://doi.org/10.1007/s11095-016-2091-1
Andrade RJ, Agúndez JA, Lucena MI, Martínez C, Cueto R, García-Martín E (2009) Pharmacogenomics in drug induced liver injury. Curr Drug Metab 10(9):956–970. https://doi.org/10.2174/138920009790711805
Li Y, Lin N, Ji X, Mai J, Li Q (2019) Organotin compound DBDCT induces CYP3A suppression through NF-κB-mediated repression of PXR activity. Metallomics 11(5):936–948. https://doi.org/10.1039/c8mt00361k
Bonifazi F, Storci G, Bandini G, Marasco E, Dan E, Zani E, Albani F, Bertoni S, Bontadini A, De Carolis S et al (2014) Glutathione transferase-A2 S112T polymorphism predicts survival, transplant-related mortality, busulfan and bilirubin blood levels after allogeneic stem cell transplantation. Haematologica 99(1):172–179. https://doi.org/10.3324/haematol.2013.089888
Wardyn JD, Ponsford AH, Sanderson CM (2015) Dissecting molecular cross-talk between Nrf2 and NF-kappaB response pathways. Biochem Soc Trans 43(4):621–626. https://doi.org/10.1042/BST20150014
Shi S, Li Y (2014) Interplay of drug-metabolizing enzymes and transporters in drug absorption and disposition. Curr Drug Metab 15(10):915–941. https://doi.org/10.2174/1389200216666150401110610
Guilcher GMT, Shah R, Shenoy S (2018) Principles of alemtuzumab immunoablation in hematopoietic cell transplantation for non-malignant diseases in children: a review. Pediatr Transplant 22(2). https://doi.org/10.1111/petr.13142
Funding
This work was funded by the National Natural Science Foundation in China (Grant No. 81503137).
Author information
Authors and Affiliations
Contributions
Chenxia Hao designed the study and wrote the manuscript. Xiaoqin Ma performed the study and wrote the manuscript. Wanhua Yang and Jingjing Huang regulated the entire project and reviewed the manuscript. Jiong Hu, Lining Wang, and Weixia Zhang analyzed the data and interpreted the results.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hao, C., Ma, X., Wang, L. et al. Predicting the presence and mechanism of busulfan drug-drug interactions in hematopoietic stem cell transplantation using pharmacokinetic interaction network–based molecular structure similarity and network pharmacology. Eur J Clin Pharmacol 77, 595–605 (2021). https://doi.org/10.1007/s00228-020-03034-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-03034-4