Abstract
Despite considerable progress in identifying specific HLA alleles as genetic risk factors for some forms of drug-induced liver injury, progress in understanding whether genetic polymorphisms relevant to drug disposition also contribute to risk for developing this serious toxicity has been more limited. Evidence from both candidate-gene case control studies and genome-wide association studies is now discussed. In the case of genes relevant to drug metabolism, polymorphisms in cytochromes P450, UDP-glucuronosyltransferases, N-acetyltransferases and glutathione S-transferases as risk factors for DILI are assessed. The relevance of ABC transporters to drug-induced liver injury is also considered, together with data showing associations of particular ABCB11, ABCB1 and ABCC2 polymorphisms with some forms of drug-induced liver injury. Very few of the associations with genes relevant to drug disposition that have been reported have been well replicated. Even apparently well-studied associations such as that between isoniazid liver injury and N-acetyltransferase 2 slow acetylators remain problematic, though it seems likely that polymorphisms in drug metabolism genes do contribute to risk for some specific drugs. A better understanding of genetic risk factors for drug-induced liver injury will require further genome-wide association studies with larger numbers of cases, especially for forms of drug-induced liver injury where HLA genotype does not appear to be a risk factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
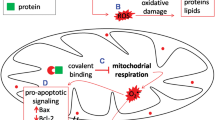
Drug-induced liver injury (DILI) is one of the most common reasons for drug withdrawal, either at a late stage of the drug development process or soon after licensing (1). It is also an important contributor to serious liver disease, though the majority of DILI cases that lead to acute liver failure are due to acetaminophen overdose rather than the rarer idiosyncratic DILI where the disease develops after the causative drug is used at the recommended dose (2). It is generally considered that metabolism of the causative drug to a reactive intermediate is an important step in the DILI process (3). In addition, impaired membrane transport in the hepatocyte, affecting either drug transport directly or bile acid transport, is considered to be a contributor to DILI, possibly by promoting accumulation of reactive intermediates or of toxic bile acids in hepatocytes (4). There is extensive data available on the functional significance of a range of polymorphisms in the genes encoding drug metabolizing enzymes and transporters. This has enabled studies on the possibility of a relationship between genotype for biologically plausible polymorphisms in these genes and risk of DILI development to be performed, resulting in some interesting observations giving insights into the underlying mechanism, though this overall area is still unclear with an absence of strong effects reported. Most genetic associations reported to date for DILI relate to HLA genes, pointing to an important role for an inappropriate immune response (5). However, not all forms of DILI show an association with a particular HLA genotype. The formation of reactive intermediates may also contribute to an inappropriate immune response so a role for genes contributing to drug disposition alongside HLA genes in DILI remains plausible.
Cytochromes P450
Because of the ability of the cytochromes P450 to metabolize a wide range of drugs to reactive intermediates and also the extent of interindividual variation in levels of P450 enzymes, polymorphisms in these genes are good candidates as susceptibility factors for DILI. An important role for P450 genes in DILI susceptibility has not been confirmed to date, though there are a few reports of associations in relation to particular drugs. In the concentration-dependent form of DILI seen in acetaminophen overdose, activation to the N-acetyl-p-benzoquinoneimine (NAPQI) reactive metabolite is the well established mechanism for toxicity. A recent study has shown a strong correlation between levels of total P450-generated metabolites and serious liver toxicity (6). CYP2E1, CYP1A2 and CYP3A are well established contributors to NAPQI production (7). Studies on the relationship between CYP genotype and development of DILI following overdose are very limited but one relatively large study reported a borderline significant relationship between CYP3A5*1 in patients who took an intentional overdose and developed acute liver failure (8). This allele is associated with CYP3A5 expression and therefore, on average, an overall higher CYP3A activity. The finding is biologically plausible but needs confirmation in another similar cohort.
Findings on relationship between CYP alleles and idiosyncratic DILI are quite limited. There is a report from the 1980s that CYP2D6 poor metabolizers were more susceptible to perhexiline-induced DILI but, since this drug was withdrawn soon after the study, follow-up was not possible (9). More recently, a role for another P450 isoform, CYP2B6, in two different forms of idiosyncratic DILI has been suggested. For DILI due to ticlopidine, an upstream SNP (rs7254579 which results in -2320T>C) which has been reported to be associated with increased CYP2B6 expression (10) was significantly more common among cases (11). It is possible that this variant could be associated with increased reactive intermediate levels leading to increased risk of DILI. On the other hand, in cases of DILI due to efavirenz, the CYP2B6*6 allele appears to be more common (12). This variant is associated with lower than normal CYP2B6 activity suggesting that for efavirenz, accumulation of the parent drug might be an important factor in DILI.
A possible association between CYP2E1 and DILI due to isoniazid has been fairly extensively investigated but studies have not shown consistent associations. This may reflect limited effects of common CYP2E1 genetic polymorphisms on enzyme activity and expression and this is still a confusing area. Most studies concerned the CYP2E1*5 variant (rs2031920) (an allele often detected using the restriction enzyme RsaI) for which the biological significance remains unclear (for review see (13)). More detailed studies investigating other CYP2E1 polymorphisms for this form of DILI might be worthwhile, though a genome-wide association study (GWAS) involving 28 cases of isoniazid DILI found no evidence for a contribution from any CYP2E1 polymorphisms (or other genes) to susceptibility (14).
UDP-glucuronosyltransferases (UGT)
Members of the UGT family make probably the largest contribution to phase II metabolism of drugs implicated in DILI. They are relevant as DILI risk factors because of their role in detoxicating reactive metabolites (or the parent drug) but also because acylglucuronides generate by glucuronidation of carboxyl groups are reactive intermediates which may themselves bind covalently to proteins triggering direct toxicity or an inappropriate immune response (15). The main associations involving UGT genes reported to date for DILI concern acetaminophen overdose and idiosyncratic reactions induced by diclofenac and tolcapone.
A number of different UGT isoforms contribute to acetaminophen glucuronidation, including 3 members of the UGT1A family which all originate from the same UGT1A gene. Studies with a human liver bank indicated that three polymorphisms at the 3’-untranslated region correlate with an increased acetaminophen glucuronidation activity, possibly due to effects on exon splicing. Carriage of one of these polymorphisms (rs8330) appeared to protect against the development of acute liver failure in patients who had suffered an unintentional overdose (16).
Tolcapone, an inhibitor of catechol-O-methyltransferase used in treatment of Parkinson’s disease, can give rise to elevated transaminase levels in some patients. Several polymorphisms in the glucuronidating enzyme UGT1A6 promoter region were found to be significantly associated with elevated transaminase levels (17). Because these polymorphisms appear to be associated with decreased enzyme levels, it was suggested that the toxicity might be linked to slow metabolism of the parent drug. It was suggested subsequently that promoter region polymorphisms in the nearby UGT1A9 may also be relevant to DILI from this drug (18).
Diclofenac is a widely prescribed non-steroidal antiinflammatory which is a relatively common cause of DILI worldwide. This compound undergoes glucuronidation by UGT2B7. In a study on susceptibility to diclofenac-related DILI, possession of UGT2B7*2, which is believed to be associated with higher than normal glucuronidating activity, was associated with an increased risk of toxicity (19). This suggests that the underlying mechanism for toxicity might involve production of high levels of diclofenac acylglucuronide. A slightly larger follow-up study (n = 30) which included some of the samples from the earlier diclofenac DILI study involved a genome-wide association study approach. In a substudy of genes relevant to drug disposition only, SNPs in the UGT2B region which were in linkage disequilibrium with the UGT2B7*2-related SNPs were more common in the diclofenac DILI cases (14).
N-acetyltransferase 2
The phase II enzyme N-acetyltransferase 2 (NAT2) has only a minor role in drug metabolism generally but a key role in metabolism of isoniazid, an important drug in the treatment of tuberculosis (TB), which is usually used in combination with other drugs. NAT2 is subject to a well studied genetic polymorphism with approx. 50% of individuals from a number of different ethnic groups lacking this enzyme activity entirely, usually due to the presence of a coding region polymorphism which affects enzyme stability or activity. Isoniazid is a common cause of DILI. Acetylhydrazine, an isoniazid metabolite which can undergo metabolism by cytochrome P450 to a toxic metabolite or by NAT2 to the less toxic diacetylhydrazine, may be the cause of toxicity but the parent drug, which is seen at higher plasma levels in those with no NAT2 activity, may also contribute (20). A possible association between NAT2 genotype and DILI susceptibility has been investigated extensively. As reviewed recently, there are a large number of studies on this aspect with the majority suggesting that absence of NAT2 activity (slow acetylator phenotype) is a risk factor for isoniazid DILI (21). However, the GWAS discussed above involving 28 cases of isoniazid DILI did not detect a signal at the NAT2 gene (14). Though reports showing this association continue to appear (22–24), there are limitations to most since the studies generally involve very small numbers of cases and often concern cases with very mild DILI which is quite common but usually resolves without the need to discontinue drug treatment. An added complication is that patients are usually also prescribed pyrazinamide, which can also cause DILI but is not metabolized by NAT2.
Glutathione S-transferases
The glutathione S-transferases (GST) metabolize a range of drugs by glutathione conjugation and also have a role in protection against oxidative stress. Two GST isoforms, GSTM1 and T1, are absent in significant numbers of individuals due to large gene deletions. Candidate gene studies on GST in relation to a number of types of DILI have been performed. These suggest that individuals homozygous null for both GSTM1 and GSTT1 are at increased risk of DILI due to troglitazone, amoxicillin-clavulanate and also possibly a wider range of drugs (25–27). Data for isoniazid-related DILI is rather contradictory with two studies reporting an increased frequency of GSTM1 homozygous null genotypes only (28,29) and a third increased GSTT1 homozygous null only (30). The finding on troglitazone is consistent with the finding that GSTM1 but not GSTT1 has a role in detoxication of a quinone metabolite of this drug (31) but there appears to be no direct role for GST in amoxicillin-clavulanate or isoniazid elimination. Independent replication of these suggested GST associations is still needed.
ABC Transporters
ABC transporters, including the specific bile acid transporter BSEP which is encoded by ABCB11, are of considerable interest in relation to DILI, especially for cholestatic forms of the disease where bile acids accumulate within hepatocytes, resulting in local toxicity. Other ABC transporters, including MDR1 and MRP2 which both contribute to biliary excretion of a range of drugs, are also plausible candidates as DILI risk factors (4). In addition to genetic variation, inhibition of the normal ABC transporter function by certain drugs may contribute to risk of DILI (32). It is possible that inhibition may be more problematic in individuals where transporter expression or activity is lower than normal due to the presence of genetic polymorphisms. In general, genome-wide association studies on DILI have failed to demonstrate any significant signals from ABC transporters, suggesting that any role as a genetic risk factor is relatively small (compared with, for example, HLA genotype) or is specific to only a few specific drugs (14). Some slightly more positive findings have emerged from candidate gene studies.
In a study on a small group of patients who had suffered DILI relating to a range of different drugs, an association between cholestatic injury and a polymorphism in exon 13 of ABCB11 was reported (33). The effect on disease risk from this common polymorphism was small and it therefore seems unlikely to be a major risk factor for DILI. In a more detailed study involving genotyping for a larger number of polymorphisms including the exon 13 variant, no association with DILI was detected (34). In contrast to the original finding about ABCB11 and cholestatic DILI, a further study on the exon 13 variant suggested that possession of this allele was associated with increased risk of hepatocellular disease, especially with non-steroidal antiinflammatory drugs (35).
MRP2 has a major role in the biliary excretion of many glucuronide conjugates and is encoded by ABCC2. In the study on diclofenac DILI described above where an association with UGT2B7 polymorphisms was detected, carriage of an upstream polymorphism in ABCC2 (rs717620; −24C>T) was found to be significantly more common among DILI cases (19). This finding is consistent with increased levels of the reactive diclofenac acyl glucuronide being linked to toxicity on the basis of findings that −24C>T results in lower expression of the MRP2 protein which would favor cellular accumulation of the glucuronide (36). In a Korean study on DILI caused by a range of drugs, a polymorphism in linkage disequilibrium with −24C>T was a significant risk factor for the development of hepatocellular toxicity whereas a second promoter region polymorphism was a risk factor for cholestatic or mixed disease (37). These findings regarding ABCC2 −24C>T are in broad agreement with the data on diclofenac toxicity. In a substudy concerned only with drug disposition genes which formed part of a larger GWAS on DILI, the lowest p values for drug disposition-related genes were seen for a series of ABCC2 polymorphisms (14). More recently, a study based in Spain on ABC transporter polymorphisms as risk factors for DILI found some associations with a rare ABCC2 genotype and also reported an association between an extended ABCC2 haplotype and disease severity (38).
Genotypes for another transporter gene, ABCB1 which codes for MDR1, have been studied in patients with DILI due to nevirapine. In African DILI cases, there was a significantly decreased frequency of the ABCB1 SNP 3435C>T (rs1045642) (39) and a similar association was also reported in a US patient group (40). However, a subsequent study on a separate group of European nevirapine DILI patients failed to confirm this association (41). No association between ABCB1 polymorphisms and DILI more generally has been found to date.
Two other ABC transporters, MRP3 and MRP4 (encoded by the ABCC3 and ABCC4 genes) are found on the basolateral membrane of the hepatocyte and are also of interest in relation to DILI susceptibility when data from model systems is considered. MRP4 is expressed at higher levels than MRP3 in human hepatocytes and also appears more important in efflux of bile acids, especially in cholestasis (42,43). It has been suggested that MRP4 inhibition by some compounds is an important underlying mechanism for bile acid accumulation in cholestatic DILI (44). For example, troglitazone and its sulfate metabolite inhibit both BSEP and MRP4 (45). In the case of MRP3, inhibition of transport by drugs appears less relevant to DILI generally but there is evidence that in a Mrp3 mouse knockout model, basolateral efflux of diclofenac acylglucuronide is lost and that the animals show increased gastrointestinal ulceration (46). It is possible that hepatic accumulation of diclofenac acylglucuronide when both MRP2 and MRP3 levels are low due to genetics or drug inhibition could be a factor in the human liver toxicity (47). However, as with the other candidate transporter polymorphisms, to date no association involving ABCC3 (MRP3) has been detected in a GWAS (14).
Concluding Remarks and Future Perspectives
There are essentially no well-replicated and completely convincing data showing associations between DILI susceptibility and specific genes relevant to drug disposition. Table I lists selected examples from those discussed in detail above which show reasonable biological plausibility but where further confirmation is still needed. The availability of GWAS approaches has added to the complexity since essentially no previously reported associations (e.g. NAT2 genotype and isoniazid DILI) have been replicated in GWAS up to now. GWAS on DILI has been successful in demonstrating HLA associations with odds ratios of approx. 2.5 or higher, even when case numbers are small, but generally other risk factors, which may well include some of the genes relevant to drug disposition discussed above, have not yet emerged from these analyses. The failure to detect these additional risk factors is not necessarily that they don’t exist but possibly because the effect sizes reported in small candidate gene studies are biased towards only strongly positive findings being reported. A better understanding of genetic risk factors for these rare events will require larger numbers of well phenotyped cases to be collected and analyzed using GWAS and DNA sequencing approaches. This is feasible through international collaboration for drugs in current use. However, where drugs have been withdrawn from the market due to serious DILI, the number of cases available for genetic studies may be relatively small and access to them difficult. The need for larger studies applies to the more common concentration-dependent toxicity seen in acetaminophen overdose as well as to idiosyncratic DILI.
Where the increased risk of an ADR such as DILI due to a particular genotype is in the order of 1 to 2 fold, the relevance of this to treatment decisions may be limited. However, this level of risk from single genetic risk factors is seen for a range of complex diseases including many cancers and type II diabetes where large numbers of such risk factors have now emerged (48). Additive risks or interactions between risk factors may still determine overall risk. It is already clear that factors such as age and gender are also predictors of risk for some forms of idiosyncratic DILI. It may be possible to develop algorithms to assess individual risk of DILI in the future and these may include genotype for polymorphisms relating to drug disposition.
Abbreviations
- DILI:
-
Drug-induced liver injury
- GST:
-
Glutathione S-transferase
- GWAS:
-
Genome-wide association study
- HLA:
-
Human leukocyte antigen
- NAPQI:
-
N-acetyl-p-benzoquinoneimine
- NAT2:
-
N-acetyltransferase 2
- SNP:
-
Single nucleotide polymorphism
- UGT:
-
UDP-glucuronosyltransferases
References
Wilke RA, Lin DW, Roden DM, Watkins PB, Flockhart D, Zineh I, et al. Identifying genetic risk factors for serious adverse drug reactions: current progress and challenges. Nat Rev Drug Discov. 2007;6(11):904–16.
Ostapowicz G, Fontana RJ, Schiodt FV, Larson A, Davern TJ, Han SH, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137(12):947–54.
Park BK, Kitteringham NR, Maggs JL, Pirmohamed M, Williams DP. The role of metabolic activation in drug-induced hepatotoxicity. Annu Rev Pharmacol Toxicol. 2005;45:177–202.
Russmann S, Jetter A, Kullak-Ublick GA. Pharmacogenetics of drug-induced liver injury. Hepatology ;52(2):748–761.
Urban TJ, Daly AK, Aithal GR. Genetic basis of drug-induced liver injury: present and future. Semin Liver Dis. 2014;34(2):123–33.
Vliegenthart AD, Kimmitt RA, Seymour JH, Homer NZ, Clarke JI, Eddleston M, et al. Circulating acetaminophen metabolites are toxicokinetic biomarkers of acute liver injury. Clin Pharmacol Ther. 2016.
Patten CJ, Thomas PE, Guy RL, Lee M, Gonzalez FJ, Guengerich FP, et al. Cytochrome P450 enzymes involved in acetaminophen activation by rat and human liver microsomes and their kinetics. Chem Res Toxicol. 1993;6(4):511–8.
Court MH, Peter I, Hazarika S, Vasiadi M, Greenblatt DJ, Lee WM. Candidate gene polymorphisms in patients with acetaminophen-induced acute liver failure. Drug Metab Dispos. 2014;42(1):28–32.
Morgan MY, Reshef R, Shah RR, Oates NS, Smith RL, Sherlock S. Impaired oxidation of debrisoquine in patients with perhexiline liver injury. Gut. 1984;25(10):1057–64.
Hesse LM, He P, Krishnaswamy S, Hao Q, Hogan K, von Moltke LL, et al. Pharmacogenetic determinants of interindividual variability in bupropion hydroxylation by cytochrome P450 2B6 in human liver microsomes. Pharmacogenetics. 2004;14(4):225–38.
Ariyoshi N, Iga Y, Hirata K, Sato Y, Miura G, Ishii I, et al. Enhanced susceptibility of HLA-mediated ticlopidine-induced idiosyncratic hepatotoxicity by CYP2B6 polymorphism in Japanese. Drug Metab Pharmacokinet. 2010;25(3):298–306.
Yimer G, Amogne W, Habtewold A, Makonnen E, Ueda N, Suda A, et al. High plasma efavirenz level and CYP2B6*6 are associated with efavirenz-based HAART-induced liver injury in the treatment of naive HIV patients from Ethiopia: a prospective cohort study. Pharmacogenomics J. 2011.
Daly AK, Day CP. Genetic association studies in drug-induced liver injury. Drug Metab Rev. 2012;44(1):116–26.
Urban TJ, Shen Y, Stolz A, Chalasani N, Fontana RJ, Rochon J, et al. Limited contribution of common genetic variants to risk for liver injury due to a variety of drugs. Pharmacogenet Genomics. 2012;22(11):784–95.
Spahn-Langguth H, Benet LZ. Acyl glucuronides revisited: is the glucuronidation process a toxification as well as a detoxification mechanism? Drug Metab Rev. 1992;24(1):5–47.
Court MH, Freytsis M, Wang X, Peter I, Guillemette C, Hazarika S, et al. The UDP-glucuronosyltransferase (UGT) 1A polymorphism c.2042C > G (rs8330) is associated with increased human liver acetaminophen glucuronidation, increased UGT1A exon 5a/5b splice variant mRNA ratio, and decreased risk of unintentional acetaminophen-induced acute liver failure. J Pharmacol Exp Ther. 2013;345(2):297–307.
Acuna G, Foernzler D, Leong D, Rabbia M, Smit R, Dorflinger E, et al. Pharmacogenetic analysis of adverse drug effect reveals genetic variant for susceptibility to liver toxicity. Pharmacogenomics J. 2002;2(5):327–34.
Martignoni E, Cosentino M, Ferrari M, Porta G, Mattarucchi E, Marino F, et al. Two patients with COMT inhibitor-induced hepatic dysfunction and UGT1A9 genetic polymorphism. Neurology. 2005;65(11):1820–2.
Daly AK, Aithal GP, Leathart JB, Swainsbury RA, Dang TS, Day CP. Genetic susceptibility to diclofenac-induced hepatotoxicity: contribution of UGT2B7, CYP2C8, and ABCC2 genotypes. Gastroenterology. 2007;132(1):272–81.
Metushi IG, Cai P, Zhu X, Nakagawa T, Uetrecht JP. A fresh look at the mechanism of isoniazid-induced hepatotoxicity. Clin Pharmacol Ther. 2011;89(6):911–4.
Ng CS, Hasnat A, Al Maruf A, Ahmed MU, Pirmohamed M, Day CP, et al. N-acetyltransferase 2 (NAT2) genotype as a risk factor for development of drug-induced liver injury relating to antituberculosis drug treatment in a mixed-ethnicity patient group. Eur J Clin Pharmacol. 2014;70(9):1079–86.
Singla N, Gupta D, Birbian N, Singh J. Association of NAT2, GST and CYP2E1 polymorphisms and anti-tuberculosis drug-induced hepatotoxicity. Tuberculosis (Edinb). 2014;94(3):293–8.
Wattanapokayakit S, Mushiroda T, Yanai H, Wichukchinda N, Chuchottawon C, Nedsuwan S, et al. NAT2 slow acetylator associated with anti-tuberculosis drug-induced liver injury in Thai patients. Int J Tuberc Lung Dis. 2016;20(10):1364–9.
Yuliwulandari R, Susilowati RW, Wicaksono BD, Viyati K, Prayuni K, Razari I, et al. NAT2 variants are associated with drug-induced liver injury caused by anti-tuberculosis drugs in Indonesian patients with tuberculosis. J Hum Genet. 2016;61(6):533–7.
Simon T, Becquemont L, Mary-Krause M, de Waziers I, Beaune P, Funck-Brentano C, et al. Combined glutathione-S-transferase M1 and T1 genetic polymorphism and tacrine hepatotoxicity. Clin Pharmacol Ther. 2000;67(4):432–7.
Watanabe I, Tomita A, Shimizu M, Sugawara M, Yasumo H, Koishi R, et al. A study to survey susceptible genetic factors responsible for troglitazone-associated hepatotoxicity in Japanese patients with type 2 diabetes mellitus. Clin Pharmacol Ther. 2003;73(5):435–55.
Lucena MI, Andrade RJ, Martinez C, Ulzurrun E, Garcia-Martin E, Borraz Y, et al. Glutathione S-transferase m1 and t1 null genotypes increase susceptibility to idiosyncratic drug-induced liver injury. Hepatology. 2008;48(2):588–96.
Roy B, Chowdhury A, Kundu S, Santra A, Dey B, Chakraborty M, et al. Increased risk of antituberculosis drug-induced hepatotoxicity in individuals with glutathione S-transferase M1 ‘null’ mutation. J Gastroenterol Hepatol. 2001;16(9):1033–7.
Huang YS, Su WJ, Huang YH, Chen CY, Chang FY, Lin HC, et al. Genetic polymorphisms of manganese superoxide dismutase, NAD(P)H:quinone oxidoreductase, glutathione S-transferase M1 and T1, and the susceptibility to drug-induced liver injury. J Hepatol. 2007;47(1):128–34.
Leiro V, Fernandez-Villar A, Valverde D, Constenla L, Vazquez R, Pineiro L, et al. Influence of glutathione S-transferase M1 and T1 homozygous null mutations on the risk of antituberculosis drug-induced hepatotoxicity in a Caucasian population. Liver Int. 2008;28(6):835–9.
Okada R, Maeda K, Nishiyama T, Aoyama S, Tozuka Z, Hiratsuka A, et al. Involvement of different human glutathione S-transferase Isoforms in the glutathione conjugation of reactive metabolites of troglitazone. Drug Metab Dispos. 2011.
Morgan RE, Trauner M, van Staden CJ, Lee PH, Ramachandran B, Eschenberg M, et al. Interference with bile salt export pump function is a susceptibility factor for human liver injury in drug development. Toxicol Sci. 2010;118(2):485–500.
Lang C, Meier Y, Stieger B, Beuers U, Lang T, Kerb R, et al. Mutations and polymorphisms in the bile salt export pump and the multidrug resistance protein 3 associated with drug-induced liver injury. Pharmacogenet Genomics. 2007;17(1):47–60.
Bhatnagar P, Day CP, Aithal G, Pirmohamed M, Bernal W, Daly AK. Genetic variants of hepatic transporters and susceptibility to drug induced liver injury. Toxicology. 2008;253(1–3):10.
Ulzurrun E, Stephens C, Crespo E, Ruiz-Cabello F, Ruiz-Nunez J, Saenz-Lopez P, et al. Role of chemical structures and the 1331 T > C bile salt export pump polymorphism in idiosyncratic drug-induced liver injury. Liver Int. 2013;33(9):1378–85.
Haenisch S, Zimmermann U, Dazert E, Wruck CJ, Dazert P, Siegmund W, et al. Influence of polymorphisms of ABCB1 and ABCC2 on mRNA and protein expression in normal and cancerous kidney cortex. Pharmacogenomics J. 2007;7(1):56–65.
Choi JH, Ahn BM, Yi J, Lee JH, Nam SW, Chon CY, et al. MRP2 haplotypes confer differential susceptibility to toxic liver injury. Pharmacogenet Genomics. 2007;17(6):403–15.
Ulzurrun E, Stephens C, Ruiz-Cabello F, Robles-Diaz M, Saenz-Lopez P, Hallal H, et al. Selected ABCB1, ABCB4 and ABCC2 polymorphisms do not enhance the risk of drug-induced hepatotoxicity in a Spanish cohort. PLoS ONE. 2014;9(4):e94675.
Haas DW, Bartlett JA, Andersen JW, Sanne I, Wilkinson GR, Hinkle J, et al. Pharmacogenetics of nevirapine-associated hepatotoxicity: an Adult AIDS Clinical Trials Group collaboration. Clin Infect Dis. 2006;43(6):783–6.
Ritchie MD, Haas DW, Motsinger AA, Donahue JP, Erdem H, Raffanti S, et al. Drug transporter and metabolizing enzyme gene variants and nonnucleoside reverse-transcriptase inhibitor hepatotoxicity. Clin Infect Dis. 2006;43(6):779–82.
Yuan J, Guo S, Hall D, Cammett AM, Jayadev S, Distel M, et al. Toxicogenomics of nevirapine-associated cutaneous and hepatic adverse events among populations of African, Asian, and European descent. AIDS. 2011;25(10):1271–80.
Rius M, Nies AT, Hummel-Eisenbeiss J, Jedlitschky G, Keppler D. Cotransport of reduced glutathione with bile salts by MRP4 (ABCC4) localized to the basolateral hepatocyte membrane. Hepatology. 2003;38(2):374–84.
Slot AJ, Molinski SV, Cole SP. Mammalian multidrug-resistance proteins (MRPs). Essays Biochem. 2011;50(1):179–207.
Kock K, Ferslew BC, Netterberg I, Yang K, Urban TJ, Swaan PW, et al. Risk factors for development of cholestatic drug-induced liver injury: inhibition of hepatic basolateral bile acid transporters multidrug resistance-associated proteins 3 and 4. Drug Metab Dispos. 2014;42(4):665–74.
Yang K, Woodhead JL, Watkins PB, Howell BA, Brouwer KL. Systems pharmacology modeling predicts delayed presentation and species differences in bile acid-mediated troglitazone hepatotoxicity. Clin Pharmacol Ther. 2014;96(5):589–98.
Scialis RJ, Csanaky IL, Goedken MJ, Manautou JE. Multidrug resistance-associated protein 3 plays an important role in protection against acute toxicity of diclofenac. Drug Metab Dispos. 2015;43(7):944–50.
Lagas JS, Sparidans RW, Wagenaar E, Beijnen JH, Schinkel AH. Hepatic clearance of reactive glucuronide metabolites of diclofenac in the mouse is dependent on multiple ATP-binding cassette efflux transporters. Mol Pharmacol. 2010;77(4):687–94.
Pranavchand R, Reddy BM. Genomics era and complex disorders: implications of GWAS with special reference to coronary artery disease, type 2 diabetes mellitus, and cancers. J Postgrad Med. 2016;62(3):188–98.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Daly, A.K. Are Polymorphisms in Genes Relevant to Drug Disposition Predictors of Susceptibility to Drug-Induced Liver Injury?. Pharm Res 34, 1564–1569 (2017). https://doi.org/10.1007/s11095-016-2091-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-2091-1