Abstract
Introduction
The importance of rational drug therapy is increasing with the aging of the population. Since one of the main reasons for inappropriate drug prescribing is also the “age-blind” approach, which results in ageist practices, this narrative literature review focuses on the description of the main barriers related to insufficient individualization of drug regimens associated with such age-blind approaches.
Methodology
A narrative literature review using the PubMed, WoS, Embase, and Scopus databases was conducted by the EU COST Action IS1402. Experts in different scientific fields from six countries (the Czech Republic, Spain, Portugal, Hungary, Serbia, and Turkey) worked in four specific areas: (1) underrepresentation of older adults in clinical trials and clinical and ethical consequences; (2) insufficient consideration of age-related changes and geriatric frailty in the evaluation of the therapeutic value of drugs; (3) frequent prescribing of potentially inappropriate medications (PIMs); and (4) frequent underuse of highly beneficial nonpharmacological strategies (e.g., exercise).
Results
Older patients are underrepresented in clinical trials. Therefore, rigorous observational geriatric research is needed in order to obtain evidence on the real efficacy and safety of frequently used drugs, and e.g. developed geriatric scales and frailty indexes for claims databases should help to stimulate such research. The use of PIMs, unfortunately, is still highly prevalent in Europe: 22.6% in community-dwelling older patients and 49.0% in institutionalized older adults. Specific tests to detect the majority of age-related pharmacological changes are usually not available in everyday clinical practice, which limits the estimation of drug risks and possibilities to individualize drug therapy in geriatric patients before drug prescription. Moreover, the role of some nonpharmacological strategies is highly underestimated in older adults in contrast to frequent use of polypharmacy. Among nonpharmacological strategies, particularly physical exercise was highly effective in reducing functional decline, frailty, and the risk of falls in the majority of clinical studies.
Conclusion
Several regulatory and clinical barriers contribute to insufficient knowledge on the therapeutic value of drugs in older patients, age-blind approach, and inappropriate prescribing. New clinical and observational research is needed, including data on comprehensive geriatric assessment and frailty, to document the real efficacy and safety of frequently used medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The world population is aging and advances in health technologies and science contribute to increasing longevity and prolonging of life expectancy in older patients. According to the World Health Organization (WHO), more than 20% of the world population will be over 60 years old and, particularly, the prevalence of very old patients (80+ years) will significantly increase by the year 2050 [1].
Unfortunately, drug-related problems in older patients are very frequent (up to 20–30% of hospitalizations) and often contribute to higher prevalence of frailty, disability, morbidity, mortality, and increased healthcare cost [2,3,4]. The European project PREDICT (Increasing the Participation of the Elderly in Clinical Trials, 7th Framework programme of the European Commission, 2009–2013) confirmed that there is a lack of specific evidence on the efficacy and safety of frequently used medications from randomized controlled trials (RCTs) for older patients, which represent the main medication users [5]. This problem of “evidence-biased geriatric medicine” creates a substantial barrier to appropriate drug prescribing in older adults. In 2000, Cohen, in his paper, confirmed that standard dosing for many frequently used medications recommended by SPCs (Summary Product Characteristics) should be adjusted to safer and equally effective low-dose drug regimens in the majority of older patients [6].
While, until today, ageism in the healthcare society was understood as systematic stereotyping, unfair treatment of older people or discrimination against older persons or certain age groups based on prejudices related to age itself [7], recent problems with ageism in the area of drug prescribing (conscious or unconscious) relates mainly to the “age-blind” approach [8]. This includes insufficient individualization of drug regimens with respect to age-related physiological, pathological, and pharmacological changes and with respect to the specific needs of geriatric patients. This also includes frequent prescribing of potentially inappropriate medications (PIMs) in higher age, risky polypharmacy, unnecessary exposure to medications having doubtful efficacy (e.g., pentoxifylline, low-dose piracetam), etc. [8]. Particularly, very old, frail, and disabled patients are the most disadvantaged group.
This review article focuses mainly on four particular areas of inappropriate medication use in older patients, namely:
-
Area 1. Underrepresentation of older adults in clinical trials, clinical and ethical consequences, and importance of new evidence from observational research,
-
Area 2. Insufficient consideration of the impact of age-related changes and geriatric frailty on the therapeutic value of drugs in daily clinical practice,
-
Area 3. Frequent use of high-risk medications in older patients in different settings of care, and
-
Area 4. Frequent underuse of some beneficial nonpharmacological strategies (e.g., physical exercise) in contrast to high prevalence of polypharmacy and PIM use.
In Central and Eastern Europe, a new scientific program EUROAGEISM H2020 project was funded for the period 2017–2021, called the FIP7 programme on “Inappropriate prescribing and availability of medication safety and medication management services in older patients in Europe”. The aim of this project is to describe the situation in polypharmacy and inappropriate medication use in older patients in Central and Eastern Europe (the Czech Republic, Estonia, Lithuania, Slovak Republic, Hungary, Serbia, Croatia, and Albania) in comparison to other developed countries (Ireland, Portugal, Belgium, and Turkey) and some developing countries (India and Ethiopia) [9].
Methodology
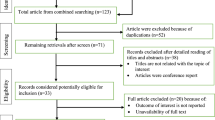
The content of this review article is based on a narrative literature review conducted with the use of the PubMed, Web of Science, Embase, and Scopus databases in the period from April 2015 to October 2018, during the active works of the WG1b working group “Healthy clinical strategies for healthy ageing” under the EU COST Action IS1402 “Ageism - a multi-national, interdisciplinary perspective” [10]. In our literature review, we focused especially on foreign scientific articles, mostly RCTs, observational studies, and systematic or narrative literature reviews, published in journals with the impact factor or peer review journals since 2000. As “ageism” is not yet recognized by many studies as a specific key word, we also used other key words selective for areas 1–4 (refer to the Introduction and corresponding with the Results subsections). These key words were: ageism, inappropriate prescribing, inappropriate drug use, potentially inappropriate medications, aged, geriatric patients, older patients, frailty, RCTs, clinical trials, underrepresentation, observational study/studies, age-related changes, negative outcomes, positive impact, nonpharmacological methods, physical activity, and physical exercise. Works on particular areas 1–4 have been summarized by experts from different fields (geriatric clinical pharmacy, pharmacology, social pharmacy, physical therapy, nursing, and pharmacoepidemiology) in cooperation with their local research teams in six countries (Czech Republic, Spain, Portugal, Hungary, Serbia, and Turkey).
Works on literature reviews were summarized by independently working research teams for sections 1–4, reviewed by other experts in the working group (minimum 2) and summarized as pre-final and final versions during face-to-face expert meetings of the EU COST Action IS1402. Cooperating research teams were not asked to record the number of searched and selected articles and sent to the center mainly pre-final and final versions of their contributions. Tables 1, 2, and 3 were summarized also from the identified literature sources.
Results
Underrepresentation of older adults in clinical trials, clinical and ethical consequences of this phenomenon, and importance of new evidence from observational research
It is known that older people respond differently to drug therapies and the risk of adverse drug events (e.g., drug interactions, adverse drug reactions, and other complications) is higher in this population due to age-related changes in pharmacokinetics and pharmacodynamics (for a comprehensive overview of pharmacological changes, see Table 1 [11,12,13]) and also due to frailty, higher degree of comorbidity, polypharmacy, and other risk factors [2,3,4, 14]. Up until now, controlled clinical trials have largely focused on the assessment of single treatment strategies or strategies applying maximally 2–3 drugs simultaneously, and mostly on non-geriatric subjects and/or subjects without multiple comorbid conditions. There is evidence of underrecruitment of older patients in clinical trials, including clinical trials testing therapies specifically used for the treatment of disorders of older age [5, 15,16,17].
Beers and colleagues (2014) from the Medical Center of Utrecht University reviewed the inclusion criteria of clinical trials (Phases II–III) performed on recently marketed medicines and concluded that these studies involved a very low proportion of older adults. Age-related exclusion criteria (comorbidity, concomitant medications, etc.) were used particularly in large clinical trials [15]. Surprisingly, an upper age limit was also applied in Parkinson disease trials, even if Parkinson’s disease is predominantly a geriatric disorder [18]. The representation of older adults remained relatively poor also in clinical trials studying treatment strategies for solid tumors and hematologic malignancies [19]. For example, trials in type 2 diabetes mellitus used an arbitrary upper age limit for participants in 65.7% of cases, even if this disorder is prevalent particularly in older age [20].
This underrepresentation of seniors in clinical trials has serious consequences for the safe and effective use of medicines in older patients. The problem has been recognized by the International Council for Harmonization (ICH) guideline ICH E7 in 1993, and amended by the European Medicines Agency (EMA) in 2010 [21], which requires the participation of a desirable proportion of older adults (> 65 years of age) in clinical trials. This guideline states that “it would be usually appropriate to include more than 100 geriatric patients in the Phase 2 and 3 databases and include patients over the entire spectrum of the geriatric patient population” [21]. However, adherence to these guidelines is still insufficient [22] and, considering the heterogeneity of the older population, the requested size of at least 100 patients is still highly underestimated for relevant pharmacoepidemiologic research.
The main reasons for the under-enrollment of older people in clinical trials are the difficulties in recruiting or retaining older patients, particularly those with chronic disorders and several health problems, or ethical problems when investigators and physicians are reluctant to expose older patients (mostly with comorbid illnesses and/or advanced disorders) to experimental, more risky therapies [17, 22]. The enrolment of older adults in clinical trials, and barriers to their participation, has gained interest in recent years; for example, the ROAR program - “Recruiting Older Adults into Research” (the US program) seeks to raise research awareness and engagement among older adults for participation in clinical trials for Alzheimer’s disease, and also for other disease conditions [23]. Moreover, the “Interventions on Frailty Working Group” developed recommendations on how to screen, recruit, evaluate, and retain frail older people in clinical trials [24, 25].
Underrepresentation of older adults in RCTs contribute to clinical and ethical dilemmas when prescribing approved “standard dosing/drug therapies” (tested on substantially healthier subjects) to geriatric patients [26]. However, with increasing utilization of e-health records and medication claims data, the role of observational research is becoming crucial in order to obtain appropriate answers on the real-life effectiveness, efficacy, and safety of medications in geriatric patients, as well as on utilization patterns and new signals of drug risks [27, 28]. Observational studies, cohort, case–control, cross-sectional, and outcome studies [29] utilizing different data sources (e.g., supplements to registration RCTs, data from practical clinical trials, patient registries, administrative claims databases, health surveys, and medical records) [30] help to answer these questions using real-world data from real geriatric patients in real conditions [28]. However, the important role of confounders in observational studies must be taken into consideration, including uncontrolled conditions of medication use by patients [27] (see also Table 1 [27, 31]).
Several examples can be stated from observational studies on geriatric patients of how risks of medicines or their inefficacy can be determined. For example, a recent study with a sample of more than 110,000 older Medicare beneficiaries conducted by Graham and colleagues published in JAMA in 2016 confirmed that the risk of intracranial bleeding and extracranial bleeding, including major gastrointestinal bleeding, was significantly higher after rivaroxaban 20 mg daily compared to dabigatran 150 mg twice daily [32]. Japanese matched-pair analyses confirmed that, most probably, the safest of these new oral anticoagulants (NOACs) when considering the risk of major bleeding and any bleeding and comparative efficacy to warfarin was apixaban 5/2.5 mg BID, while dabigatran 150/110 mg BID and rivaroxaban 15/10 mg QD were associated with significantly fewer events of major bleeding, but not any bleeding compared with warfarin [33].
The observational research and e-health systems open large possibilities to define the real therapeutic value of drugs in clinical practice in different subgroups of older patients in different settings of care with the use of huge study datasets [34]. In Europe nowadays, the main large medical datasets are THIN and CPRD (The Health Improvement Network and Clinical Practice Research Datalink, United Kingdom), the HSD-CSD-LPD database in Italy (Health Search Database-Cegedim-Strategic Data-Longitudinal Patient Database), the IPCI and PHARMO databases in the Netherlands (Integrated Primary Care Information and PHARMO Database Network), the Spanish database for pharmacoepidemiological research in primary care (BIFAP) or Information System for the Development of Primary Care Research (SIDIAP) in Spain, and the Pharmacoepidemiological Research Database (GePaRD) in Germany [34]. Some of these datasets are also linked with other data sources (e.g., socioeconomic data of patients) [27]. However, for future geriatric observational research, of high importance are mainly datasets implementing information on comprehensive geriatric assessment and frailty measures, e.g., geriatric datasets of GIFA (Italian Group for Pharmacoepidemiology) [35], interRAI acute care datasets (University of Brisbane, Queensland, Australia) [36], and interRAI integrated geriatric care datasets in Canada (e.g., CIHI, Canadian Institute for Health Information, Ontario, Canada) [37].
Insufficient consideration of the impact of age-related changes and geriatric frailty on the therapeutic value of drugs in daily clinical practice
It is well known that chronological age (65 years and older) cannot be considered a cut-off point for geriatric age because chronological aging does not correspond with physiological aging. There is an extensive inter-individual heterogeneity among older adults of the same age group in biological age and this, of course, contributes to substantial heterogeneity in therapeutic responses and outcomes among older patients [38]. It is very important to adjust the selection of medications and dosages with respect to biological age and age-related changes in drug pharmacokinetics and pharmacodynamics, of which the most known changes are listed in Table 1 [11,12,13]. Until now, the highest emphasis has been put on adjustments of dosing in relation to renal and hepatic functions, but, in the future, a more complex approach in drug selection and dosing with respect to all individual pharmacological and physiological changes in geriatric patients is necessary. Even if many age-related changes are known for decades, specific clinical tests enabling their identification are mostly missing in everyday clinical practice. Thus, they cannot be identified in advance and preventive measures are very limited (see Table 2 [11,12,13]). Because the majority of healthcare professionals care and will care in the future particularly for older patients in different settings of care, knowledge of pharmacological changes accompanying aging and associated drug risks are crucial for all healthcare professionals [39].
Besides age-related pharmacological changes, geriatric frailty further increases the heterogeneity in patients’ drug response in the same age cohort [40] and the concept of “frailty” has emerged as another measure of “biological age” and, probably, a better prognostic factor of possible poor health outcomes. Frail older people are more vulnerable to adverse drug events/outcomes [40] and the identification of geriatric frailty is an important predictive factor of possible adverse drug reactions and events [41].
Frailty is, in general, a term widely used to denote a multidimensional syndrome of loss of reserves (energy, physical ability, mobility, cognition, and health) that gives rise to an increased vulnerability of older persons to stressors (e.g., concomitant acute illnesses, hospitalizations, medical procedures) [42]. Although the biological mechanisms underlying physical frailty are still scarcely understood, common signs include fatigue, weight loss, muscle weakness, and progressive decline in physiological functions [43]. Operational criteria to define physical frailty are based on impairment in several physiological domains, including mobility, balance, muscle strength, motor processing, cognition, nutrition (often identified as nutritional status or weight loss), endurance (including feelings of fatigue and exhaustion), and physical activity [24]. Assessment of frailty significantly varies among different tools, which include: (1) frailty phenotype, based on the presence of 3 out of 5 risk factors (weight loss, exhaustion, low physical activity, muscle weakness, and slow gait) [40]; (2) the “Rothman” instrument, which is a modification of the frailty phenotype including cognition parameters [43]; (3) frailty scales and indicators, e.g., Clinical Frailty Scale (CFS); Tilburg Frailty Indicator (TFI); Groningen Frailty Indicator (GFI); and (4) frailty indexes including the number of health deficits (e.g., symptoms, signs, disabilities, laboratory, radiographic test), such as the FRAIL index (the Fatigue, Resistance, Ambulation, Illnesses and Loss of weight index) and others [44, 45]. The EMA recommends the Short Physical Performance Battery (SPPB) as an instrument to assess physical frailty in clinical trials, and gait speed as an alternative instrument [46]. As claims databases and electronic health records became important sources for observational studies, several tools have recently been developed to measure geriatric frailty in these datasets, e.g., Medicare claims-based algorithm of frailty [47], claims-based frailty index [48], claims-based frailty indicator [49], electronic frailty index [50], etc. In observational studies, these tools may help to improve the validity and reduce confounding when adverse drug outcomes are tested.
Frailty measures have also been utilized in first observational studies providing information on the efficacy and safety of drug therapies particularly in frail older patients. An observational study by Pilotto and colleagues showed that statins reduced the 3-year mortality rate even in frail older persons with cardiovascular disorders [51]. Martinez and colleagues compared, in an observational study, apixaban, dabigatran, and rivaroxaban versus warfarin in frail older patients with nonvalvular atrial fibrillation, and concluded (in contradiction to findings in the previous section) that only rivaroxaban was associated with reduced risk of stroke or systemic embolism and there were no significant differences in the risk of major bleeding for NOACs when compared to warfarin [52]. In another study using frailty tools, Droz and colleagues evaluated the efficacy and tolerability of taxane therapy in senior adults with chemonaïve metastatic castration-resistant prostate cancer and found that frail patients experienced more toxicity events but still gained significant clinical benefit from taxane therapy [53]. In another study, antidepressant use in not frail older women was associated with increased risk of incident frailty after 3 years [54].
It has also been described that the use of PIMs in older patients may contribute to a decline in physical performance and functional autonomy. Many of these PIMs cause frequent peripheral and central side effects [55,56,57] and may aggravate or worsen geriatric symptoms and syndromes (e.g., depression, cognitive impairment, urinary incontinence, weight loss, malnutrition, etc.) [55,56,57,58,59]. Interaction between the processes and exposure to PIMs may speed up the manifestation of geriatric frailty [58,59,60]. Some geriatric studies confirm that PIMs are often prescribed to frail older adults and frailty has also been documented as a specific risk factor or predictor of PIM use [59, 60].
Comprehensive geriatric assessment and care management including the assessment of geriatric frailty has already shown a benefit by reducing suboptimal prescribing in frail older inpatients and outpatients, and by reducing serious adverse drug reactions [61]. However, we still know little about how to individualize drugs with respect to the degree of geriatric frailty, and geriatric teaching books still mostly recommend “higher cautiousness” and the “start low-go slow” approach [62].
Frequent use of high-risk medications in older patients in different settings of care
Many explicit criteria of PIMs in older patients have been developed in the past 25 years, e.g., Beers criteria 2015 [55], STOPP/START criteria [56], Australian medication use and prescribing indicators [63], NORGEP criteria [64], PRISCUS and FORTA criteria [65], and others, to assist prescribers in the identification of high-risk medications in older patients and to help them reduce the excessive and unnecessary prescribing of such medications. Also, drugs having poor efficacy in older age (mostly due to processes of aging) are included on the lists of PIMs [55, 56, 63,64,65].
Despite the first explicit criteria of PIMs being published more than 20 years ago and updated many times since (at the last time in the year 2015) [55] and despite the development of national variations of these criteria in many countries [56, 63,64,65], epidemiological findings still confirm the highly prevalent use of PIMs in older adults in different settings of care, in up to 84.5% in acute care [60], up to 62.4% in noninstitutionalized seniors in the community (using five or more medications) [66], or up to 70% in older residents in nursing homes [67]. According to two systematic reviews, the weighted prevalence of the use of PIMs in Europe was 22.6% in community-dwelling older adults and 49.0% in institutionalized older people, with substantial variations across study sites and countries [68, 69]. Two larger studies using claims databases examined the trends of the use of PIMs in the outpatient setting in Ireland and in the USA (1997–2012), and showed that the prevalence of PIMs slightly increased in Ireland from 32.6% to 37.3% and decreased in the USA from 64.9% to 56.6% [70, 71]. Many of the adverse drug reactions of PIMs mimic geriatric syndromes (e.g., impaired cognition, instability and falls, malnutrition, etc.) or may cause or aggravate various geriatric problems (e.g., renal insufficiency, short memory impairment, severe bradycardias, sedation, and others) [55, 56, 60]. Despite contradictory findings, exposure to PIMs led, in some studies, to higher occurrence of geriatric symptoms, syndromes, and geriatric frailty, increased hospitalizations, healthcare costs, and decreased quality of life [57,58,59, 72,73,74].
Some publications show that PIMs are more likely to be prescribed in disadvantaged older patients or in older patients at higher risk of adverse drug events/outcomes. Older adults using polypharmacy, psychotropic drugs, or geriatric patients suffering from polymorbidity are more likely to be exposed to PIMs [75,76,77]. Factors associated with socioeconomic problems or lower socioeconomic status (e.g., having poor economic situation, not having informal carer, etc.) [76] were also significantly associated with PIM use, as well as signs of inadequate care management or care risks (e.g., having more than one prescriber [78], frequent physician visits [77], longer stay in nursing homes [68, 79], longer hospital stay [80], etc.). Based on findings of our European multicentric project ADHOC (“AgeD in Home Care”), the odds of being prescribed at least one PIM increased exponentially with increasing number of risk factors for adverse drug events [76].
Deprescribing, defined as the “process of withdrawal of an inappropriate medication, supervised by a health care professional with the goal of managing polypharmacy and improving outcomes”, can be used to reduce exposure to PIMs and to improve older patients’ safety and health outcomes [81]. Various tools of deprescribing have been published to date, e.g., specific guidelines for deprescribing, different risk scores and clinical prediction tools helping to estimate individual risk of adverse drug events, scales enabling to identify individual anticholinergic and sedative medications burden, and implicit and explicit criteria of inappropriate prescribing [82]. Fifteen deprescribing tools have been already specifically developed for frail older patients or for older adults with limited life expectancy (e.g., Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy, STOPPFrail) [83] [84]. However, a systematic review and meta-analysis of studies published by Page et al. in 2016 showed conflicting results on the impact of deprescribing on older patients’ mortality. While the mortality of older adults has been reduced in nonrandomized studies, no reduction was found in RCTs (except for a subgroup of RCTs analyzing non-educational patient-specific deprescribing interventions) [85].
Frequent underuse of some beneficial nonpharmacological strategies (e.g., physical exercise) in contrast to high prevalence of polypharmacy and PIM use
Even if the primary goal of this article was to emphasize issues related to inappropriate drug prescribing with respect to aspects of ageism, this short subsection is devoted to the underuse of some highly beneficial nonpharmacological strategies (e.g., physical exercise) in contrast to the frequent overuse of PIMs and polypharmacy. This subsection does not focus on all nonpharmacological interventions (e.g., other physiotherapeutic methods, occupational therapy, speech, language therapy, and nutritional therapy), as this was not a primary goal of this article [86], neither does it consider patient medication adherence and persistence, which are the other biggest issues of rational drug treatment [87].
There is clear, strong epidemiological evidence indicating that some nonpharmacological approaches, e.g., regular physical activity, have an important preventive effect associated with reduced rates of all-cause mortality and morbidity [88]. Regular aerobic exercise is one of the most potent strategies to preserve vascular functions with advancing age; other pharmaceutical and nutraceutical strategies can only help to further delay, minimize, or prevent arterial aging [89]. Increase in exercise capacity (increase in each one metabolic equivalent during the exercise) is associated with a 16% mean reduction in all-cause and CVS mortality in older adults [90]. These results correspond favorably with the survival benefit reached by the secondary prevention of myocardial infarction with the use of low-dose aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors [91].
Particularly, physiological functions can be preserved or improved by regular exercise and the prevalence of several disorders is significantly reduced, e.g., hypertension, stroke, metabolic syndrome, type 2 diabetes, breast and colon cancer, depression, the risk of falling, etc. [88]. A systematic review by Lozano-Montoya and colleagues showed that exercise interventions alone or with nutritional supplementation may improve physical performance in community-dwelling older patients with physical frailty and sarcopenia, but further well-designed studies are needed on this topic to also confirm the effectiveness of such interventions [92]. An RCT published by Martínez-Velilla and colleagues also showed that exercise can reverse functional decline in hospitalized older patients [93].
Moreover, polypharmacy and some medications may negatively influence functional capacity and physical activity (e.g., benzodiazepines, Z-drugs, other hypnosedatives, older generations of antidepressants, antipsychotics, etc. that are also stated on the lists of PIMs). According to the study of Heseltine and colleagues, every additional medication prescribed (OR 1.069, CI 1.016–1.124) increased the likelihood of being categorized as sedentary [94]. The results of walking speed and grip strength tests were also inversely associated with polypharmacy [95].
Contradictory are findings of studies testing the impact of physical exercise on cognitive functioning. Two systematic reviews published showed no evidence of the benefit of exercise on cognitive performance in older patients without cognitive impairment and with dementia [96, 97]. The only benefit in older patients having dementia was the improvement in the ability to perform activities of daily living, although the quality of this evidence was low [96]. A review of studies summarized by Santos-Lozano and colleagues described that regular physical activity may prevent the development of Alzheimer’s disease in older persons, but further rigorous research is needed [98].
In Table 3, we summarized, as an example, the effectiveness of some nonpharmacological, pharmacological, and combined interventions in preventing falls in older people in different settings of care. The findings are based on two Cochrane systematic reviews [99, 100] that confirmed the predominant positive role of exercise and, partially, also vitamin D supplementation.
Among available therapeutic strategies, regular physical activity is a potent “healthy clinical strategy for healthy aging”, particularly in community-residing older adults. In real clinical practice, the important role of this nonpharmacological strategy is highly underestimated and not always recommended by prescribing physicians. Appropriate exercise is available at low cost and relatively free of adverse effects [101]. It decreases the rapidity of aging, all-cause morbidity, and mortality. On the other hand, strategies helping to reduce the burden of polypharmacy and, particularly, long-term exposition to PIMs may also help to increase the physical activity in older patients.
Limitations
The first limitation of our article is that, in our narrative literature review, we focused only on a general overview of newer research findings for four particular areas listed in the Methodology section. Secondly, as the narrative literature review method was selected, we did not follow any strict guidelines for conducting systematic literature reviews. This approach introduces bias, as well as the fact that we mainly focused on newer RCTs, observational studies, and literature reviews published after the year 2000. Thirdly, even if works on specific subsections have been conducted and reviewed by experts in particular professional areas, specific selection of articles might lead to another bias. Lastly, while the aim of our article was to emphasize important problems of safe medication prescribing in older adults directly or indirectly linked to aspects of ageism, ageism is not a frequently used key word in the study databases, so we also selected articles using other key words related to safe and effective medication use in older adults.
Conclusion
Rational prescribing in older patients is accompanied by many clinical and ethical dilemmas and problems that directly or indirectly result from or in ageist practices. Clinical guidelines are often non-geriatric and evidence from recent studies do not yet provide clear answers on how to specifically individualize drug treatment (dosing, drug combinations, etc.) with respect to all age-related pharmacological and physiological changes and different stages of geriatric frailty. Clinical tests that may help to identify important age-related changes are mostly nonspecific or missing in daily clinical practice and cannot support enough highly individualized drug treatment. Moreover, new rigorous geriatric evidence is necessary not only from randomized controlled trials (RCTs), but also from geriatric observational studies. Aging of the population creates a new challenge for research and clinical practice that should focus more on effective and safe pharmacological and nonpharmacological interventions in specific cohorts of geriatric patients. Moreover, e-health and information technologies, data sharing between different settings of care, and already higher emphasis on individualized drug treatment in older patients will speed up the process of geriatrization of medicine and pharmacy.
References
World Health Organization (WHO) (2014) Ageing and life-course: facts about ageing. Available online at: http://www.who.int/ageing/about/facts/en. Accessed 10 Jul 2018
Corsonello A, Pedone C, Lattanzio F, Lucchetti M, Garasto S, Di Muzio M, Giunta S, Onder G, Di Iorio A, Volpato S, Corica F, Mussi C, Antonelli Incalzi R; Pharmacosur Veillance in the Elderly Care Study Group (2009) Potentially inappropriate medications and functional decline in elderly hospitalized patients. J Am Geriatr Soc 57(6):1007–1014. https://doi.org/10.1111/j.1532-5415.2009.02266.x
Fialová D, Desplenter F (2016) Aging of the population, clinical pharmacy services, and interdisciplinary cooperation in the optimization of pharmacotherapy in older patients. Drugs Aging 33(3):163–167. https://doi.org/10.1007/s40266-016-0361-6
Spinewine A, Fialová D, Byrne S (2012) The role of the pharmacist in optimizing pharmacotherapy in older people. Drugs Aging 29(6):495–510. https://doi.org/10.2165/11631720-000000000-00000
Crome P, Cherubini A, Oristrell J (2014) The PREDICT (increasing the participation of the elderly in clinical trials) study: the charter and beyond. Expert Rev Clin Pharmacol 7(4):457–468. https://doi.org/10.1586/17512433.2014.922864
Cohen JS (2000) Avoiding adverse reactions. Effective lower-dose drug therapies for older patients. Geriatrics 55(2):54–56, 59–60, 63–64
Achenbaum WA (2014) Robert N. Butler, MD (January 21, 1927–July 4, 2010): visionary leader. Gerontologist 54(1):6–12. https://doi.org/10.1093/geront/gnt015
Fialová D, Kummer I, Držaić M, Leppee M (2018) Ageism in medication use in older patients. In: Ayalon L, Tesch-Römer C (eds) Contemporary perspectives on ageism. Springer International Publishing. https://doi.org/10.1007/978-3-319-73820-8
EU H2020 “EUROAGEISM” project (2017–2021). Faculty of Pharmacy in Hradec Kralove Charles University - Science Portal. Home page at: https://portal.faf.cuni.cz/Research-Overview/Euroageism-project/?lang=cs-CZ. Accessed 7 Jul 2018
COST Action IS1402 on Ageism. Home page at: http://notoageism.com. Accessed 10 Jul 2018
Simonson W (2001) Introduction to the aging process. In: Delafuente JC, Steward RB (eds) Therapeutics in the elderly, 3rd edn. Harvey Whitney Books Company, Cincinnati, Ohio, 842 pp
Tan JL, Eastment JG, Poudel A, Hubbard RE (2015) Age-related changes in hepatic function: an update on implications for drug therapy. Drugs Aging 32(12):999–1008. https://doi.org/10.1007/s40266-015-0318-1
Tobias D (2004) Age-related changes in pharmacokinetics and pharmacodynamics: a review. Consult Pharm 19(8):736–739
Fialová D, Onder G (2009) Medication errors in elderly people: contributing factors and future perspectives. Br J Clin Pharmacol 67(6):641–645. https://doi.org/10.1111/j.1365-2125.2009.03419.x
Beers E, Moerkerken DC, Leufkens HG, Egberts TC, Jansen PA (2014) Participation of older people in preauthorization trials of recently approved medicines. J Am Geriatr Soc 62(10):1883–1890. https://doi.org/10.1111/jgs.13067
Konrat C, Boutron I, Trinquart L, Auleley GR, Ricordeau P, Ravaud P (2012) Underrepresentation of elderly people in randomised controlled trials. The example of trials of 4 widely prescribed drugs. PLoS One 7(3):e33559. https://doi.org/10.1371/journal.pone.0033559
McMurdo ME, Roberts H, Parker S, Wyatt N, May H, Goodman C, Jackson S, Gladman J, O’Mahony S, Ali K, Dickinson E, Edison P, Dyer C; Age and Ageing Specialty Group, NIHR, Comprehensive Clinical Research Network (2011) Improving recruitment of older people to research through good practice. Age Ageing 40(6):659–665. https://doi.org/10.1093/ageing/afr115
Fitzsimmons PR, Blayney S, Mina-Corkill S, Scott GO (2012) Older participants are frequently excluded from Parkinson’s disease research. Parkinsonism Relat Disord 18(5):585–589. https://doi.org/10.1016/j.parkreldis.2012.03.003
Denson AC, Mahipal A (2014) Participation of the elderly population in clinical trials: barriers and solutions. Cancer Control 21(3):209–214. https://doi.org/10.1177/107327481402100305
Cruz-Jentoft AJ, Carpena-Ruiz M, Montero-Errasquín B, Sánchez-Castellano C, Sánchez-García E (2013) Exclusion of older adults from ongoing clinical trials about type 2 diabetes mellitus. J Am Geriatr Soc 61(5):734–738. https://doi.org/10.1111/jgs.12215
European Medicines Agency (2010) ICH topic E7. Studies in support of special populations: geriatrics questions and answers. Available online at: https://www.ema.europa.eu/documents/scientific-guideline/ich-e-7-studies-support-special-populations-geriatrics-questions-answers-step-5_en.pdf. Accessed 2 Jul 2018
McMurdo ME (2012) Older people in clinical trials. No more arbitrary upper age limits for clinical research. BMJ 344:e4040. https://doi.org/10.1136/bmj.e4040
National Institute on Aging (NIA) (2015) Clinical trials. Recruiting older adults into research (ROAR) toolkit. Home page at: https://www.nia.nih.gov/health/recruiting-older-adults-research-roar-toolkit. Accessed 2 Jul 2018
Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB Jr, Walston JD; Interventions on Frailty Working Group (2004) Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc 52(4):625–634. https://doi.org/10.1111/j.1532-5415.2004.52174.x
Witham MD, McMurdo ME (2007) How to get older people included in clinical studies. Drugs Aging 24(3):187–196. https://doi.org/10.2165/00002512-200724030-00002
De Spiegeleer B, Wynendaele E, Bracke N, Veryser L, Taevernier L, Degroote A, Stalmans S (2016) Regulatory development of geriatric medicines: to GIP or not to GIP? Ageing Res Rev 27:23–36. https://doi.org/10.1016/j.arr.2016.02.004
Cohen AT, Goto S, Schreiber K, Torp-Pedersen C (2015) Why do we need observational studies of everyday patients in the real-life setting? Eur Heart J Suppl 17:D2–D8. https://doi.org/10.1093/eurheartj/suv035
Poscia A, Collamati A, Milovanovic S, Vetrano DL, Liotta G, Petitti T, Di Pietro ML, Magnavita N, Ricciardi W, Cherubini A, Onder G (2017) Methodological issues in the observational studies conducted in older population: a narrative review. Epidemiol Biostat Public Health 14(2). https://doi.org/10.2427/12627
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4(10):e296. https://doi.org/10.1371/journal.pmed.0040296
Garrison LP Jr, Neumann PJ, Erickson P, Marshall D, Mullins CD (2007) Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value Health 10(5):326–335. https://doi.org/10.1111/j.1524-4733.2007.00186.x
Booth CM, Tannock IF (2014) Randomised controlled trials and population-based observational research: partners in the evolution of medical evidence. Br J Cancer 110(3):551–555. https://doi.org/10.1038/bjc.2013.725
Graham DJ, Reichman ME, Wernecke M, Hsueh YH, Izem R, Southworth MR, Wei Y, Liao J, Goulding MR, Mott K, Chillarige Y, MaCurdy TE, Worrall C, Kelman JA (2016) Stroke, bleeding, and mortality risks in elderly Medicare beneficiaries treated with dabigatran or rivaroxaban for nonvalvular atrial fibrillation. JAMA Intern Med 176(11):1662–1671. https://doi.org/10.1001/jamainternmed.2016.5954
Kohsaka S, Murata T, Izumi N, Katada J, Wang F, Terayama Y (2017) Bleeding risk of apixaban, dabigatran, and low-dose rivaroxaban compared with warfarin in Japanese patients with non-valvular atrial fibrillation: a propensity matched analysis of administrative claims data. Curr Med Res Opin 33(11):1955–1963. https://doi.org/10.1080/03007995.2017.1374935
Damiani A, Onder G, Valentini V (2018) Large databases (big data) and evidence-based medicine. Eur J Intern Med 53:1–2. https://doi.org/10.1016/j.ejim.2018.05.019
Onder G, Vetrano DL, Cherubini A, Fini M, Mannucci PM, Marengoni A, Monaco A, Nobili A, Pecorelli S, Russo P, Vitale C, Bernabei R (2014) Prescription drug use among older adults in Italy: a country-wide perspective. J Am Med Dir Assoc 15(7):531.e11–531.e15. https://doi.org/10.1016/j.jamda.2014.04.005
Hubbard RE, Peel NM, Samanta M, Gray LC, Fries BE, Mitnitski A, Rockwood K (2015) Derivation of a frailty index from the interRAI acute care instrument. BMC Geriatr 15:27. https://doi.org/10.1186/s12877-015-0026-z
Access data and reports. Seniors and ageing. Canadian Institute for Health Information (CIHI). Home page at: https://www.cihi.ca/en/access-data-reports/results?f%5B0%5D=field_primary_theme%3A2054. Accessed 14 Nov 2018
Fielding RA (2015) A summary of the biological basis of frailty. In: Proceedings of the 83rd Nestlé Nutrition Institute Workshop, Barcelona, March 2014. https://doi.org/10.1159/000430966
Keijsers CJ, van Hensbergen L, Jacobs L, Brouwers JR, de Wildt DJ, ten Cate OT, Jansen PA (2012) Geriatric pharmacology and pharmacotherapy education for health professionals and students: a systematic review. Br J Clin Pharmacol 74(5):762–773. https://doi.org/10.1111/j.1365-2125.2012.04268.x
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA; Cardiovascular Health Study Collaborative Research Group (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156
Cullinan S, O’Mahony D, O’Sullivan D, Byrne S (2016) Use of a frailty index to identify potentially inappropriate prescribing and adverse drug reaction risks in older patients. Age Ageing 45(1):115–120. https://doi.org/10.1093/ageing/afv166
Rockwood K (2005) Frailty and its definition: a worthy challenge. J Am Geriatr Soc 53(6):1069–1070. https://doi.org/10.1111/j.1532-5415.2005.53312.x
Rothman MD, Leo-Summers L, Gill TM (2008) Prognostic significance of potential frailty criteria. J Am Geriatr Soc 56(12):2211–2216. https://doi.org/10.1111/j.1532-5415.2008.02008.x
Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 1:323–336. https://doi.org/10.1100/tsw.2001.58
Dent E, Kowal P, Hoogendijk EO (2016) Frailty measurement in research and clinical practice: a review. Eur J Intern Med 31:3–10. https://doi.org/10.1016/j.ejim.2016.03.007
European Medicines Agency (2018) Reflection paper on physical frailty: instruments for baseline characterisation of older populations in clinical trials. Available online at: https://www.ema.europa.eu/documents/scientific-guideline/reflection-paper-physical-frailty-instruments-baseline-characterisation-older-populations-clinical_en.pdf. Accessed 5 Nov 2018
Cuthbertson CC, Kucharska-Newton A, Faurot KR, Stürmer T, Jonsson Funk M, Palta P, Windham BG, Thai S, Lund JL (2018) Controlling for frailty in pharmacoepidemiologic studies of older adults: validation of an existing Medicare claims-based algorithm. Epidemiology 29(4):556–561. https://doi.org/10.1097/ede.0000000000000833
Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J (2018) Measuring frailty in Medicare data: development and validation of a claims-based frailty index. J Gerontol A Biol Sci Med Sci 73(7):980–987. https://doi.org/10.1093/gerona/glx229
Segal JB, Chang H-Y, Du Y, Walston JD, Carlson MC, Varadhan R (2017) Development of a claims-based frailty indicator anchored to a well-established frailty phenotype. Med Care 55(7):716–722. https://doi.org/10.1097/mlr.0000000000000729
Clegg A, Bates C, Young J, Ryan R, Nichols L, Teale EA, Mohammed MA, Parry J, Marshall T (2018) Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 47(2):319. https://doi.org/10.1093/ageing/afx001
Pilotto A, Gallina P, Panza F, Copetti M, Cella A, Cruz-Jentoft A, Daragjati J, Ferrucci L, Maggi S, Mattace-Raso F, Paccalin M, Polidori MC, Topinkova E, Trifirò G, Welmer AK, Strandberg T, Marchionni N; MPI_AGE Project Investigators (2016) Relation of statin use and mortality in community-dwelling frail older patients with coronary artery disease. Am J Cardiol 118(11):1624–1630. https://doi.org/10.1016/j.amjcard.2016.08.042
Martinez BK, Sood NA, Bunz TJ, Coleman CI (2018) Effectiveness and safety of apixaban, dabigatran, and rivaroxaban versus warfarin in frail patients with nonvalvular atrial fibrillation. J Am Heart Assoc 7(8). pii: e008643. https://doi.org/10.1161/jaha.118.008643
Droz JP, Efstathiou E, Yildirim A, Cabrera P, Soo Kim C, Horchani A, Heidenreich A, Rinck-Junior JA, Hitier S, Ӧzen H (2016) First-line treatment in senior adults with metastatic castration-resistant prostate cancer: a prospective international registry. Urol Oncol 34(5):234.e21–234.e29. https://doi.org/10.1016/j.urolonc.2015.12.005
Lakey SL, LaCroix AZ, Gray SL, Borson S, Williams CD, Calhoun D, Goveas JS, Smoller JW, Ockene JK, Masaki KH, Coday M, Rosal MC, Woods NF (2012) Antidepressant use, depressive symptoms, and incident frailty in women aged 65 and older from the Women’s Health Initiative Observational Study. J Am Geriatr Soc 60(5):854–861. https://doi.org/10.1111/j.1532-5415.2012.03940.x
American Geriatrics Society 2015 Beers Criteria Update Expert Panel (2015) American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 63(11):2227–2246. https://doi.org/10.1111/jgs.13702
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218. https://doi.org/10.1093/ageing/afu145
Tosato M, Landi F, Martone AM, Cherubini A, Corsonello A, Volpato S, Bernabei R, Onder G; Investigators of the CRIME Study (2014) Potentially inappropriate drug use among hospitalised older adults: results from the CRIME study. Age Ageing 43(6):767–773. https://doi.org/10.1093/ageing/afu029
Landi F, Russo A, Liperoti R, Barillaro C, Danese P, Pahor M, Bernabei R, Onder G (2007) Impact of inappropriate drug use on physical performance among a frail elderly population living in the community. Eur J Clin Pharmacol 63(8):791–799. https://doi.org/10.1007/s00228-007-0321-5
Poudel A, Peel NM, Nissen L, Mitchell C, Gray LC, Hubbard RE (2014) Potentially inappropriate prescribing in older patients discharged from acute care hospitals to residential aged care facilities. Ann Pharmacother 48(11):1425–1433. https://doi.org/10.1177/1060028014548568
Jensen LD, Andersen O, Hallin M, Petersen J (2014) Potentially inappropriate medication related to weakness in older acute medical patients. Int J Clin Pharm 36(3):570–580. https://doi.org/10.1007/s11096-014-9940-y
Schmader KE, Hanlon JT, Pieper CF, Sloane R, Ruby CM, Twersky J, Francis SD, Branch LG, Lindblad CI, Artz M, Weinberger M, Feussner JR, Cohen HJ (2004) Effects of geriatric evaluation and management on adverse drug reactions and suboptimal prescribing in the frail elderly. Am J Med 116(6):394–401. https://doi.org/10.1016/j.amjmed.2003.10.031
Reuben DB, Herr KA, Pacala JT, Pollock BG, Potter JF, Semla TP (2017) Geriatrics at your fingertips: 2017, 19th edn. American Geriatrics Society, New York
Basger BJ, Chen TF, Moles RJ (2012) Application of a prescribing indicators tool to assist in identifying drug-related problems in a cohort of older Australians. Int J Pharm Pract 20(3):172–182. https://doi.org/10.1111/j.2042-7174.2011.00177.x
Rognstad S, Brekke M, Fetveit A, Spigset O, Wyller TB, Straand J (2009) The Norwegian General Practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients. A modified Delphi study. Scand J Prim Health Care 27(3):153–159. https://doi.org/10.1080/02813430902992215
Wickop B, Härterich S, Sommer C, Daubmann A, Baehr M, Langebrake C (2016) Potentially inappropriate medication use in multimorbid elderly inpatients: differences between the FORTA, PRISCUS and STOPP ratings. Drugs 3(3):317–325. https://doi.org/10.1007/s40801-016-0085-2
Popović B, Quadranti NR, Matanović SM, Lisica ID, Ljubotina A, Duliba DP, Vlahović-Palčevski V (2014) Potentially inappropriate prescribing in elderly outpatients in Croatia. Eur J Clin Pharmacol 70(6):737–744. https://doi.org/10.1007/s00228-014-1667-0
O’Sullivan DP, O’Mahony D, Parsons C, Hughes C, Murphy K, Patterson S, Byrne S (2013) A prevalence study of potentially inappropriate prescribing in Irish long-term care residents. Drugs Aging 30(1):39–49. https://doi.org/10.1007/s40266-012-0039-7
Morin L, Laroche ML, Texier G, Johnell K (2016) Prevalence of potentially inappropriate medication use in older adults living in nursing homes: a systematic review. J Am Med Dir Assoc 17(9):862.e1–862.e9. https://doi.org/10.1016/j.jamda.2016.06.011
Tommelein E, Mehuys E, Petrovic M, Somers A, Colin P, Boussery K (2015) Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol 71(12):1415–1427. https://doi.org/10.1007/s00228-015-1954-4
Jirón M, Pate V, Hanson LC, Lund JL, Jonsson Funk M, Stürmer T (2016) Trends in prevalence and determinants of potentially inappropriate prescribing in the United States: 2007 to 2012. J Am Geriatr Soc 64(4):788–797. https://doi.org/10.1111/jgs.14077
Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T (2015) Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open 5(9):e008656. https://doi.org/10.1136/bmjopen-2015-008656
Brown JD, Hutchison LC, Li C, Painter JT, Martin BC (2016) Predictive validity of the Beers and Screening Tool of Older Persons’ potentially inappropriate Prescriptions (STOPP) criteria to detect adverse drug events, hospitalizations, and emergency department visits in the United States. J Am Geriatr Soc 64(1):22–30. https://doi.org/10.1111/jgs.13884
Cahir C, Moriarty F, Teljeur C, Fahey T, Bennett K (2014) Potentially inappropriate prescribing and vulnerability and hospitalization in older community-dwelling patients. Ann Pharmacother 48(12):1546–1554. https://doi.org/10.1177/1060028014552821
Wallace E, McDowell R, Bennett K, Fahey T, Smith SM (2017) Impact of potentially inappropriate prescribing on adverse drug events, health related quality of life and emergency hospital attendance in older people attending general practice: a prospective cohort study. J Gerontol A Biol Sci Med Sci 72(2):271–277. https://doi.org/10.1093/gerona/glw140
Blanco-Reina E, García-Merino MR, Ocaña-Riola R, Aguilar-Cano L, Valdellós J, Bellido-Estévez I, Ariza-Zafra G (2016) Assessing potentially inappropriate prescribing in community-dwelling older patients using the updated version of STOPP-START criteria: a comparison of profiles and prevalences with respect to the original version. PLoS One 11(12):e0167586. https://doi.org/10.1371/journal.pone.0167586
Fialová D, Topinková E, Gambassi G, Finne-Soveri H, Jónsson PV, Carpenter I, Schroll M, Onder G, Sørbye LW, Wagner C, Reissigová J, Bernabei R; AdHOC Project Research Group (2005) Potentially inappropriate medication use among elderly home care patients in Europe. JAMA 293(11):1348–1358. https://doi.org/10.1001/jama.293.11.1348
Zhan C, Sangl J, Bierman AS, Miller MR, Friedman B, Wickizer SW, Meyer GS (2001) Potentially inappropriate medication use in the community-dwelling elderly: findings from the 1996 medical expenditure panel survey. JAMA 286(22):2823–2829
Hajjar ER, Hanlon JT, Sloane RJ, Lindblad CI, Pieper CF, Ruby CM, Branch LC, Schmader KE (2005) Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc 53(9):1518–1523. https://doi.org/10.1111/j.1532-5415.2005.53523.x
Chen LL, Tangiisuran B, Shafie AA, Hassali MA (2012) Evaluation of potentially inappropriate medications among older residents of Malaysian nursing homes. Int J Clin Pharm 34(4):596–603. https://doi.org/10.1007/s11096-012-9651-1
Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF; Collaborative Working Group (2013) Frequency of inappropriate medication prescription in hospitalized elderly patients in Italy. PLoS One 8(12):e82359. https://doi.org/10.1371/journal.pone.0082359
Reeve E, Gnjidic D, Long J, Hilmer S (2015) A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol 80(6):1254–1268
Scott I, Anderson K, Freeman C (2017) Review of structured guides for deprescribing. Eur J Hosp Pharm 24(1):51–57. https://doi.org/10.1136/ejhpharm-2015-000864
Lavan AH, Gallagher P, Parsons C, O’Mahony D (2017) STOPPFrail (Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy): consensus validation. Age Ageing 46(4):600–607. https://doi.org/10.1093/ageing/afx005
Thompson W, Lundby C, Graabaek T, Nielsen DS, Ryg J, Søndergaard J, Pottegård A (2018) Tools for deprescribing in frail older persons and those with limited life expectancy: a systematic review. J Am Geriatr Soc. https://doi.org/10.1111/jgs.15616
Page AT, Clifford RM, Potter K, Schwartz D, Etherton-Beer CD (2016) The feasibility and effect of deprescribing in older adults on mortality and health: a systematic review and meta-analysis. Br J Clin Pharmacol 82(3):583–623. https://doi.org/10.1111/bcp.12975
Abraha I, Cruz-Jentoft A, Soiza RL, O’Mahony D, Cherubini A (2015) Evidence of and recommendations for non-pharmacological interventions for common geriatric conditions: the SENATOR-ONTOP systematic review protocol. BMJ Open 5(1):e007488. https://doi.org/10.1136/bmjopen-2014-007488
Jankowska-Polańska B, Zamęta K, Uchmanowicz I, Szymańska-Chabowska A, Morisky D, Mazur G (2018) Adherence to pharmacological and non-pharmacological treatment of frail hypertensive patients. J Geriatr Cardiol 15(2):153–161. https://doi.org/10.11909/j.issn.1671-5411.2018.02.002
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT; Lancet Physical Activity Series Working Group (2012) Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 380(9838):219–229. https://doi.org/10.1016/s0140-6736(12)61031-9
Seals DR (2014) Edward F. Adolph distinguished lecture: the remarkable anti-aging effects of aerobic exercise on systemic arteries. J Appl Physiol (1985) 117(5):425–439. https://doi.org/10.1152/japplphysiol.00362.2014
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301(19):2024–2035. https://doi.org/10.1001/jama.2009.681
Boden WE, Franklin BA, Wenger NK (2013) Physical activity and structured exercise for patients with stable ischemic heart disease. JAMA 309(2):143–144. https://doi.org/10.1001/jama.2012.128367
Lozano-Montoya I, Correa-Pérez A, Abraha I, Soiza RL, Cherubini A, O’Mahony D, Cruz-Jentoft AJ (2017) Nonpharmacological interventions to treat physical frailty and sarcopenia in older patients: a systematic overview—the SENATOR Project ONTOP Series. Clin Interv Aging 12:721–740. https://doi.org/10.2147/cia.S132496
Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, López Sáez de Asteasu M, Lucia A, Galbete A, García-Baztán A, Alonso-Renedo J, González-Glaría B, Gonzalo-Lázaro M, Apezteguía Iráizoz I, Gutiérrez-Valencia M, Rodríguez-Mañas L, Izquierdo M (2018) Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2018.4869
Heseltine R, Skelton DA, Kendrick D, Morris RW, Griffin M, Haworth D, Masud T, Iliffe S (2015) “Keeping Moving”: factors associated with sedentary behaviour among older people recruited to an exercise promotion trial in general practice. BMC Fam Pract 16:67. https://doi.org/10.1186/s12875-015-0284-z
Sganga F, Vetrano DL, Volpato S, Cherubini A, Ruggiero C, Corsonello A, Fabbietti P, Lattanzio F, Bernabei R, Onder G (2014) Physical performance measures and polypharmacy among hospitalized older adults: results from the CRIME study. J Nutr Health Aging 18(6):616–621. https://doi.org/10.1007/s12603-014-0029-z
Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S (2015) Exercise programs for people with dementia. Cochrane Database Syst Rev (4):CD006489. https://doi.org/10.1002/14651858.CD006489.pub4
Young J, Angevaren M, Rusted J, Tabet N (2015) Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev (4):CD005381. https://doi.org/10.1002/14651858.CD005381.pub4
Santos-Lozano A, Pareja-Galeano H, Sanchis-Gomar F, Quindós-Rubial M, Fiuza-Luces C, Cristi-Montero C, Emanuele E, Garatachea N, Lucia A (2016) Physical activity and Alzheimer disease: a protective association. Mayo Clin Proc 91(8):999–1020. https://doi.org/10.1016/j.mayocp.2016.04.024
Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N (2018) Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 9:CD005465. https://doi.org/10.1002/14651858.CD005465.pub4
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev (9):CD007146. https://doi.org/10.1002/14651858.CD007146.pub3
Fiuza-Luces C, Garatachea N, Berger NA, Lucia A (2013) Exercise is the real polypill. Physiology (Bethesda) 28(5):330–358. https://doi.org/10.1152/physiol.00019.2013
Acknowledgements
We thank the members of the WG1b group “Healthy clinical strategies for healthy ageing” of the EU COST Action IS 1402 (205-2018) “Ageism - a multi-national, interdisciplinary perspective”, the chairs of this EU COST prof. Liat Ayalon and prof. Clemens Toesch-Römer, and the research group “Ageing and Changes in the Therapeutic Value of Drugs in the AgeD” (Chair: Fialová D., PharmD, PhD, BCCP) under the scientific program PROGRESS Q42 at the Faculty of Pharmacy, Charles University, Czech Republic. We also acknowledge to all research teams participating in the EUROAGEISM H2020 project, Horizon 2020-MSCA-ITN-764632 (2017–2021).
Grant support
The work has been supported by the EU COST Action IS1402 initiative “Ageism - a multi-national, interdisciplinary perspective” (2015–2018), the EUROAGEISM H2020 project no. 764632, Horizon 2020-MSCA-ITN -764632 (2017–2021), and by the scientific program PROGRESS Q42 at the Department of Social and Clinical Pharmacy, Faculty of Pharmacy, Charles University, Czech Republic.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors have been supported in participation at meetings of the EU COST Action IS1402 initiative “Ageism - interprofessional, multidisciplinary perspectives” (April 2015–October 2018). Dr. Fialová has been supported as Chair of the FIP7 program of the EUROAGEISM H2020 project, no. 764632, Horizon 2020-MSCA-ITN (2017–2021), and by the scientific program PROGRESS Q42 at the Faculty of Pharmacy in Hradec Králové, Charles University, Czech Republic.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fialová, D., Laffon, B., Marinković, V. et al. Medication use in older patients and age-blind approach: narrative literature review (insufficient evidence on the efficacy and safety of drugs in older age, frequent use of PIMs and polypharmacy, and underuse of highly beneficial nonpharmacological strategies). Eur J Clin Pharmacol 75, 451–466 (2019). https://doi.org/10.1007/s00228-018-2603-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-018-2603-5