Abstract
Background
Clinical guidance is needed to initiate, continue, and discontinue drug treatments near the end of life.
Aim
To identify drugs and drug classes most often adequate, questionable, or inadequate for older people at the end of life.
Design
Delphi consensus survey.
Setting/participants
Forty European experts in geriatrics, clinical pharmacology, and palliative medicine from 10 different countries. Panelists were asked to characterize drug classes as “often adequate,” “questionable,” or “often inadequate” for use in older adults aged 75 years or older with an estimated life expectancy of ≤ 3 months. We distinguished the continuation of a drug class that was previously prescribed from the initiation of a new drug. Consensus was considered achieved for a given drug or drug class if the level of agreement was ≥ 75%.
Results
The expert panel reached consensus on a set of 14 drug classes deemed as “often adequate,” 28 drug classes deemed “questionable,” and 10 drug classes deemed “often inadequate” for continuation during the last 3 months of life. Regarding the initiation of new drug treatments, the panel reached consensus on a set of 10 drug classes deemed “often adequate,” 23 drug classes deemed “questionable,” and 23 drug classes deemed “often inadequate”. Consensus remained unachieved for some very commonly prescribed drug treatments (e.g., proton-pump inhibitors, furosemide, haloperidol, olanzapine, zopiclone, and selective serotonin reuptake inhibitors).
Conclusion
In the absence of high-quality evidence from randomized clinical trials, these consensus-based criteria provide guidance to rationalize drug prescribing for older adults near the end of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Near the end of life, drug treatments should focus on palliative goals of care by gradually reducing disease-oriented therapy and prioritizing symptom relief and comfort [1,2,3]. Yet, polypharmacy is commonplace during the final months of life of older adults, fueled not only by the surge of analgesics and other symptomatic drugs but also by the continuation of medications prescribed for the long-term prevention of chronic diseases [4,5,6,7]. This highlights the need to rationalize drug prescribing near the end of life [8, 9].
Drugs are usually considered as potentially inappropriate when the risk of harmful effects outweighs their expected benefit, or when there exist a safer, better tolerated, or more effective alternative [10]. Several assessment tools have been developed over the past two decades to help prescribers identify potentially inappropriate drugs, including the Beers and the STOPP/START criteria [11, 12]. However, these tools are not designed to evaluate the quality of drug prescribing in the context of end-of-life care. Drug classes considered as potentially inappropriate with regard to their risk of side effects (e.g., opioids, benzodiazepines, scopolamine) may be indicated for the management of distressing symptoms during the final weeks of life. Conversely, drugs appropriate for older adults in general may be of little benefit and present a higher risk of harmful effects near the end of life. Holmes et al. have therefore proposed a prescribing model that goes beyond the pharmacological focus of existing criteria [13]. They suggest that physicians should consider stopping otherwise appropriate medications when the time needed to achieve a clinically significant outcome is longer than the remaining life expectancy, or when the treatment target is no longer aligned with the preferred goals of care.
Deprescribing has gained considerable attention in geriatric medicine [14, 15]. However, there is limited evidence to assess the benefits and risks of discontinuing drug treatments in older adults with limited life expectancy [16, 17]. Older adults with advanced illness and multiple chronic diseases are typically excluded from randomized controlled trials and well-designed prospective cohort studies are scarce. Clinical guidance must therefore mostly rely on expert consensus. Yet, until now most initiatives have focused on a single disease (e.g., dementia [18], cancer [19,20,21]), or have adopted a broader perspective encompassing all frail older adults without specifically targeting the final months of life (e.g., STOPPFrail [22], NORGEP-NH [23]). While the former have a limited generalizability, the latter may prove difficult to apply in real-world clinical practice because of the considerable uncertainty that comes with estimating the life expectancy of frail older adults. Survival predictions made by physicians in routine clinical practice are often over-optimistic, and are notoriously unreliable when the actual survival exceeds a few months or weeks [24,25,26]. One way to reduce this prognostic uncertainty is to focus on a shorter period where end-of-life care needs are easier to ascertain.
The purpose of this study was to develop a consensus about prescription drugs that are most likely adequate, questionable, or inadequate for people aged 75 years or older with an estimated life expectancy of ≤ 3 months. Our goal was thereby twofold: (i) to provide guidance for prescribers caring for older adults nearing the end of life and (ii) to develop a tool that could be used to assess the quality of drug prescribing in pharmacoepidemiological studies based on routinely collected data.
Methods
Selection of panelists
The consensus panel consisted of European clinicians and researchers with in-depth expertise of drug prescribing in older adults at the end of life. We only included healthcare professionals with clinical experience in either palliative medicine, geriatrics, family medicine, or pharmacology. Potentially eligible participants were identified through a literature review, selecting principal investigators and principal authors of relevant original studies on the topic. To broaden the panel of experts, we also asked key informants to provide names of potential participants. Age, gender and occupational and geographical balance were ensured during the selection of panelists. Eligible candidates were emailed an invitation presenting the study aims and the Delphi process. Participants who agreed to participate were required to sign an electronic consent form and were informed that they could withdraw from the survey at any time. No financial incentive was provided.
Selection of criteria
We conducted a systematic review of the literature updating the findings from Todd et al. [1] to identify therapeutic classes or individual drugs considered as potentially adequate or inadequate for use in the context of end-of-life care. A preliminary list of 49 drug classes was developed by a research team consisting of two clinical pharmacologists, one pharmacist, and one geriatrician. We included items at the pharmacological subgroup level of the Anatomical Therapeutic Chemical (ATC) classification rather than at the individual drug level (e.g., “A02B Drugs for peptic ulcer and gastro-oesophageal reflux disease” instead of “A02BC01 omeprazole”). Our study focused on drug treatments, and did therefore not include other types of medical treatments such as herbal drugs, mechanical ventilation, or tube feeding. However, because blood transfusion is a therapeutic alternative to drug treatments in the management of anemia and thrombocytopenia, it was also included.
Delphi process
The candidate set of drug classes was submitted to the panelists through a web-based Delphi survey. Delphi techniques are used to elicit opinion and gain consensus from a group of experts on a subject for which there is no or insufficient evidence-based information [27]. The process consists of a structured and iterative survey of at least two rounds, which continues until consensus is reached. Panelists receive feedback between each round. Delphi panels have been used extensively for generating lists of potentially inappropriate drugs in older adults [28,29,30,31,32].
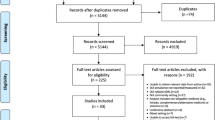
The first Delphi round took place between June 1 and August 31, 2016 (Fig. 1). Panelists were asked to rate to what extent the prescription of different pharmacological classes included in the preliminary list seemed adequate or inadequate in older adults aged 75 years or older with an estimated life expectancy of ≤ 3 months, regardless of their underlying condition and regardless of the clinical indication of the drug. They were instructed to take into account not only the need to avoid adverse events and to ensure optimal symptom management, but also the potential futility of treatments near the end of life. We distinguished two scenarios: on the one hand, the continuation of a drug class that was previously prescribed, and on the other hand, the initiation of a new drug class. For each drug class, participants indicated their opinion on a 5-point, non-numerical Likert scale: “Always inadequate,” “Often inadequate,” “Questionable,” “Often adequate,” and “Always adequate”. They also had the possibility to suggest the inclusion of more precise drug classes in the following rounds (e.g., to break-down a large drug class into several ones), and to add drugs or drug classes that were not initially included. Participants received up to three email reminders. Consensus was considered as achieved if at least 75% of participants rated a given drug class as either “Always/often inadequate” or “Always/often adequate” for continuation and initiation, respectively. Drugs for which consensus was reached at this stage were not reviewed again during the subsequent round.
During the second round (November 1 to December 31, 2016), panelists were provided with feedback consisting of detailed results for each item rated during round 1 as well as comments and requests from the other participants. They were asked to re-rate drug classes for which consensus was not achieved previously, and to rate drug classes or subgroups that were proposed during the first round. Results were analyzed to evaluate the level of agreement for each criterion. The categorization of drug classes is illustrated by the diagram presented in Fig. 2. Only drugs and drug classes for which the level of agreement was at least 75% were included in the final list of criteria. Drug classes with a moderate (65–74%) or low (< 65%) level of agreement are presented in Appendix Table in the ESM. The regional ethical review Board in Stockholm, Sweden, approved the study (decision no. 2015/1341-31/1).
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available due to privacy issues, but are available from the corresponding author on reasonable request.
Results
Participating experts
A total of 58 potential participants were invited, of whom 40 (69%) agreed to be part of the consensus panel and responded in the first Delphi round. Of them, 39 also participated in the second round. As shown in Table 1, 58% of panelists were female, and 85% had at least 10 years of clinical experience. Although participants were predominantly geriatricians (33%) or palliative care physicians (30%), the panel also included seven general practitioners, seven pharmacists or clinical pharmacologists, and one palliative care psychiatrist. Participants were located in 10 different European countries.
Continuation of previously prescribed drug classes
During the first Delphi round, panelists reached consensus to consider the continuation of seven drug classes as “often adequate” and four drug classes as “often inadequate”. They asked for 33 suggested drug classes to be broken-down into 96 more detailed sub-classes and suggested the inclusion of 13 additional drugs in the following round (e.g., mirtazapine, haloperidol, metoclopramide). As a result, the candidate set compiled for the second Delphi round was composed of a total of 114 distinct drugs and drug classes. Consensus was achieved to consider the continuation of 9 drug classes as “often adequate,” 44 drug classes “questionable,” and 8 drug classes “often inadequate”. To facilitate the interpretation of the findings, drugs were then categorized into homogenous ATC classes, which resulted in a final list of 14 drugs or drug classes considered “often adequate,” 28 considered “questionable,” and 10 considered “often inadequate” for continuation in older adults with ≤ 3 months life expectancy (Table 2). In addition, 29 drug classes obtained only a moderate consensus (level of agreement 65 to 74%) and were therefore not included in the final set of criteria. Due to a low level of agreement (< 65%), consensus remained unachieved for 24 drug classes (Appendix Table in the ESM).
Initiation of new drug classes
Consensus was achieved during the first Delphi round to consider the initiation of 4 drug classes as “often adequate” and 11 drug classes as “often inadequate” (out of the 49 included in the initial candidate set). The participants suggested that 22 drug classes should be presented at a more detailed level and asked for the inclusion of 13 additional drugs or drug classes. This resulted in a candidate set of 85 drugs and drug classes to be evaluated during the second Delphi round. Panelists reached consensus for 7 drug classes deemed “often adequate,” 39 drug classes deemed “questionable,” and 24 drug classes deemed “often inadequate”. After regrouping these items into homogenous ATC classes, the final list was composed of 10 drugs or drug classes considered “often adequate,” 23 considered “questionable,” and 23 considered “often inadequate” for initiation in older adults with ≤ 3 months life expectancy (Table 3). Among drugs for which consensus was not reached, the level of agreement between experts was moderate (65–74%) for 15 drug classes and low (< 65%) for 25 drug classes, including proton-pump inhibitors, furosemide, haloperidol, olanzapine, zopiclone, zolpidem, and selective serotonin reuptake inhibitors (see Appendix Table in the ESM).
Discussion
In this study, 40 European experts in geriatrics, palliative medicine, general practice, pharmacy, and clinical pharmacology from 10 different countries provided their professional opinion drug prescribing in older adults aged 75 years or older with an estimated life expectancy of ≤ 3 months. Panelists were given the opportunity to differentiate between the continuation and the initiation of drug therapy. Based on these results, we developed a consensus list of adequate, questionable, and inadequate drugs for older adults near the end of life.
Drug classes considered as often adequate by a qualified majority of panelists (≥ 75% agreement) are mostly prescribed for symptom management and comfort, e.g., analgesics, antinauseants, anxiolytics, drugs for constipation, levodopa. This is in line with the palliative goals of care often established near the end of life, and medications classified as often adequate are in fact highly congruent with the list of essential medicines in palliative care established by the World Health Organization in collaboration with the International Association for Hospice and Palliative Care (IAHPC) [33]. Consensus criteria for drugs of questionable benefit are for a large part centered around treatments used for the control of non-life-threatening comorbidities or for the secondary prevention of cardiovascular diseases, e.g., platelet aggregation inhibitors and oral antidiabetics. This category also contains drugs commonly prescribed to counteract the side effects of other treatment—a phenomenon known as the prescription cascade. Finally, drug classes categorized as often inadequate include a majority of drug treatments used for the long-term prevention of chronic diseases (e.g., vitamin D, statins).
Our approach does not assume that certain drugs are inherently futile or unnecessary at the end of life. Participating experts were asked to provide their probabilistic opinion based on their clinical experience and scientific knowledge rather than an all-embracing judgment with no room for uncertainty or case-by-case variability. For example, panelists reached consensus to consider that continuing antidementia drugs is often inadequate near the end of life, even though it could be justified in specific situations. Conversely, even if one can think of individual patients for whom opioid analgesics would not provide any substantial benefit at the end of life, in a majority of cases it is adequate. Consensus-based criteria are useful to provide guidance and to encourage benchmarking, but decisions regarding the continuation or discontinuation of drug treatments should be tailored at the bedside to address the specific needs and preferences of each individual patient. Recognizing the need for a personalized assessment of drug therapy is essential to avoid the pitfalls of one-size-fits-all clinical standards. Thus, panelists were given the opportunity to express a consensus about the questionable nature of the decision to continue or initiate drug treatments for older adults with very limited life expectancy. We have identified a number of drug classes that may very well be adequate at the end of life, but that should be systematically questioned beforehand and not result from routine-based prescribing practices. This approach is well in line with the Choosing Wisely campaign, in which medical societies have identified tests, procedures, and treatments that are often used inappropriately and that both physicians and patients should question [34, 35].
In the present study, drugs were considered for use among older adults with a maximum of 3 months of life expectancy. In contrast, the STOPPFrail criteria [22] were developed to identify inappropriate drugs among older adults with poor 1-year prognosis, thus broadening the perspective to a substantially longer period of time before death. Physicians and patients typically overestimate the remaining life expectancy, and the accuracy of survival predictions tends to decrease as the timeframe increases [26, 36, 37]. Therefore, determining whether the time-to-benefit of medications is shorter than life expectancy is more difficult for patients who might live for another 12–18 months than for persons whose life expectancy is estimated to be 1–3 months. Our focus on the very end of life may reduce the prognostic uncertainty, and thus enhance the applicability of the proposed lists of drugs in routine clinical practice.
The continuation and the initiation of drug therapy near the end of life pose different challenges in the daily clinical practice. From a pharmacological perspective, the discontinuation of specific drug classes (e.g., antidepressants) is known to trigger withdrawal symptoms and adverse effects that may cause discomfort and affect quality of life at the end of life. Cessation of these drugs requires time-consuming tapering of dosage and a careful monitoring of symptoms [14, 38, 39]. This process implies the availability of a physician at the bedside, which is not always feasible in the everyday care setting. Moreover, stopping drug treatments is often perceived by prescribers as an active decision that can lead to serious adverse consequences, which creates a strong incentive against deprescribing out of fear that it may cause harm. In comparison, the decision not to initiate a new drug treatment is widely considered as an omission rather than as an act. As a result, physicians have been found to perceive the limitation of treatments as less likely to result in negative outcomes than withdrawal [40]. Acknowledging that the degree of appropriateness of a prescription depends on whether therapy is being started or continued can increase the acceptability of our list of inadequate drugs by clinicians. It can also serve as a reminder that good prescribing is not only about knowing when to start and when to stop treating patients, but also about knowing when not to start in the first place.
Consensus remained unachieved for some very commonly prescribed drug classes. Neither the continuation nor the initiation of proton-pump inhibitors (PPI) gathered a consensual opinion among panelists. This lack of agreement mirrors the existence of conflicting positions regarding the use of these drugs near the end of life. While Holmes et al. considered PPIs to be “sometimes appropriate” for older adults with advanced dementia and limited life expectancy [18], De Schreye et al. came to the opposite conclusion and considered all gastric protectors to be inappropriate during the last 6 months of life [41]. Participating experts also did not reach consensus regarding the continuation and the initiation of selective serotonin-reuptake inhibitors (SSRI). This was unexpected, since citalopram and sertraline are recommended as first-line treatment options for depression in palliative care patients and have fewer side effects than other antidepressants, lower risks of drug-drug interactions, and a shorter time-to-benefit [42, 43]. Similarly, consensus remained unachieved for haloperidol, an antipsychotic often prescribed in palliative care practice for the management of delirium [44, 45]. Although 67% of panelists considered the continuation of haloperidol to be “often adequate,” no majority opinion emerged regarding initiation. This may be explained by the lack of evidence regarding the effectiveness of haloperidol for the management of delirium compared with other alternatives (e.g., quetiapine, olanzapine, risperidone) or even with placebo. Recent randomized controlled trials showed that haloperidol did not reduce delirium and resulted in significantly higher extrapyramidal symptoms [46, 47].
The present study present several limitations. First, although consensus methods are widely used to inform clinical practice in the absence of robust empirical data, expert judgment ranks low in the hierarchy of evidence. However, our study was designed to mitigate potential biases, as recommended by Jünger et al. [48]. The panel was larger than for previously published criteria, and composition was balanced with regard to age, occupations, and countries (thus reducing the homogeneity of clinical practices and prescribing attitudes). Consensus attainment was defined a priori based on a 75% agreement cutoff, providing a rather conservative set of criteria for each category. We also made sure that the material sent to participating experts would not directly or indirectly influence their opinion. The list of participants was kept undisclosed during the Delphi survey to prevent cross-contamination among panelists. Second, although it can be argued that implicit criteria (e.g., Medication Appropriateness Index [49]) are clinically more relevant, they cannot be operationalized in large drug prescription databases. Explicit criteria inevitably reduce the complexity of personal, clinical, and ethical considerations that surround the decision to prescribe a specific treatment. However, it is unrealistic to expect data with individualized assessments in large (sometimes country-wide) study cohorts of older adults at the end of life. Third, we asked panelists to grade the appropriateness of drug treatments regardless of their clinical indications although many drug classes may be used for specific health problems near the end of life. This probably explains why some drug classes did not reach a sufficiently high level of agreement. Fourth, our criteria are based on the expert judgment of European clinicians, and may therefore reflect cultural preferences or prescribing attitudes that are specific to European countries. Further studies should therefore investigate whether they also generate consensus in other geographical areas. Also, some adjustments may be necessary to apply these criteria to non-European care settings since the availability of specific drugs varies across national markets. Finally, it should be remembered that our criteria have not been developed to replace the clinical judgment of prescribers. They should instead to be used to encourage patient–physician discussions about the benefits and risks of drug treatments near the end of life.
Conclusion
Considering the lack of robust evidence from randomized clinical trials and well-designed observational studies, our criteria can provide guidance to rationalize drug prescribing for older adults near the end of life. These criteria also offer a standardized framework for future studies investigating the prevalence and the adverse outcomes associated with the use of questionable or inadequate drugs at the end of life.
References
Todd A, Husband A, Andrew I, Pearson SA, Lindsey L, Holmes H (2017) Inappropriate prescribing of preventative medication in patients with life-limiting illness: a systematic review. BMJ Support Palliat Care 7(2):113–121
Molist Brunet N, Espaulella Panicot J, Sevilla-Sánchez D, Amblàs Novellas J, Codina Jané C, Altimiras Roset J, Gómez-Batiste X (2015) A patient-centered prescription model assessing the appropriateness of chronic drug therapy in older patients at the end of life. Eur Geriatr Med 6(6):565–569
Maddison AR, Fisher J, Johnston G (2011) Preventive medication use among persons with limited life expectancy. Prog Palliat Care 19(1):15–21
Morin L, Vetrano DL, Rizzuto D, Calderón-Larrañaga A, Fastbom J, Johnell K (2017) Choosing wisely? Measuring the burden of medications in older adults near the end of life: nationwide, longitudinal cohort study. Am J Med 130(8):927–936.e9
Currow DC, Stevenson JP, Abernethy AP, Plummer J, Shelby-James TM (2007) Prescribing in palliative care as death approaches. J Am Geriatr Soc 55(4):590–595
McNeil MJ, Kamal AH, Kutner JS et al (2016) The burden of polypharmacy in patients near the end of life. J Pain Symptom Manag 51(2):178–183.e2
Ma G, Downar J (2014) Noncomfort medication use in acute care inpatients comanaged by palliative care specialists near the end of life: a cohort study. Am J Hosp Palliat Care 31(8):812–819
Holmes HM, Min LC, Yee M, Varadhan R, Basran J, Dale W, Boyd CM (2013) Rationalizing prescribing for older patients with multimorbidity: considering time to benefit. Drugs Aging 30(9):655–666
Tjia J, Lapane K (2017) Guideline-based prescribing in frail elderly patients. JAMA Intern Med 177(2):262–263
Spinewine A, Schmader KE, Barber N, Hughes C, Lapane KL, Swine C, Hanlon JT (2007) Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet 370(9582):173–184
(2015) American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 63(11):2227–2246
O’Mahony D, O’Sullivan D, Byrne S et al (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218
Holmes HM, Hayley DC, Alexander GC, Sachs GA (2006) Reconsidering medication appropriateness for patients late in life. Arch Intern Med 166(6):605–609
Scott IA, Hilmer SN, Reeve E et al (2015) Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med 175(5):827–834
Garfinkel D, Mangin D (2010) Feasibility study of a systematic approach for discontinuation of multiple medications in older adults: addressing polypharmacy. Arch Intern Med 170(18):1648–1654
Kutner JS, Blatchford PJ, Taylor DHJ et al (2015) Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med 175(5):691–700
Gnjidic D, Le Couteur DG, Kouladjian L et al (2012) Deprescribing trials: methods to reduce polypharmacy and the impact on prescribing and clinical outcomes. Clin Geriatr Med 28(2):237–253
Holmes HM, Sachs GA, Shega JW et al (2008) Integrating palliative medicine into the care of persons with advanced dementia: identifying appropriate medication use. J Am Geriatr Soc 56:1306–1311
Raijmakers NJH, van Zuylen L, Furst CJ, Beccaro M, Maiorana L, Pilastri P, Rossi C, Flego G, van der Heide A, Costantini M (2013) Variation in medication use in cancer patients at the end of life: a cross-sectional analysis. Support Care Cancer 21(4):1003–1011
Lindsay J, Dooley M, Martin J, Fay M, Kearney A, Khatun M, Barras M (2015) The development and evaluation of an oncological palliative care deprescribing guideline: the ‘OncPal deprescribing guideline’. Support Care Cancer 23(1):71–78
Fede A, Miranda M, Antonangelo D, Trevizan L, Schaffhausser H, Hamermesz B, Zimmermann C, del Giglio A, Riechelmann RP (2011) Use of unnecessary medications by patients with advanced cancer: cross-sectional survey. Support Care Cancer 19:1313–1318
Lavan AH, Gallagher P, Parsons C, O’Mahony D (2017) STOPPFrail (screening tool of older persons prescriptions in frail adults with limited life expectancy): consensus validation. Age Ageing 46(4):600–607
Nyborg G, Jør S, Klovning A et al (2015) The Norwegian General Practice-Nursing Home criteria (NORGEP-NH) for potentially inappropriate medication use: a web-based Delphi study. Scand J Prim Health Care 33(2):134–141
Amano K, Maeda I, Shimoyama S, Shinjo T, Shirayama H, Yamada T, Ono S, Yamamoto R, Yamamoto N, Shishido H, Shimizu M, Kawahara M, Aoki S, Demizu A, Goshima M, Goto K, Gyoda Y, Hashimoto K, Otomo S, Sekimoto M, Shibata T, Sugimoto Y, Morita T (2015) The accuracy of physicians’ clinical predictions of survival in patients with advanced cancer. J Pain Symptom Manag 50(2):139–46.e1
White N, Kupeli N, Vickerstaff V, Stone P (2017) How accurate is the ‘Surprise Question’ at identifying patients at the end of life? A systematic review and meta-analysis. BMC Med 15(1):139
White N, Reid F, Harris A, Harries P, Stone P (2016) A systematic review of predictions of survival in palliative care: how accurate are clinicians and who are the experts? PLoS One 11(8):e0161407
Dalkey NC (1969) The Delphi Method: an experimental study of group opinion. RAND Corporation, Santa Monica. https://doi.org/10.1016/S0016-3287(69)80025-X
Kaufmann CP, Tremp R, Hersberger KE, Lampert ML (2013) Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol 70(1):1–11
Marriott J, Stehlik P (2012) A critical analysis of the methods used to develop explicit clinical criteria for use in older people. Age Ageing 41(4):441–450
Renom-Guiteras A, Meyer G, Thürmann PA (2015) The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol 71(7):861–875
Fried TR, Niehoff K, Tjia J, Redeker N, Goldstein MK (2016) A Delphi process to address medication appropriateness for older persons with multiple chronic conditions. BMC Geriatr 16(1):67
Rodríguez-Pérez A, Alfaro-Lara ER, Albiñana-Perez S, Nieto-Martín MD, Díez-Manglano J, Pérez-Guerrero C, Santos-Ramos B (2017) Novel tool for deprescribing in chronic patients with multimorbidity: list of evidence-based deprescribing for chronic patients criteria. Geriatr Gerontol Int 17(11):2200–2207
De Lima L, Radbruch L, Bruera E (2015) Essential medicines for palliative care. In: Cherny N, Fallon M, Kaasa S et al (eds) Oxford textbook of palliative medicine (5 ed.). Oxford University Press
Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA, Choosing Wisely International Working Group (2015) ‘Choosing Wisely’: a growing international campaign. BMJ Qual Saf 24(2):167–174
AGS Choosing Wisely Workgroup (2013) American Geriatrics Society identifies five things that healthcare providers and patients should question. J Am Geriatr Soc 61(4):622–631
Glare P, Virik K, Jones M, Hudson M, Eychmuller S, Simes J, Christakis N (2003) A systematic review of physicians’ survival predictions in terminally ill cancer patients. BMJ 327(7408):195–198
Hui D (2015) Prognostication of survival in patients with advanced cancer: predicting the unpredictable? Cancer Control 22(4):489–497
Parsons C (2016) Withdrawal of antidementia drugs in older people: who, when and how? Drugs Aging 33(8):545–556
van der Cammen TJM, Rajkumar C, Onder G et al (2014) Drug cessation in complex older adults: time for action. Age Ageing 43(1):20–25
Reeve E, Denig P, Hilmer SN, ter Meulen R (2016) The ethics of deprescribing in older adults. J Bioeth Inq 13(4):581–590
De Schreye R, Houttekier D, Deliens L et al (2017) Developing indicators of appropriate and inappropriate end-of-life care in people with Alzheimer’s disease, cancer or chronic obstructive pulmonary disease for population-level administrative databases: a RAND/UCLA appropriateness study. Palliat Med:269216317705099
Rayner L, Price A, Hotopf M, Higginson IJ (2011) The development of evidence-based European guidelines on the management of depression in palliative cancer care. Eur J Cancer 47(5):702–713
Rayner L, Price A, Hotopf M, Higginson IJ (2011) Expert opinion on detecting and treating depression in palliative care: a Delphi study. BMC Palliat Care 10(1):10
Bush SH, Kanji S, Pereira JL, Davis DHJ, Currow DC, Meagher DJ, Rabheru K, Wright DK, Bruera E, Agar M, Hartwick M, Gagnon PR, Gagnon B, Breitbart W, Regnier L, Lawlor PG (2014) Treating an established episode of delirium in palliative care: expert opinion and review of the current evidence base with recommendations for future development. J Pain Symptom Manag 48(2):231–248
Lindqvist O, Lundquist G, Dickman A, Bükki J, Lunder U, Hagelin CL, Rasmussen BH, Sauter S, Tishelman C, Fürst CJ, OPCARE9 (2013) Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med 16(1):38–43
Agar MR, Lawlor PG, Quinn S et al (2016) Efficacy of oral Risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med 27(6):486–498
Schrijver EJM, de Vries OJ, van de Ven PM et al (2017) Haloperidol versus placebo for delirium prevention in acutely hospitalised older at risk patients: a multi-centre double-blind randomised controlled clinical trial. Age Ageing:1–8
Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG (2017) Guidance on conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 31(8):684–706
Samsa GP, Hanlon JT, Schmader KE, Weinberger M, Clipp EC, Uttech KM, Lewis IK, Landsman PB, Cohen HJ (1994) A summated score for the medication appropriateness index: development and assessment of clinimetric properties including content validity. J Clin Epidemiol 47(8):891–896
Acknowledgements
The authors would like to acknowledge the participation of the following experts who participated in the consensus panel and agreed to being acknowledged: Adam Todd, Adelaide Ricciotti, Adriana Turriziani, Alberto Meléndez Gracia, Ana Bandrés Liso, Angelo Carfì, Annabel Price, Bailey Rob, Beatriz Larrayoz Sola, Bernd Oliver Maier, Carlos Coscollar Santaliestra, Céu Rocha, Claudia Bausewein, Claudia Gamondi, Constanze Remi, Domenico Fusco, Domenico La Carpia, Duncan Forsyth, Ferraz Gonçalves, Georg Bosshard, Henri-Pierre Cornu, James Diver, Javier Alonso Renedo, Jørund Straand, Laurent Calvel, Luis Gimeno Feliu, Lydia Holmdahl, Marta Gutiérrez Valencia, Nele Van Den Noortgate, Nicolás Martinez Velilla, Nicole Vogt, Patrick Frioucourt, Per Fürst, Sabine Ruths, Sébastien Moine, Sophie Pautex, Stephen Barclay, Virginie Leroy, as well as the two experts who wished to remain unnamed. The authors are also grateful to Amaia Calderon Larrañaga for her help in identifying potential participants in Spain, and to Jonas Wastesson for his insightful comments during the preparation of the present article.
Funding
This work was supported by a grant from the Swedish Research Council for Health, Working Life and Welfare (grant no. 2014-4699).
Author information
Authors and Affiliations
Contributions
LM, KJ, and JF conceived and designed the study. LM conducted the Delphi survey and analyzed the data. LM, DLV, and MLL interpreted the data. All authors revised the manuscript for important intellectual content and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The regional ethical review Board in Stockholm, Sweden approved the study (decision no. 2015/1341-31/1).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Electronic supplementary material
ESM 1
(DOCX 256 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Morin, L., Laroche, ML., Vetrano, D.L. et al. Adequate, questionable, and inadequate drug prescribing for older adults at the end of life: a European expert consensus. Eur J Clin Pharmacol 74, 1333–1342 (2018). https://doi.org/10.1007/s00228-018-2507-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-018-2507-4