Abstract
In patients with neurofibromatosis type 1 (NF1), decreased bone mineral density (BMD) and low levels of 25-hydroxy vitamin D3 (25OHD) have been reported. Recently, the trabecular bone score (TBS) measurement has been proposed as index of bone microarchitecture and fracture risk. In 74 NF1 patients (48 females, 26 males, age 41 ± 12), we measured TBS and investigated clinical stage, lifestyle, vitamin D, serum bone turnover markers, vertebral and femoral BMD. A homogenous cohort of 61 healthy subjects was used as control group. TBS was lower in NF1 patients (1.266 ± 0.113 vs. 1.346 ± 0.105) without differences between sexes. No correlations with 25OHD, low exercise, low calcium intake, reduced sun exposure, and number of skin neurofibromas were observed. As expected, hypovitaminosis D was common (98.6%), as well as BMD reduction in hip and spine sites: In NF1 patients, bone texture evaluated by TBS was low in both sexes without any correlation with clinical or metabolic parameters, suggesting a direct role of the fibromin mutation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 1 neurofibromatosis (NF1) is an autosomal dominant disorder, involving approximately until one subject every 2000 [1]. The NF1 gene is an oncosuppressor with 60 exons, spanning 350 kb on 17q11.2 region. It encodes for neurofibromin, an ubiquitously expressed protein involved in pathways affecting cell growth and development of skeletal, cardiovascular, and nervous system [2]. Neurofibromin is a member of the GTPase-activating protein gene family and can modulate adenylyl cyclase activity and protein kinase A (PKA), regulators of osteoblasts, and osteoclasts cell function. Decreased expression of neurofibromin is correlated with dose-dependent elevation of intracellular RAS-activity and increasing expression of intracellular signaling pathways, such as mitogen-activated protein kinase (MAPK), phosphatidil inositol-3-phosphate kinase (PI-3K), and decreasing expression of c-fos, a crucial regulator in osteoblast differentiation [3].
Following the recommendations of the National Institute of Health [4, 5] the diagnosis of NF1 can be made when two or more of the following criteria are found: cutaneous neurofibromas, “café-au-lait” spots, iris hamartomas (Lisch’s nodules), axillary or groin freckles, optical gliomas, and bone deformities. The molecular diagnosis of NF1 can identify up to 95% of gene mutations in patients with typical neurofibromatosis [6].
As bone features are concerned, NF1 patients are shorter than expected, with maintained body proportions, thus suggesting a generalized skeleton bone growth decrease [7]. Other studies showed local and general dysregulation in bone resorption, remodeling [8] and increased formation of osteoclasts [9]. An increased bone fractures rate was also observed in affected adults [10] as well as in NF1 postmenopausal women [11]. Reduced bone mineral density (BMD) and osteoporosis were also found in young patients together with an increased fracture risk [12]. Moreover, previous studies reported low levels of serum 25-hydroxy vitamin D3 (25OHD), reduced BMD and trabecular bone density in both adults and children NF1 patients in comparison with healthy subjects [10, 12,13,14,15].
Recently, the trabecular bone score (TBS) has been found to be more accurate than spinal BMD alone as an index of trabecular bone strength able to detect the presence of damage accumulation [16]. TBS is a gray-level texture measurement based on the use of experimental variograms of two-dimensional (2D) projection images acquired during a dual-energy X-ray absorptiometry (DXA) of the lumbar spine (LS). Unlike histomorphometric analysis on bone biopsy, TBS assessment is noninvasive and cost-effective. Moreover, it is calculated by a computer software during the common BMD measurement session and it is highly accurate [17,18,19,20]. It may be used for the routine evaluation of bone microarchitecture, and it is supported by several studies for identifying patients at risk of fracture associated with impaired trabecular microarchitecture [21, 22]. Evidences showed its utility to discriminate fractured patients and to predict fracture risk in primary and secondary osteoporosis [23,24,25,26].
The aim of this study was to evaluate TBS in a cohort of NF1 patients, in order to find possible differences with controls and correlations with bone metabolism, cutaneous NF1 stigmata, sun exposure, and habits of life at the recruitment.
Methods
Seventy-four consecutive patients (48 females, 26 males, age 41.8 ± 11.8) were enrolled in the study in 12 months. A multidisciplinary team, including endocrinologists, geneticists, and radiologists, has evaluated all of them. The enrollment was carried out according with the following inclusion criteria: (i) age between 18 and 65; (ii) clinically diagnosis of NF1 based on recommendations of National Institute of Health; (iii) informed consent expression. The exclusion criteria were: (i) pregnancy or nursing; (ii) disorders affecting bone metabolism, i.e., primary hyperparathyroidism, hyperthyroidism, renal or hepatic chronic disease, malabsorption, hypercortisolism, hypogonadism, premature menopause; (iii) previous or ongoing treatments with glucocorticoids, chemotherapies, bisphosphonates, or other antiosteoporotic drugs; (iv) previous spine or hip fractures; (v) surgical correction of scoliosis.
Sixty-one voluntary healthy subjects (16 males, 45 females, age 40.5 ± 12.8, 32.8% menopause, Table 2) were collected as control group for bone mineralometry and TBS. Age, sex, and menopause rate did not significantly differ between controls and patients. None of the controls had disorders or treatments affecting bone metabolism or mineralometry.
The primary outcomes of the study were: to evaluate TBS difference between NF1 patients and controls in both sexes; to study TBS correlations with 25OH vitamin D, bone metabolism parameters, cutaneous NF1 stigmata, sun exposure, and habits of life at the recruitment.
The study was approved by the local ethics committee.
Clinical Stage of Neurofibromatosis
The severity grade of the disorder was defined according with Riccardi [27]. Briefly, in grade 1 the presence of NF1 features is minimal, without compromise of health; grade 2 stands for an overt disease, but with no health compromise; in grade 3 patients health and well-being are compromised, but clinical problems can be treatable and do not shorten life expectancy; grade 4 includes severe and difficult to treat conditions (mental retardation, tumors, etc.), associated with shortened lifespan [27].
Moreover, the cutaneous involvement of NF1 was evaluated subdividing the cohort of NF1 patients in four subgroups based on the number of skin neurofibromas (minimal: less than 10; mild: 10–99; moderate: 100–999; and severe: more than 1000; this classification was modified from Lammert et al. [13] introducing the “less than 10” category) assessed by clinicians. Clinical data of this cohort are reported in Table 1.
Lifestyle
Employment, exercise, sun exposure, and calcium intake were recorded by questionnaire administration during the enrollment visit.
Briefly, sun exposure was considered low with at least two of the following criteria: no arm and skin exposure during summer months; no sunbathing or holiday in sunny places; no working outdoors. Physical activity (e.g., jogging, swimming, cycling, dancing) for less than 2 h a week has been considered low exercise.
Diet calcium intake was defined low with at least two of the following criteria: milk assumption less than 100 mL a day; less than three yogurts in a week; eating cheese less than two times in a week.
Bone Metabolism and Radiology
Standard assays were used for blood and urine tests. Total calcium was corrected for serum albumin according to the formula: total calcium + (4.4 − albumin [g/dl]) × 0.8 (normal range 8.4–10.4 mg/dl, 2.1–2.5 mmol/l). Urinary calcium and creatinine were measured in 24-h urine collections.
Calcium, albumin, alkaline phosphatase, and creatinine in serum and urinary calcium and creatinine were measured by standard colorimetric techniques. Serum intact PTH was measured by a chemiluminescent method (Nichols Institute Diagnostic, San Juan Capistrano, CA, USA) with intra- and interassay coefficient of variation (CV) of 5.1 and 8.2%, respectively. Serum 25OH-vitamin D (25OHD) levels were measured by RIA (DiaSorin, Saluggia, Italy) with an intra- and interassay CV of 5.6 and 15%, respectively. The serum osteocalcin (OC) was measured (normal value 5–25 ng/ml) by the Invitrogen human Osteocalcin Enzyme Amplified Sensitivity Immunoassay (EASIA) (Life Technologies, Carlsbad, CA, USA) following manufacturer’s instruction. Serum bone turnover markers including the bone resorption marker collagen type 1 C-terminal telopeptide (CTX) (normal value 80–320 pg/ml for men aged 20–50 years, up to 704 pg/ml for men 50–70 years, and 70–573 pg/ml for premenopausal women over 20 years) were determined by the Serum CrossLaps Enzyme-linked Immunosorbent Assay (ELISA) (ImmunodiagnosticSystem Ltd, Boldon, UK) according to manufacturer’s assay procedure.
NF1 patients were classified according to the Endocrine Society’s latest guidelines for vitamin D levels [28]: in particular, deficiency when 25OHD was less than or equal to 20 ng/ml; insufficiency when between 21 and 29 mg/ml, and normal if more than 30 ng/ml.
In all patients, DXA scans were performed at lumbar spine (L1–L4 vertebrae) and non-dominant femoral neck (FN) for BMD measurement, as well as trabecular bone score (TBS) assessment by spine DXA (Hologic discovery, Software version 13.3.3, Bedford MA, USA). TBS measurement was reliable when the BMI of the subjects lied in 18–35 Kg/m2 range, outside of which it has to be corrected. Osteopenia was defined as a BMD T-score between − 1.0 (included) and − 2.5 (excluded), while osteoporosis was assessed when T-score was − 2.5 or less.
Statistical Analysis
The distribution of continuous variables was assessed by inspection of frequency histograms and by Kolmogorov–Smirnov test. Normal variables were reported as mean ± standard deviation (SD), and comparisons were carried out by Student t test. Non-Gaussian variables were reported as median (interquartile range, IQR) and compared by Wilcoxon–Mann–Whitney test.
Dichotomous and nominal variables were compared by Fisher exact test. Linear regression analysis was performed by SPSS software (version 21 for Windows, IBM Inc, Armonk NY USA).
Statistical significance threshold (α) was set to 0.05. When multiple comparisons were carried out, α was reduced according to Bonferroni correction. Statistical power was determined using free calculator available at http://powerandsamplesize.com site and reported as type 2 error probability or β value (1 − power) when α ≥ 0.05.
Results
Trabecular Bone Score
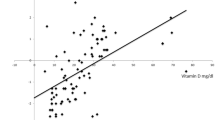
Patients BMI was within 18–35 Kg/m2 range (24.2 ± 3.5, min. 18.0, max. 32.9), and no TBS correction was needed. TBS was 1.266 ± 0.113 in overall patients without sex difference (F: 1.253 ± 0.107 vs. M: 1.273 ± 0.117, P = 0.456, β = 0.20), although the sample size was not adequate to exclude an actual gender variance. TBS in NF1 was significantly lower than in unaffected subjects: 1.346 ± 0.105 (P < 0.001, Fig. 1). Such difference was observed also considering sex-based subgroups. In NF1 males, TBS was 1.253 ± 0.107 versus 1.366 ± 0.092 in controls (P = 0.001) whereas in females was 1.273 ± 0.117 versus 1.339 ± 0.110 (P = 0.001, Fig. 1).
No associations among TBS and 25OHD, age, low exercise, reduced sun exposure, Riccardi scale, and number of skin neurofibromas were observed by linear regression analysis. We also compared TBS in patients with scoliosis (1.272 ± 0.122) or not (1.258 ± 0.079) with no significant difference (P = 0.601, β = 0.60).
Bone Mineralization
In the sample study, bone mineralization was decreased in NF1 patients than in controls (Table 2). In particular, spine raw BMD was significantly reduced in NF1 both whole cohort (0.928 ± 0.141 vs. 1.030 ± 0.109 g/cm2, P < 0.001) and in females (0.918 ± 0.139 vs. 1.030 ± 0.109 g/cm2, P < 0.001, Table 2). In male NF1 BMD was reduced but without significance: 0.948 ± 0.146 versus 1.030 ± 0.113, P = 0.046, β = 0.60. (α was reduced to 0.004 after Bonferroni correction.)
Spine osteopenia was found in 27.9% of controls and in 41.4% of NF1 patients (P = 0.040, β = 0.60) ,and such difference is above the α corrected by Bonferroni method also sex subgroups: female 22.2% versus 37.5%, P = 0.037, β = 0.70; male 43.8% versus 42.3%, P = 0.480, β = 0.90 (Table 2). As regards femoral osteopenia, the differences were 21.3% versus 43.7% (P < 0.001) between controls and NF1 and held for both sexes (females: 24.4% vs. 47.9%, P = 0.001; males: 12.5% vs. 34.6%, P = 0.001, Table 2).
Spine osteoporosis was observed only in NF1 patients (~ 15% vs. 0%, Table 2), and it was not statistically significant on the overall population (P = 0.006, β = 0.10), between females (16.7%, P = 0.006, β = 0.30), and in males (15.4%, P = 0.280, β = 0.60). Femoral osteoporosis prevalence was low and similar in both NF1 and controls (~ 1%), and no statistical analysis was carried out.
Bone Metabolism
Vitamin D levels (25-hydroxy vitamin D, 25OHD) were less than 30 ng/ml in almost all patients (73 out of 74 subjects), while 28 patients (37.8%) had 25OHD less than 10 ng/ml.
Fourteen patients (18.9%) had secondary hyperparathyroidism. In these patients, 25OHD levels were similar to those measured in patients with normal parathyroid hormone (11.1 ± 6.4 vs. 12.7 ± 6.1 ng/ml, P = 0.410), as well as calcium intake and sun exposition rates. 25OHD levels did not significantly differ between sexes: 13.0 ± 6.6 in females versus 11.2 ± 5.1 in males, P = 0.244. A mild, but nonsignificant, correlation among age and 25OHD was detected (ρ = − 0.208, P = 0.100).
No associations between 25OHD and calcium metabolism markers (PTH, alkaline phosphatase, daily urinary calcium) were observed, except for serum phosphate, which showed a positive correlation with vitamin D (r = 0.329, P = 0.004). As regards clinical stigmata, 25OHD correlated with the number of cutaneous neurofibromas (ρ = − 0.242, P = 0.037) but not with Riccardi scale (ρ = − 0.209, P = 0.074).
In a subgroup of 37 patients (22 females, age 42 ± 12), osteocalcin (OC) and collagen type 1 C-terminal telopeptide (CTX) were measured as markers of bone formation and resorption, respectively. Serum CTX was 505.7 ± 202.8 and was found higher than the normal age- and sex-specific range in 11 patients (29.7%), 10 of them being males less than 50 years old (CTX 517.4 ± 163.4, normal range: 80–320 pg/ml).
Osteocalcin levels were 22.6 ± 5.0 ng/ml, with increased levels (> 25 ng/ml) in nine subjects (24.3%, six females and three postmenopausal women, age 41 ± 13).
Discussion
Type 1 neurofibromatosis (NF1) is a genetic disorder due to neurofibromin mutations [6]. Typical NF1 patients have neurofibromas and brown macules on skin, and iris hamartomas [4]. Both bone abnormalities and reduced mineralization [7,8,9,10,11,12] as well as hypovitaminosis D [13] are also common in these patients. Although several studies supported the accuracy of TBS analysis in the assessment of trabecular bone microarchitecture and fracture risk in different disorders, no data on TBS in NF1 patients are available yet.
In this cohort of 74 Italian patients affected with NF1, we observed a marked and significant reduction in TBS in both sexes (Fig. 1). This finding did not correlate with sex, age, 25OHD, sun exposure, lower diet calcium, and lower exercise, and it should be considered as a proper effect of the genetic disorder. Furthermore, this observation was in agreement with the reported evidences of trabecular bone reduction detected by histological methods [12].
Reduced bone mineral content in NF1 patients was already known [7, 10,11,12], and it is due to negative effects of neurofibromin mutations on bone growth and structure [8, 9]. In this cohort, we observed lesser T and Z scores in both hip and spine sites and a significant increase in osteopenia and osteoporosis rates (Table 2). In particular, spine osteoporosis was about 15% in NF1 versus 0% in controls (Table 2), despite the relatively young age of the patients (41 ± 12).
Another common finding in NF1 is hypovitaminosis D that in this series was present in almost all the subjects (Table 1), without gender and age differences. The mechanism underlying the reduced 25OHD in NF1 is unknown. In our population, we found an association between 25OHD and the number of skin neurofibromas (ρ = − 0.242, P = 0.037), confirming what Lammert et al. previously reported [13]. One possible interpretation of this finding is that patients with major skin involvement might avoid exposure because of aesthetic embarrassment or discomfort, although no association with low sun exposure was found. In future, in vitro studies on skin samples might assess whether vitamin D production and metabolism may be deranged in NF1 patients.
As markers of bone formation and resorption were concerned, they did not seem to be related to cutaneous involvement or habits of the patients. The observation of increased levels of osteocalcin (OC), a marker of osteoblastic activity and bone neoformation, in NF1 patients is consistent with a previous report [14]. This finding might be considered as a compensatory mechanism against the increased resorption, which is in turn pointed out by high levels of CTX observed in NF1 patients. However, in this study OC and CTX abnormalities were referred to the normal range of the assay: no biochemical evaluation against the control group was carried out.
Another common finding in NF1 was scoliosis, which we found in 32% of patients. In the present study, no correlation between TBS and scoliosis was observed, but the statistical power of such comparison was poor (0.40%).
In conclusion, to date this is the first study reporting low TBS in NF1 patients, this observation being in agreement with the reported evidences of trabecular bone reduction detected by histological methods [12]. It would be of great clinical interest to verify in further and targeted studies the accuracy of TBS in assessing the risk of other bone abnormalities that are frequent in NF1 patients, specially scoliosis and bone dysplasia, as well as fracture risk in elder patients. This goal will be easily achieved in the future by introducing DXA bone quality assessment calculating TBS as routine evaluation in NF1 patients.
References
Kallionpää RA, Uusitalo E, Leppävirta J et al (2017) Prevalence of neurofibromatosis type 1 in the Finnish population. Genet Med. https://doi.org/10.1038/gim.2017.215
Larizza L, Gervasini C, Natacci F, Riva P (2009) Developmental abnormalities and cancer predisposition in neurofibromatosis type 1. Curr Mol Med 9:634–653
Ylä-Outinen H, Aaltonen V, Björkstrand AS et al (1998) Upregulation of tumor suppressor protein neurofibromin in normal human wound healing and in vitro evidence for platelet derived growth factor (PDGF) and transforming growth factor-beta1 (TGF-beta1) elicited increase in neurofibromin mRNA steady-state levels in dermal fibroblasts. J Invest Dermatol 110:232–237. https://doi.org/10.1046/j.1523-1747.1998.00108.x
(1988) National Institutes of Health Consensus Development Conference Statement: neurofibromatosis. Bethesda, Md., USA, July 13–15, 1987. Neurofibromatosis 1:172–178
Pasmant E, Parfait B, Luscan A et al (2015) Neurofibromatosis type 1 molecular diagnosis: what can NGS do for you when you have a large gene with loss of function mutations? Eur J Hum Genet EJHG 23:596–601. https://doi.org/10.1038/ejhg.2014.145
Pasmant E, Sabbagh A, Spurlock G et al (2010) NF1 microdeletions in neurofibromatosis type 1: from genotype to phenotype. Hum Mutat 31:E1506–E1518. https://doi.org/10.1002/humu.21271
Lammert M, Kappler M, Mautner V-F et al (2005) Decreased bone mineral density in patients with neurofibromatosis 1. Osteoporos Int 16:1161–1166. https://doi.org/10.1007/s00198-005-1940-2
Seitz S, Schnabel C, Busse B et al (2010) High bone turnover and accumulation of osteoid in patients with neurofibromatosis 1. Osteoporos Int 21:119–127. https://doi.org/10.1007/s00198-009-0933-y
Stevenson DA, Yan J, He Y et al (2011) Multiple increased osteoclast functions in individuals with neurofibromatosis type 1. Am J Med Genet A 155:1050–1059. https://doi.org/10.1002/ajmg.a.33965
Tucker T, Schnabel C, Hartmann M et al (2009) Bone health and fracture rate in individuals with neurofibromatosis 1 (NF1). J Med Genet 46:259–265. https://doi.org/10.1136/jmg.2008.061895
Kuorilehto T, Pöyhönen M, Bloigu R et al (2005) Decreased bone mineral density and content in neurofibromatosis type 1: lowest local values are located in the load-carrying parts of the body. Osteoporos Int 16:928–936. https://doi.org/10.1007/s00198-004-1801-4
Brunetti-Pierri N, Doty SB, Hicks J et al (2008) Generalized metabolic bone disease in neurofibromatosis type I. Mol Genet Metab 94:105–111. https://doi.org/10.1016/j.ymgme.2007.12.004
Lammert M, Friedman JM, Roth HJ et al (2006) Vitamin D deficiency associated with number of neurofibromas in neurofibromatosis 1. J Med Genet 43:810–813. https://doi.org/10.1136/jmg.2006.041095
Petramala L, Giustini S, Zinnamosca L et al (2012) Bone mineral metabolism in patients with neurofibromatosis type 1 (von Recklingausen disease). Arch Dermatol Res 304:325–331. https://doi.org/10.1007/s00403-011-1191-3
Armstrong L, Jett K, Birch P et al (2013) The generalized bone phenotype in children with neurofibromatosis 1: a sibling matched case–control study. Am J Med Genet A 161:1654–1661. https://doi.org/10.1002/ajmg.a.36001
Mirzaali MJ, Libonati F, Ferrario D et al (2018) Determinants of bone damage: an ex-vivo study on porcine vertebrae. PLoS ONE 13:e0202210. https://doi.org/10.1371/journal.pone.0202210
Pothuaud L, Carceller P, Hans D (2008) Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone 42:775–787. https://doi.org/10.1016/j.bone.2007.11.018
Pothuaud L, Barthe N, Krieg M-A et al (2009) Evaluation of the potential use of trabecular bone score to complement bone mineral density in the diagnosis of osteoporosis: a preliminary spine BMD-matched, case-control study. J Clin Densitom 12:170–176. https://doi.org/10.1016/j.jocd.2008.11.006
Rabier B, Héraud A, Grand-Lenoir C et al (2010) A multicentre, retrospective case-control study assessing the role of trabecular bone score (TBS) in menopausal Caucasian women with low areal bone mineral density (BMDa): analysing the odds of vertebral fracture. Bone 46:176–181. https://doi.org/10.1016/j.bone.2009.06.032
Hans D, Goertzen AL, Krieg M-A, Leslie WD (2011) Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res 26:2762–2769. https://doi.org/10.1002/jbmr.499
Del Rio LM, Winzenrieth R, Cormier C, Di Gregorio S (2013) Is bone microarchitecture status of the lumbar spine assessed by TBS related to femoral neck fracture? A Spanish case-control study. Osteoporos Int 24:991–998. https://doi.org/10.1007/s00198-012-2008-8
Bréban S, Briot K, Kolta S et al (2012) Identification of rheumatoid arthritis patients with vertebral fractures using bone mineral density and trabecular bone score. J Clin Densitom 15:260–266. https://doi.org/10.1016/j.jocd.2012.01.007
Ulivieri FM, Silva BC, Sardanelli F et al (2014) Utility of the trabecular bone score (TBS) in secondary osteoporosis. Endocrine 47:435–448. https://doi.org/10.1007/s12020-014-0280-4
Eller-Vainicher C, Filopanti M, Palmieri S et al (2013) Bone quality, as measured by trabecular bone score, in patients with primary hyperparathyroidism. Eur J Endocrinol Eur Fed Endocr Soc 169:155–162. https://doi.org/10.1530/EJE-13-0305
Martineau P, Silva BC, Leslie WD (2017) Utility of trabecular bone score in the evaluation of osteoporosis. Curr Opin Endocrinol Diabet Obes 24:402–410. https://doi.org/10.1097/MED.0000000000000365
Silva BC, Broy SB, Boutroy S et al (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom 18:309–330. https://doi.org/10.1016/j.jocd.2015.06.008
Riccardi VM (1981) Cutaneous manifestation of neurofibromatosis: cellular interaction, pigmentation, and mast cells. Birth Defects Orig Artic Ser 17:129–145
Cianferotti L, Brandi ML (2012) Guidance for the diagnosis, prevention and therapy of osteoporosis in Italy. Clin Cases Miner Bone Metab 9:170–178
Acknowledgements
Authors would like to show their gratitude to Dr Faustina Lalatta, Dr Claudia Cesaretti, Dr Luca Petruccio Piodi, Dr Ciriaco Buonomenna for their contribution to this study and, in particular, to Dr. Silvana Puglisi for data collection.
Author information
Authors and Affiliations
Contributions
MF, UV, and FN designed the study. UV is guarantor. MF, UV, FN, FMU, CG, and GR contributed to patients management and collecting data. MF was responsible for statistical analysis. MF, UV, MA, and AS prepared the first draft of the paper. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Corresponding author
Ethics declarations
Conflict of interest
Marcello Filopanti, Uberta Verga, Fabio Massimo Ulivieri, Claudia Giavoli, Giulia Rodari, Maura Arosio, Federica Natacci, and Anna Spada declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethical Committee of the Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico. No investigations in animals were carried out in this study. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Filopanti, M., Verga, U., Ulivieri, F.M. et al. Trabecular Bone Score (TBS) and Bone Metabolism in Patients Affected with Type 1 Neurofibromatosis (NF1). Calcif Tissue Int 104, 207–213 (2019). https://doi.org/10.1007/s00223-018-0488-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0488-z