Abstract
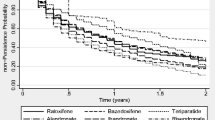
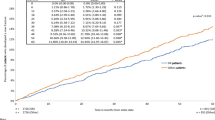
The objective of this study was to describe and analyze the gastrointestinal tolerability and medication switching in patients receiving treatment for primary osteoporosis in Sweden. The study was based on all patients starting therapy with alendronate, risedronate, strontium ranelate, and raloxifene in Sweden between 2005 and 2009. The primary outcome measure was start of treatment with a gastroprotective agent, and the secondary outcome was hospitalization for a gastrointestinal adverse event (GIAE). Switching was analyzed while patients were on treatment. The crude incidence of gastroprotective treatment during the first 6 months after initiation of osteoporosis therapy was 5.14%, 5.93%, 4.25%, and 2.86% for patients prescribed alendronate, risedronate, strontium ranelate, and raloxifene, respectively. Patients prescribed raloxifene had a significantly lower risk of filling a prescription for a gastroprotective agent compared with alendronate. There was no significant difference in the risk of hospitalization for GIAEs. Less than 3% switched therapy while on treatment. Patients prescribed risedronate, strontium ranelate, and raloxifene had a significantly higher risk of switching compared with patients taking alendronate. In conclusion, no significant difference in the incidence of GIAEs was found between patients prescribed alendronate, risedronate, and strontium ranelate. Individuals prescribed raloxifene had a significantly lower risk of GIAEs compared with patients prescribed alendronate. No significant difference was found in the frequency of hospitalization for GIAEs. Switching between osteoporosis medications and drug classes was uncommon. Prescribers should consider the real-world gastrointestinal safety of osteoporosis drugs when choosing between treatment options to potentially improve medication adherence and consequently effectiveness.



Similar content being viewed by others
References
Reginster JY, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:S4–S9
EFFO(NOF) (1997) Who are candidates for prevention and treatment for osteoporosis? Osteoporos Int 7:1–6
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16 Suppl 2: S3–S7
Swedish Medical Products Agency (2007) Behandling av osteoporos. Information från Läkemedelsverket 18:19–38
National Institute for Health and Clinical Excellence (NICE) (2008) Osteoporosis: assessment of fracture risk and the prevention of osteoporotic fractures in individuals at high risk. Available from: http://www.nice.org.uk/nicemedia/live/11621/42362/42362.pdf
Bobba RS, Beattie K, Parkinson B, Kumbhare D, Adachi JD (2006) Tolerability of different dosing regimens of bisphosphonates for the treatment of osteoporosis and malignant bone disease. Drug Saf 29:1133–1152
Strampel W, Emkey R, Civitelli R (2007) Safety considerations with bisphosphonates for the treatment of osteoporosis. Drug Saf 30:755–763
Cadarette SM, Katz JN, Brookhart MA, Sturmer T, Stedman MR, Levin R, Solomon DH (2009) Comparative gastrointestinal safety of weekly oral bisphosphonates. Osteoporos Int 20:1735–1747
Miller R, Bolognese M, Worley K, Solis A, Sheer R (2004) Incidence of gastrointestinal events among bisphosphonate patients in an observational setting. Am J Manag Care 10:207–215
Kane S, Borisov N, Brixner D (2004) Pharmacoeconomic evaluation of gastrointestinal tract events during treatment with risedronate or alendronate: a retrospective cohort study. Am J Manag Care 10:216–226
Ste-Marie LG, Brown JP, Beary JF, Matzkin E, Darbie LM, Burgio DE, Racewicz AJ (2009) Comparison of the effects of once-monthly versus once-daily risedronate in postmenopausal osteoporosis: a phase II, 6-month, multicenter, randomized, double-blind, active-controlled, dose-ranging study. Clin Ther 31:272–285
MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, Mojica W, Timmer M, Alexander A, McNamara M, Desai SB, Zhou A, Chen S, Carter J, Tringale C, Valentine D, Johnsen B, Grossman J (2008) Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 148:197–213
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, Coyle D, Tugwell P (2008) Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev CD001155
Deeks ED, Dhillon S (2010) Strontium ranelate: a review of its use in the treatment of postmenopausal osteoporosis. Drugs 70:733–759
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Gluer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) investigators. JAMA 282:637–645
Lanza FL, Hunt RH, Thomson AB, Provenza JM, Blank MA (2000) Endoscopic comparison of esophageal and gastroduodenal effects of risedronate and alendronate in postmenopausal women. Gastroenterology 119:631–638
Thomson AB, Marshall JK, Hunt RH, Provenza JM, Lanza FL, Royer MG, Li Z, Blank MA (2002) 14 day endoscopy study comparing risedronate and alendronate in postmenopausal women stratified by Helicobacter pylori status. J Rheumatol 29:1965–1974
Ideguchi H, Ohno S, Hattori H, Ishigatsubo Y (2007) Persistence with bisphosphonate therapy including treatment courses with multiple sequential bisphosphonates in the real world. Osteoporos Int 18:1421–1427
Landfeldt E, Strom O, Robbins S, Borgstrom F (2011) Adherence to treatment of primary osteoporosis and its association to fractures—the Swedish Adherence Register Analysis (SARA). Osteoporos Int (in press)
Ettinger B, Chidambaran P, Pressman A (2001) Prevalence and determinants of osteoporosis drug prescription among patients with high exposure to glucocorticoid drugs. Am J Manag Care 7:597–605
National Board of Health and Welfare (2010) http://www.socialstyrelsen.se
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139
Ettinger B, Pressman A, Schein J (1998) Clinic visits and hospital admissions for care of acid-related upper gastrointestinal disorders in women using alendronate for osteoporosis. Am J Manag Care 4:1377–1382
Hosmer DW, Lemeshow S (1999) Applied survival analysis: regression modeling of time to event data. John Wiley & Sons, New York, NY
Rosenbaum P, Rubin D (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Cramer JA, Lynch NO, Gaudin AF, Walker M, Cowell W (2006) The effect of dosing frequency on compliance and persistence with bisphosphonate therapy in postmenopausal women: a comparison of studies in the United States, the United Kingdom, and France. Clin Ther 28:1686–1694
Brankin E, Walker M, Lynch N, Aspray T, Lis Y, Cowell W (2006) The impact of dosing frequency on compliance and persistence with bisphosphonates among postmenopausal women in the UK: evidence from three databases. Curr Med Res Opin 22:1249–1256
Foster SA, Foley KA, Meadows ES, Johnston JA, Wang S, Pohl GM, Long SR (2008) Characteristics of patients initiating raloxifene compared to those initiating bisphosphonates. BMC Womens Health 8:24
Shah AA, Fitzgerald DJ, Murray FE (1999) Non-steroidal anti-inflammatory drugs (NSAIDs) and gastro-intestinal toxicity: current issues. Ir J Med Sci 168:242–245
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was sponsored by Amgen. E. Landfeldt, A. Lang, and O. Ström have previously received funding from pharmaceutical companies involved in marketing products for treatment of osteoporosis. S. Robbins is an employee of Amgen.
Rights and permissions
About this article
Cite this article
Landfeldt, E., Lang, A., Robbins, S. et al. Gastrointestinal Tolerability and Patterns of Switching in Patients Treated for Primary Osteoporosis: The Swedish Adherence Register Analysis (SARA). Calcif Tissue Int 89, 234–245 (2011). https://doi.org/10.1007/s00223-011-9511-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-011-9511-3