Abstract
There is an ongoing controversy respecting calcium supplementation and its role in osteoporosis treatment and prevention. Ca can be present in different forms that are likely to vary in their chemical properties and bioavailability. This is the first study to investigate the bioavailability of calcium pyruvate (CaPyr) and to compare it with calcium citrate malate (CaCitrMalt) and calcium carbonate (CaCarb).We performed a double-blind, four-arm, randomized, placebo-controlled trial (crossover design with 14-day washout) in which 1 g of Ca in each of these forms was administrated orally to 12 healthy postmenopausal women fasted prior to intervention. The greatest increase in serum Ca content was observed within the first 180 min although no statistically significant difference was found in the area under the plasma concentration curve between the studied supplement groups. The urinary Ca content in the 0- to 12-h interval increased after CaCitrMalt and CaPyr administration with the greatest values observed for the former. All the studied formulas decreased the intact parathyroid hormone level in serum although the greatest change was observed for CaPyr and CaCarb. The administration of CaPyr induced gastrointestinal side effects, dyspepsia and diarrhea in 16.6 % of the studied individuals. No serious adverse events were noted. CaPyr demonstrates both a promising source of Ca and a potential for use in osteoporosis prevention. Further investigations should focus on the long-term dietary effects of CaPyr supplementation to assess its safety and potential beneficial effect on human Ca turnover.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcium (Ca) is a highly essential element whose intake in some populations is below the required recommendations. At the same time, being the most abundant mineral in the human body, it is necessary for muscle function, nerve transmission, intracellular signaling and vascular contraction and vasodilation. The majority of Ca (99 %) is present in teeth and bones in a chemical form of hydroxyapatite [Ca10(PO4)6(OH)2] with the rest circulating in extracellular fluids and plasma and deposited in soft tissues and organs. This internal Ca balance is mediated by vitamin D and parathyroid hormone [1, 2]. The most important human pathology resulting from lowered Ca intakes or poor Ca absorption is osteoporosis—a skeletal disorder characterized by decreased bone mass, weakness and fragility [3].
The recommended daily intakes of Ca vary from 400 to 1200 mg per day depending on age and gender; however, these needs are not always met in a traditional diet [4, 5]. Therefore, the use of dietary supplements containing Ca, as a method to prevent osteoporosis and other disorders related to Ca deficiency, is becoming increasingly popular [6]. Over the years, a variety of Ca formulas have become commercially available with most products based on carbonate or citrate form. The bioavailability of Ca from dietary supplements has been widely studied in recent years but remains controversial [7, 8]. Interestingly, the bioavailability of Ca in the organic form of Ca pyruvate has not been studied so far. Pyruvate is known to play a pivotal role in various physiological processes, e.g., as the gateway between the glycolysis pathway and the Krebs cycle [9]. Therefore, as a counterion, it could affect the absorption of Ca through the epithelial cells and subsequently increase its availability.
The present study investigated Ca absorption from different compounds: pyruvate, citrate/malate as well as carbonate, and their effect on the intact parathyroid hormone (iPTH) level in a double-blind, four-arm, randomized, placebo-controlled trial. We also assessed the safety of the tested compounds and the potential side effects they may induce. This study adds to the general understanding of the role of Ca supplementation with various formulas in prevention of Ca deficiency and associated disorders, and demonstrates for the first time that pyruvate is a bioavailable form of Ca with a promising potential to prevent disorders related to Ca deficiency.
Subjects and methods
Subjects
Twelve volunteers were recruited from the general population of healthy postmenopausal women aged 45–60 years old, living in the City of Poznań (Poland, Europe). The exclusion criteria were as follows: overweight (BMI > 30 kg/m2), menstrual hemorrhage in the preceding 6 months before participation in the study changes in hormone replacement therapy (if present) during trial participation (3 months), diabetes, hyperparathyroidism, thyroid or other endocrine disorders, bone disease, nephrolithiasis, renal disease, peptic or duodenal ulcer, bowel disease, intestinal resection or malabsorption, regional enteritis, chronic diarrhea, liver disorder, cigarette smoking and alcoholism. The exclusion criteria further included: uptake of any vitamin or mineral supplement, anticonvulsants, diuretics, steroids (other than hormone replacement therapy as described above), bisphosphonates or other medications that could affect calcium or vitamin D metabolism in the preceding 14 days before study day 1. To exclude participants with major or long-lasting disturbances in bone metabolism, bone densitometry was performed using the DEXA method. All volunteers eligible for the study had a Z-score within the −1.0 to +1.0 range. The study was approved by the Bioethics Committee of Poznan University of Medical Sciences and was in conformance with the Declaration of Helsinki and CONSORT statement. Written informed consent was obtained from all participants before inclusion in the trial.
Tested calcium formulations and placebo
Three Ca formulations were used in this study: 5.80 g of pyruvate monohydrate (C6H6CaO6; CaPyr) containing 17.2 % of Ca [10], 4.23 g of citrate malate hydrate (C16H14Ca4O19; CaCitrMal) containing 23.7 % of Ca, and 2.80 g of carbonate (CaCO3; CaCarb) containing 40 % of Ca. Content of Ca in each formulation corresponded to 1 g of Ca2+. The placebo was composed of maltose. All compounds were placed in the form of powder in blinded sachets of identical appearance. Before administration, the whole content of each sachet was thoroughly suspended in 150 mL of distilled water by stirring for 30 s.
Run-in phases
Two weeks prior to the study, each volunteer was brought to Ca homeostasis through a daily intake of two doses of dietary supplement (Theva Pharmaceuticals, Poland) containing 500 mg Ca (in form of CaCO3) and 200 IU of vitamin D3 lasting for 11 days and followed by 2 days of a balanced diet to aid Ca absorption. This supplementation was undertaken to ensure that decreased Ca status would not alter its absorption rate during the intervention phase.
Intervention
To investigate the bioavailability of Ca in tested formulations, twelve volunteers were included in the placebo-controlled, randomized, four-way, four-period, repeated-measures crossover study. A single oral dose of CaPyr, CaCitrMal, CaCarb or placebo was randomly assigned on study days 1, 14, 28 and 42 after a 12-h fasting period. The blinded random list was based upon 4 × 4 Latin squares (block size 4) and their mirror images (balanced design) and was not known to either investigators or volunteers until the end of the study. After administration, all volunteers were kept fasting and after 4, 6 and 10 h received a Ca-standardized breakfast, dinner and supper, respectively. The 100 mL of non-carbonized water uptake per hour was maintained. Urine samples were collected in fractions 0–12 h and 12–4 h after administration. Venous blood samples were collected directly before administration (0 h) and 1, 2, 3, 5, 6, 12 and 24 h afterward. All volunteers were kept under observation by the investigators throughout the entire study period.
Analyses of Ca content in serum and urine
To estimate the bioavailability of Ca from orally ingested formulations, the content of the element was determined in urine and serum 1, 3, 5, 7, 12 and 24 h following the administration of each supplement. Levels of Ca were analyzed using a photometric assay performed at the Central Laboratory in the Gynecologic and Obstetrical Hospital in Poznań, Poland, using a multi-analyte analyzer Cobas Integra 400 Plus (Roche Diagnostics Ltd., Switzerland). The laboratory is accredited annually by RIQAS (Randox International Quality Assessment Scheme).
Analyses of intact parathyroid hormone content in serum
The content of intact parathyroid hormone (iPTH) in serum was estimated by a radioimmunological assay carried out in a routine diagnostics at an endocrinological laboratory 1, 3, 7 and 24 h following the administration of each supplement.
Calculations and statistical analyses
Obtained data were analyzed using Proc MIXED of the statistical software SAS V9.2. Serum concentrations were transformed from mmol L−1 to mg dL−1 using the factor 4.01 and ln-transformed before calculating the area under the plasma concentration–time curve (AUC) and maximum plasma concentration (C max). The parameters for AUC were confined to the area under the curve from time zero to the last measurement. The content of serum Ca and iPTH was presented as a percentage of the baseline level.
Results
Serum concentrations of Ca
The mean curves of serum Ca concentrations for each treatment phase (CaPyr, CaCitrMalt, CaCarb and placebo) revealed no statistically significant difference. An increase in Ca content was observed within the first 180 min of ingestion with the maximum values found for CaCitrMalt (Fig. 1). No differences in C max and AUC were found between the treated groups and the placebo although again, the maximum values were revealed after the ingestion of CaCitrMalt (Table 1).
Urinary excretion of Ca
Compared to the placebo, the mean urinary concentrations of Ca between 0–12 h were significantly increased in the group treated with CaPyr and CaCitrMalt, but no such difference was noted for CaCarb. For the 12- to 24-h and 0- to 24-h time intervals, Ca concentrations revealed no differences between the placebo and treatment groups. Moreover, the treatment groups also did not vary between each other (Table 2).
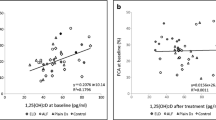
Parathyroid hormone level
All studied Ca supplements induced a decrease in iPTH. The most profound changes were found after administration of CaPyr and CaCarb (Fig. 2).
Side effects and adverse events
Following CaPyr ingestion, two volunteers reported adverse events characterized by gastrointestinal effects: dyspepsia and diarrhea. Additionally, one volunteer reported the same side effects following CaCitrMalt intake. No other adverse events were recorded. No patient was lost or withdrawn from the study.
Discussion
Supplementation of Ca has been commonly recommended for patients suffering from osteoporosis but also for the prevention of this disease in groups of increased risk, e.g., postmenopausal women [7, 11]. Commercial products manufactured to supplement this mineral vary in Ca form. Therefore, a study and comparison of their bioavailability and metabolism is essential. The present study demonstrated that the tested Ca formulas, carbonate, pyruvate and citrate/malate, differ in bioavailability. CaCitrMalt increased Ca levels most significantly but revealed the greatest urinary excretion and the lowest effect on iPTH level. Thus, it can be assumed that CaCarb and CaPyr were the most effective in Ca supplementation. The study was, however, conducted on small number of subjects, and therefore, its results should be treated cautiously.
It should be emphasized that Ca supplementation may not always be beneficial for human health and it remains controversial. As recognized by the general public, Ca supplementation, apart from decreasing the risk of osteoporosis, may also have an impact on cancer prevention and play a role in the decrease in cardiovascular disorders [6, 12]. These assumptions are, however, only partially supported and require further studies [11, 13, 14]. Moreover, some studies support the view that Ca supplementation may even increase the risk of adverse cardiovascular events and have a deteriorating effect on lipid levels [15, 16]. To achieve realistic and comparable conditions in which both passive and active absorption pathways contribute significantly, in the present each supplement was administered in a dose of 1 g of Ca. It should, however, be noted that such daily supplementation at such concentration may finally adversely affect iron absorption [17]. Therefore, it would be desirable for such supplementation to be subjected to ‘pro’s and con’s’ analyses prior to use and an evaluation made as to whether the potentially detrimental effects can be balanced against the likely benefits of calcium on bone [16, 18]. The aforementioned adverse events associated with Ca supplementation were, however, observed epidemiologically or in long-term (>half year) randomized controlled trials. Our study had a short-term design and, as shown, both CaCitrMalt and CaPyr formulas induced dyspepsia and diarrhea. The latter has previously been reported for pyruvate compounds along with gas and bloating [19]. Although the prevalence of these symptoms was low in the studied group, the potential risk of gastrointestinal events following the use of these supplements should be taken into account. To decrease the potential occurrence of side effects, it should be ensured that the manufactured product is of the highest quality and purity [20].
Previous studies have shown that CaCitrMalt is likely to be more bioavailable than CaCarb [8, 21, 22]. These differences arise from the dependency of CaCarb solubility on an acidic environment, while CaCitrMalt has been shown to be partially soluble in water [23]. The present study is the first to compare the absorption of CaCitrMalt and CaCarb with CaPyr which is only slightly soluble in water [24]. As demonstrated in some previous investigations, CaPyr may have beneficial effects on health which include stimulation of weight and fat loss as well as improvement of exercise capacity, primarily in overweight individuals [25]. Hence, pyruvate has recently become a popular weight-loss supplement and a performance-enhancing aid [26]. Nevertheless, these findings remain controversial and depend on the quality and stability issues of different CaPyr hydrates [27]. It has been demonstrated that CaPyr does not alter training adaptations without creatinine supplementation [25]. Moreover, Koh-Banerjee et al. [15] showed that not only does CaPyr supplementation not affect body composition during training but it may even cancel some of the normally positive effects of exercise on blood lipid profiles. Further investigations are necessary to fully elucidate the mechanism behind this observation.
As demonstrated in the present study, ingestion of a relatively high single dose of Ca (1000 mg) in the form of CaPyr, CaCitrMalt or CaCarb induced a slight increase in Ca blood levels within the studied time intervals. The greatest effect, also signified by C max and AUC values, was found for CaCitrMalt. In agreement with Hanzlik et al. [8], the increase in serum Ca content was the most significant only within the first few hours of ingestion. The oral use of CaCitrMalt also resulted in the greatest urinary excretion of Ca, whereas in case of CaPyr and CaCarb, excretion was nearly equal. Interestingly, CaPyr and CaCarb had the most profound effect on decreasing the iPTH levels. Considering its role in Ca regulation and use as biochemical marker of relative bioavailability of Ca from various products [1, 2], the lowered iPTH content following the administration of the studied Ca supplements indicates that all of them, but particularly CaPyr and CaCarb may be useful in inhibiting the release of Ca from bone stores.
The maximum values of serum Ca content followed by significantly increased urine Ca levels following the ingestion of CaCitrMalt suggest that this form of Ca is the most readily absorbed form among those that were studied. CaPyr exhibited no competitive properties in Ca supplementation with CaCitrMalt in this regard. This does not exclude its potential use in Ca supplementation, particularly for subjects with low Ca dietary intakes or suffering from Ca deficiency although further clinical trials would be required to fully understand the potential of this forms in the treatment of Ca-associated alterations.
In summary, the present study demonstrated that supplementation of CaCitrMalt exhibits the greatest absorption but also the most profound Ca loss with urine. In turn, administration of CaPyr and CaCarb leads to the most effective decrease in iPTH in the short term. No serious side effects were noted following a single dosage of each supplement although two individuals developed mild gastrointestinal events after CaPyr use. However, CaPyr demonstrates a promising source of Ca and a potential for use in osteoporosis prevention. Further investigations should focus on the long-term dietary effects of CaPyr supplementation to assess its safety and potential beneficial effect on human Ca turnover.
References
Awenuy EM, Bukoski RD (2006) In: Weaver CM, Haeney RP (eds) Cellular functions and fluxes of calcium. Humana Press Inc, Totwa
Reinwald S, Weaver CM, Kester JJ (2008) The health benefits of calcium citrate malate: a review of the supporting science. Adv Food Nutr Res 54:219–346
Golob AL, Laya MB (2015) Osteoporosis: screening, prevention, and management. Med Clin North Am 99:587–606
Pettifor JM (2008) Vitamin D &/or calcium deficiency rickets in infants & children: a global perspective. Indian J Med Res 127:245–249
Al-Musharaf S, Al-Othman A, Al-Daghri NM, Krishnaswamy S, Yusuf DS, Alkharfy KM, Al-Saleh Y, Al-Attas OS, Alokail MS, Moharram O, Yakout S, Sabico S, Chrousos GP (2012) Vitamin D deficiency and calcium intake in reference to increased body mass index in children and adolescents. Eur J Pediatr 171:1081–1086
Neuhouser ML (2003) Dietary supplement use by American women: challenges in assessing patterns of use, motives and costs. J Nutr 133:1992S–1996S
Dawson-Hughes B, Dallal GE, Krall EA, Sadowski L, Sahyoun N, Tannenbaum S (1990) A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med 323:878–883
Hanzlik RP, Fowler SC, Fisher DH (2005) Relative bioavailability of calcium from calcium formate, calcium citrate, and calcium carbonate. J Pharmacol Exp Ther 313:1217–1222
Hereng TH, Elgstøen KB, Cederkvist FH, Eide L, Jahnsen T, Skålhegg BS, Rosendal KR (2011) Exogenous pyruvate accelerates glycolysis and promotes capacitation in human spermatozoa. Hum Reprod 26:3249–3263
Pischel I, Weiss S, Ortenburger G, Koenig H (1999) Method of producing calcium pyruvates, US5962734
Prentice RL, Pettinger MB, Jackson RD, Wactawski-Wende J, Lacroix AZ, Anderson GL, Chlebowski RT, Manson JE, Van Horn L, Vitolins MZ, Datta M, LeBlanc ES, Cauley JA, Rossouw JE (2013) Health risks and benefits from calcium and vitamin D supplementation: Women’s Health Initiative clinical trial and cohort study. Osteoporos Int 24:567–580
Neuhouser ML, Patterson RE, Levy L (1999) Motivations for using vitamin and mineral supplements. J Am Diet Assoc 99:851–854
Bostick RM, Kushi LH, Wu Y, Meyer KA, Sellers TA, Folsom AR (1999) Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am J Epidemiol 149:151–161
Heine-Bröring RC, Winkels RM, Renkema JM, Kragt L, van Orten-Luiten AC, Tigchelaar EF, Chan DS, Norat T, Kampman E (2015) Dietary supplement use and colorectal cancer risk: a systematic review and meta-analyses of prospective cohort studies. Int J Cancer 136:2388–2401
Koh-Banerjee PK, Ferreira MP, Greenwood M, Bowden RG, Cowan PN, Almada AL, Kreider RB (2005) Effects of calcium pyruvate supplementation during training on body composition, exercise capacity, and metabolic responses to exercise. Nutrition 21:312–319
Bolland MJ, Barber PA, Doughty RN, Mason B, Horne A, Ames R, Gamble GD, Grey A, Reid IR (2008) Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 336:262–266
Cook JD, Dassenko SA, Whittaker P (1991) Calcium supplementation: effect on iron absorption. Am J Clin Nutr 53:106–111
Shin CS, Kim KM (2015) The risks and benefits of calcium supplementation. Endocrinol Metab (Seoul) 30:27–34
Onakpoya I, Hunt K, Wider B, Ernst E (2014) Pyruvate supplementation for weight loss: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Food Sci Nutr 54:17–23
Rzymski P, Niedzielski P, Kaczmarek N, Jurczak T, Klimaszyk P (2015) The multidisciplinary approach to safety and toxicity assessment of microalgae-based food supplements following clinical cases of poisoning. Harmful Algae 46:34–42
Heller HJ, Greer LG, Haynes SD, Poindexter JR, Pak CY (2000) Pharmacokinetic and pharmacodynamic comparison of two calcium supplements in postmenopausal women. J Clin Pharmacol 40:1237–1244
Tondapu P, Provost D, Adams-Huet B, Sims T, Chang C, Sakhaee K (2009) Comparison of the absorption of calcium carbonate and calcium citrate after Roux-en-Y gastric bypass. Obes Surg 19:1256–1261
Pak CYC, Poindexter J, Finlayson B (1989) A model system for assessing physicochemical factors affecting calcium absorbability from the intestinal tract. J Bone Miner Res 4:119–127
EFSA (2009) Calcium acetate, calcium pyruvate, calcium succinate, magnesium pyruvate magnesium succinate and potassium malate added for nutritional purposes to food supplements. EFSA J 1088:1–25
Herda TJ, Ryan ED, Stout JR (2008) Effect of a supplement designed to increase ATP levels on muscle strength, power output, and endurance. J Int Soc Sports Nutr 5:3
Egras AM, Hamilton WR, Lenz TL, Monaghan MS (2011) An evidence-based review of fat modifying supplemental weight loss products. J Obes. doi:10.1155/2011/297315
Stone MH, Sanborn K, Smith LL et al (1999) Effects of in-season (5 weeks) creatine and pyruvate supplementation on anaerobic performance and body composition in American football players. Int J Sports Nutr 2:146–165
Acknowledgments
The study was financially supported by the Phytolab GmbH & Co in the form of a scientific grant. We would like to thank all volunteers for their participation in our study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
The research was conducted on human volunteers, and it was approved by the Bioethics Committee of Poznan University of Medical Sciences and was in conformance with the Declaration of Helsinki and CONSORT statement. Written informed consent was obtained from all participants before inclusion in the trial.
Conflict of interest
None.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rzymski, P., Pischel, I., Conrad, F. et al. The bioavailability of calcium in the form of pyruvate, carbonate, citrate–malate in healthy postmenopausal women. Eur Food Res Technol 242, 45–50 (2016). https://doi.org/10.1007/s00217-015-2516-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00217-015-2516-9