Abstract
Legionella pneumophila are pathogenic bacteria that can be found in high concentrations in artificial water systems like evaporative cooling towers, which have been the source of frequent outbreaks in recent years. Since inhaled L. pneumophila can lead to Legionnaires’ disease, the development of suitable sampling and rapid analysis strategies for these bacteria in aerosols is therefore of great relevance. In this work, different concentrations of viable L. pneumophila Sg 1 were nebulized and sampled by the cyclone sampler Coriolis® µ under defined conditions in a bioaerosol chamber. To quantify intact Legionella cells, the collected bioaerosols were subsequently analyzed by immunomagnetic separation coupled with flow cytometry (IMS-FCM) on the platform rqmicro.COUNT. For analytical comparison, measurements with qPCR and cultivation were performed. Limits of detection (LOD) of 2.9 × 103 intact cells m−3 for IMS-FCM and 7.8 × 102 intact cells m−3 for qPCR indicating a comparable sensitivity as in culture (LOD = 1.5 × 103 culturable cells m−3). Over a working range of 103 − 106 cells mL−1, the analysis of nebulized and collected aerosol samples with IMS-FCM and qPCR provides higher recovery rates and more consistent results than by cultivation. Overall, IMS-FCM is a suitable culture-independent method for quantification of L. pneumophila in bioaerosols and is promising for field application due to its simplicity in sample preparation.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over recent years, there have been repeated news about outbreaks of Legionella resulting from the release of bioaerosols from evaporative cooling systems [1,2,3]. To establish rapid quantification of pathogens in aerosols by culture-independent methods, which are based on immunoassays or molecular biological methods, it must be proven that these approaches achieve similar results as by culture. Additionally, sampling strategies that are compatible with such rapid analysis need to be verified. This raises the need to explore ways of studying viable pathogens in bioaerosols in the laboratory without the risk of exposure. Nebulizing and bioaerosol sampling must be performed in bioaerosol chambers in laboratories of class 2 or higher [4]. In this work, such a protocol was implemented in a bioaerosol chamber [5] for the first time with active Legionella. These bacteria occur in more than 50 species, the most common pathogenic one being Legionella pneumophila [6]. The term Legionella species (Legionella spp.) includes all species. The specific species L. pneumophila, in turn, can be divided in serogroups (Sg), which are differentiated by the structure of their lipopolysaccharides (LPS), a component on the outside of their membranes [7]. L. pneumophila Sg 1 is the most frequent cause of infection, accounting for over 70% of cases, and it is the most common causative agent for the disease legionellosis [8, 9]. This includes Legionnaires’ disease, an infection similar to pneumonia, and Pontiac fever, a milder form that resembles a cold and often goes unnoticed [10]. A common exposure way is the inhalation of contaminated bioaerosols within a size range of 1–5 µm, as those airborne particles reach the alveoli area in the lung where they can cause an infection [11]. A very frequent polluter of Legionella in bioaerosols are evaporative cooling systems. In such systems, process water is cooled by heat exchange between water and air. To increase the cooling effect, the water is nebulized to generate small droplets. If the process water is contaminated with Legionella, the chance is given that they are transported in droplets to the outside of the tower up to several kilometers away from the source where they represent a health risk when inhaled [12]. Since in case of an outbreak fast laboratory results are necessary to identify the source of a contamination, rapid detection methods are needed.
The analysis of Legionella by cultivation is still the gold standard, even though cultivation comes with many disadvantages. First, the long analysis time of up to 10 days bears the risk of possible outbreaks of Legionella before results become available. Second, the presence of other microflora can overgrow Legionella colonies, so that a quantification may prove difficult. Third, Legionella can enter a viable-but-not-culturable (VBNC) state, making them undetectable through cultivation, which leads to an underestimation of the concentration [13,14,15,16]. Dietersdorfer et al. [17] showed that VBNC Legionella pneumophila Sg 1 are still virulent in human macrophages, albeit with reduced efficiency. This is of particular importance in the case of aerosols, as the collection process for analysis can cause bacteria to enter stress situations and switch to the metabolically inactive status. Although they are still pathogenic, they will not be detected by cultivation.
For these reasons, the establishment of culture-independent analytical methods for bioaerosols is highly recommended. A molecular biological technique for the detection of L. pneumophila is the quantitative polymerase chain reaction (qPCR). In addition to high sensitivity and specificity [18,19,20,21], it has a low limit of detection (LOD) of, for example, 1.6 × 102 genomic units (GU) L−1 [20] or 80 GU L−1 [21]. With the ability to measure 96 samples at once and to determine the distribution between living and dead cells, there are many advantages of this bioanalytical method. On the other hand, a DNA extraction has to be performed beforehand, which requires skilled personnel to minimize loss of DNA. In environmental samples, inhibiting compounds also represent a source of error [13, 15, 22, 23]. Despite these drawbacks, qPCR is a promising culture-independent method for the detection of L. pneumophila in water and aerosol as already demonstrated in past research [19, 24, 25]. A distribution between intact and damaged cells becomes also possible with qPCR when adding a dye that binds covalently to the DNA of cells with damaged cell membranes and inhibits the amplification [26]. Propidium monoazide (PMA) and ethidium monoazide (EMA) are examples of such dyes [25,26,27].
The immuno-analytical platform rqmicro.COUNT, which relies on a combination of antibody-based immunomagnetic separation (IMS) and flow cytometry (FCM) in a microfluidic plastic cartridge, is a promising new measurement system for the rapid detection of L. pneumophila. The general advantage over other flow cytometry systems is that no washing steps of the fluidic system are needed, which reduces maintenance and unwanted carry-over. Furthermore, the combination of IMS and FCM enables measurements in complex matrices which is often a big challenge of FCM [28, 29]. It was shown before [30,31,32], that in principle IMS coupled with FCM is suitable for the analysis of L. pneumophila in different water matrices, but the approach has not yet been investigated with aerosols. Here, magnetic particles are coupled to a panel of monoclonal anti-L. pneumophila Sg 1 antibodies that enable the separation of bacteria cells from other particles of the matrix. The quantification via FCM takes place through the addition of green fluorochromes, also coupled to anti-L. pneumophila Sg 1 antibodies, and in the following referred to as staining dye [33]. Advantages of this method are the low analysis time of 2 h and the absence of elaborate sample pre-treatment. Through the further addition of the red dye propidium iodide (PI), which only enters cells with damaged cell membranes, a distribution between intact (viable) and damaged (dead) cells becomes possible [26].
So far, the analysis of process water is preferred over that of the emitted air since an easier sampling can be applied. Nevertheless, the analysis of aerosols can have benefits, for example for testing drift eliminators efficiencies. In addition, it is not fully investigated whether other sources, like biofilm in the cooling tower, can lead to an emission of Legionella. To enable direct sampling of bioaerosols, a suitable aerosol sampler with sufficient physical and biological sampling efficiency is required. Hereby, the physical sampling efficiency is the recovery of the particles in the collected aerosol, whereas the biological sampling efficiency states additionally the survival of bacteria during the collection process [34]. Because of difficulties in the decontamination of particle counters, it is challenging to measure the total amount of particles for pathogens. Therefore, in our work, the sampling efficiency of total and viable Legionella is determined by combining the sampler with the respective detection method. By nebulizing a defined bacteria concentration, a calibration of the measurement system can be achieved.
There are various kinds of aerosol samplers available which show different sampling efficiencies. With cyclone sampling, in this case the Coriolis® µ, the cells are captured in a liquid, which improves the viability of bacteria through less drought stress [35]. When entering the sampler, the air flows in a spiral pattern causing a vortex in which particles larger than the cut-off diameter accumulate on the walls due to inertia and centrifugal forces. The air then leaves the sampler through an outlet on the top [36]. These kinds of samplers are less prone to re-entrainment of particles than other sampling techniques like impingement or impaction [37, 38] and are suitable to collect particles above a size of 0.5 µm according to the manufacturer. With an airflow of 100–300 L min−1, it shows a high sampling volume compared to other samplers. Previous experiments with inactivated L. pneumophila in aerosols indicated a sampling efficiency of 42% for the Coriolis® µ [39], but so far, no studies have been conducted with living Legionella.
In this study, L. pneumophila Sg 1 of defined concentrations was nebulized with specified droplet sizes in a bioaerosol chamber and subsequently collected with the cyclone sampler Coriolis® µ. For the first time, to our knowledge, the IMS-FCM method was applied to analyze L. pneumophila in aerosols. This measuring system was then compared to cultivation and qPCR to evaluate their suitability for analysis of L. pneumophila in aerosols. Total Legionella count (TLC) as well as intact Legionella count (ILC) were compared to derive the physical and biological sampling efficiency of the Coriolis® µ sampler depending on the cell concentration and the used analytical detection method.
Material and methods
Bacteria cryo standard
Bacteria solutions were obtained from a L. pneumophila Sg 1 Subtype Bellingham cryo standard (produced from strain DMSZ 25214, see Supplementary Information) with a TLC of 4.82 × 107 cells mL−1 and an ILC of 4.77 × 107 cells mL−1. Cryo stocks are a 1:1 mixture of bacteria suspended in Evian water (purchased from local store) and cryo buffer (122 g L−1 K2HPO4, 14 g L−1 KH2PO4, 85 g L−1 NaCl, 20 g L−1 BSA, and 120 g L−1 Dextran 40 in deionized water, all chemicals from Sigma-Aldrich, St. Louis, USA). The produced cryo stocks were stored at − 80 °C until further use. Through dilution in Ringer’s solution (B.Braun, Melsungen, Germany), the intended concentrations of bacteria solutions were achieved.
Preparation of aerosol samples
For the aerosolization, four different concentrations between 103 and 106 cells mL−1, relating to TLC, and sterile Ringer’s solution as a blank (0 cells mL−1) were nebulized and sampled. The ILC is slightly less (99% ILC) than the TLC. Therefore, concentrations in the range of 9.87 × 101 cells mL−1 to 9.92 × 105 cells mL−1, relating to ILC, were achieved. Five milliliters of the bacterial solutions was put in the nebulizer vessel. For each concentration, three bacterial solutions and one blank were nebulized. All nebulizer vessels were weighed before and after the nebulizing process to obtain the amount of generated aerosol. Collection vessels of the Coriolis® µ sampler were filled with 10 mL sterile Ringer’s solution as collection liquid. The vessels were weighed before the filling and after the sampling to determine the remaining amount of sample. Because of liquid loss due to evaporation, the vessels were filled up to 10 mL with sterile Ringer’s solution afterwards.
Collection of aerosols
Aerosol generation and collection took place in a bioaerosol chamber in a Bio2 laboratory. The modified glove box has HEPA-filters on openings for incoming and outgoing air so a constant air flow through the chamber can be realized. It is operated at negative pressure to avoid any safety risks while working with pathogen aerosols. The chamber is described in detail elsewhere [5]. Sampling was done with the cyclone sampler Coriolis® µ (Bertin, Montigny-le-Bretonneux, France), while nebulizing was performed with a PARI LC PLUS® Nebulizer (Pari GmbH, Starnberg, Germany) and a PARI BOY® Compressor (Pari GmbH, Starnberg, Germany). Nebulizer and sampler were started at the same time and aerosols were collected for 10 min with a flow rate of 300 L min−1. Afterwards, collection vessels were removed from the chamber through a sluice for further analyzation.
Measurements with IMS-FCM
For measurements with IMS-FCM on rqmicro.COUNT, the samples needed to be contained in a defined medium (10 mM phosphate buffer with pH 7.4, 150 mM NaCl/KCl, 1% BSA, 0.05% Tween-20) for proper interaction with the antibodies of magnetic particles and staining dye. Therefore, a solution containing 100 mM phosphate (80 mM Na2HPO4, 20 mM KH2PO4), 10% BSA, and 0.5% Tween-20 was prepared in deionized water (all chemicals from Sigma-Aldrich, St. Louis, USA) and subsequently diluted 1:10 in the sample (therefore results need to be multiplied with a factor of 1.11). The required chloride concentration was already covered by Ringer’s solution. Ten microliters of magnetic particles Sg 1 (rqmicro, Schlieren, Switzerland) and 10 µL staining dye Sg 1 (rqmicro, Schlieren, Switzerland) were added to 200 µL of the prepared samples followed by an incubation for 1 h at RT on an overhead shaker (rqmicro, Schlieren, Switzerland). After incubation, 800 µL of buffer 1 (rqmicro, Schlieren, Switzerland) was added to the samples. One milliliter thereof was then transferred into the cartridge (rqmicro, Schlieren, Switzerland). For determination of TLC, 2 mL of 1 × PBS (137 mM NaCl, 2.7 mM KCl, 8 mM Na2HPO4, 2 mM K2PO4) and 0.05% Tween-20 were added to the buffer wells; for ILC measurements, 2 mL of PI containing buffer 2 (rqmicro, Schlieren, Switzerland). Magnetic particles, staining dye, buffer 1, and buffer 2 were part of the rqmicro L.p. SG1 DETECT Kit (31010) (rqmicro, Schlieren, Switzerland). Measurements were performed on the device rqmicro.COUNT (rqmicro, Schlieren, Switzerland) that combines immunomagnetic separation with flow cytometry. With one cartridge, four samples could be measured simultaneously within 49 min. All samples were measured in triplicate.
DNA extraction
DNA extraction was performed with a foodproof® StarPrep Two Kit (Biotecon, Potsdam, Germany). Therefore, 700 µL of the sample was used without further treatment except for determination of living cells, where 300 µL of D-Reagent (Biotecon, Potsdam, Germany) was added as well. All further steps were conducted according to the manual of the kit. Prepared DNA extracts were stored at − 20 °C until use.
Measurements with qPCR
qPCR measurements were performed with a microproof® Legionella Quantification LyoKit (Biotecon, Potsdam, Germany) according to ISO/TS 12869:2019, where 25 µL of DNA extract was added to the Quantification Kit according to the manual. Afterwards, qPCR was conducted on a qPCR Tower3 G (Analytik Jena, Germany). A negative control (PCR-H2O) and two positive controls (standards A and D from the Quantification Kit) were added to all measurement runs to check that the system worked properly. The measuring program was run with thermal cycling conditions stated in the manual. In one run, L. pneumophila, L. pneumophila Sg 1, and Legionella spp. were measured simultaneously. All DNA extracts were measured in triplicate.
Cultivation
0.1 mL, 0.3 mL, and 0.5 mL of each sample were plated on BCYE agar plates (Xebios Diagnostics, Düsseldorf, Germany) with different dilutions. The plates were incubated at 37 °C for 10 days in a CO2 incubator (Binder, Tuttlingen, Germany). Colonies were counted after 5, 7, and 10 days.
Data evaluation
For aerosol measurements, the aerosol factor had to be considered. It refers to the volume of nebulized bacteria solution relative to the end volume in the collection vessel, which is 10 mL in our experiments. This factor serves to convert measured counts from collection vessels to the number of L. pneumophila in aerosols.
Recoveries before (Recoveryassay) and after (Recoveryaerosol) aerosolization were calculated as follows:
The LOD for aerosols (LODaerosol) was determined with the following equation as stated elsewhere [39].
where LODmethod is the LOD of the respective analytical method, Vend is the end volume in collection vessel, Q is the flow rate of the sampler, t is the sampling time, and η is the sampling efficiency. Sampling efficiency equals recoveryaerosol (see Table 1).
Results and discussion
Droplet spectrum
As a result of the characterization of generated aerosols by PARI LC PLUS® nebulizer, Fig. S1 shows the cumulative mass distribution. Fifty percent of the mass fraction falls within a droplet size range above and below a mass mean diameter (MMD) of 6.3 µm, respectively, whereas 80% of the mass falls in the range between 2.3 and 12 µm. As it is stated elsewhere [40], the generated droplet sizes in our experiments are in the right range to not only carry bacteria cells but also to reach the thoracic region as well. Therefore, they are suitable to simulate the droplets in the environment that can cause an infection. In addition, according to Carvalho et al. [41], the Coriolis® µ sampler shows physical sampling efficiencies between 41 and 92% for particles with a diameter of 2.4 to 10 µm. While these values are not directly comparable to our results due to differences in experimental conditions, they provide a rough estimate of what to expect.
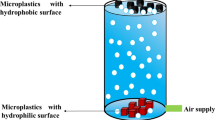
Experimental setup
To characterize any bioanalytical method for pathogens in bioaerosols, nebulizing and aerosol sampling has to be performed in a bioaerosol chamber as shown in Fig. 1. Throughout the experimental setup, it was possible to perform experiments with viable L. pneumophila Sg 1 in bioaerosols without the risk of exposure. Cyclone sampling is a favorable method for many applications because the bacteria cells are transferred from air into an aqueous medium from which sample detection can directly be taken.
Experimental setup for experiments with aerosols. Bioaerosols were generated with a PARI LC PLUS® nebulizer and collected with the cyclone sampler Coriolis® µ in a bioaerosol chamber. Nebulizer and sampler were placed within a distance of 5 cm. After finishing the sampling process, the collection vessels were taken out of the chamber through a sluice. By adding magnetic particles and a staining dye, the IMS procedure and FCM measurements were performed successively on the measuring device. In addition, a DNA extraction followed by qPCR and analysis by cultivation were conducted
IMS-FCM
For data evaluation, the IMS-FCM analysis platform rqmicro.COUNT generates dot plots by plotting green against red fluorescence. A default gate, which was set by the manufacturer for drinking water and was adjusted for aerosol samples, was used for counting of events. The adjustment was necessary because a different matrix than drinking water was used, which can lead to a slight shift of events. To prevent events from the background in the gate, it was manually adjusted directly on the device. Blank measurements were used to distinguish between events of the background and the cells. In Fig. 2A, the dot plot of the TLC measurement for 105 cells mL−1 nebulized L. pneumophila Sg 1 is shown. On the left outside the gate, the background noise of the device is visible, while events in the gate represent stained bacteria cells. As here only the green staining dye was used, intact and damaged cells are both measured. Accordingly, the total count of L. pneumophila Sg 1 results in 3.3 × 104 cells mL−1 after considering dilution factors. In comparison, Fig. 2B shows the result after adding PI which intercalates with double-stranded DNA of damaged cells. This means damaged cells are shifted in the direction of red fluorescence and are now outside the gate. The events remaining in the gate represent bacteria with intact cell membranes which include active and VBNC L. pneumophila Sg 1. A concentration of 2.4 × 104 ILC cells mL−1 was determined for this sample.
A, B Received dot plots from the measurements of green and red fluorescence with IMS-FCM of nebulized 105 cells mL−1. A, TLC; B, ILC, with dead cells shifted to red fluorescence. C, D Correlation between applied and measured concentration in cells mL−1 of Legionella pneumophila Sg 1 for IMS-FCM. Measuring points (number of measurements (m) = 4 for aerosol; m = 5 before aerosolization) before (spiked concentration in nebulizer vessel) and after aerosolization (found concentration in Coriolis® µ vessel) were added. C, TLC and D, ILC. Error bars represent replicate measurements (number of replicates (n) = 3)
For TLC as well as for ILC, recoveryassay without aerosolization (Eq. 2) and recoveryaerosol (Eq. 3) are responsible for loss in cell concentration compared to the applied bacteria concentration. For recoveryassay, 53.7 ± 23.8% for TLC and 52.9 ± 6.2% for ILC were calculated. Both recoveries show similar results for ILC as well as for TLC, so the system is suitable for both kinds of measurements. For TLC, a 17.6% higher standard deviation is seen, which can be justified by the different techniques. During TLC measurements, antibodies of staining dye and magnetic particles bind to all cells with LPS structures of L. pneumophila Sg 1, even those with damaged cell membranes. Damaged cells have the disadvantage of coagulation effects, which can interfere with the measurements. For ILC measurements, only intact cells are considered and coagulation effects are reduced.
Since the results received with IMS-FCM are given as cells mL−1 for TLC and ILC, respectively, they can directly be correlated to those of the applied concentrations in the nebulizer. The plotting of applied against measured concentration for TLC before aerosolization (Fig. 2C) demonstrates a linear correlation (Pearson r (ρ) = 0.996, number of measurements m = 5, for linear regressions, see Table S1). After aerosolization, there is still an identical linear correlation between applied cells and sampled cells (ρ = 0.997, m = 4). By looking at the measurements of ILC (Fig. 2D), similar results compared to TLC can be recognized. A linear correlation before (ρ = 0.999, m = 5) and after (ρ = 0.996, m = 4) aerosolization is given.
Blank measurements with nebulized Ringer’s solution were also added to the graph. When comparing the results of these measurements before and after the aerosolization, an increase of 41.0 cells mL−1 for TLC and of 82.9 cells mL−1 for ILC is visible. This can be explained by possible carry-over during the collection process with the sampler in the aerosol chamber, where the possibility of remaining bacteria in the air or the sampler is given.
In addition, the LODs for ILC and TLC were calculated. Here, it can be distributed between LOD of the detection method (LODmethod) and the LOD with aerosols (LODaerosol). LODmethod was calculated by adding three times the standard deviation of blank measurements to the mean value of blank measurements in aerosols. This results in 2.4 × 102 cells mL−1 for applied TLC and 5.5 × 102 cells mL−1 for applied ILC. With these results, the LODaerosol could be calculated by using Eq. (4), with Vend = 10 mL; Q = 0.3 m3 min−1; t = 10 min; and ηTLC = 0.64, ηILC = 0.63. This resulted in LODaerosol, TLC = 1.3 × 103 cells m−3 and LODaerosol, ILC = 2.9 × 103 cells m−3.
All these results lead to the assumption that this method coupled with aerosol sampling is suitable to gain consistent results for Legionella pneumophila Sg 1 in aerosols.
qPCR
With the used qPCR kit, genes specific to L. pneumophila, L. pneumophila Sg 1, and Legionella spp., referred to as target genes, can be determined simultaneously. Figure 3 shows the measured Ct values before as well as after aerosolization for the respective concentrations. Because L. pneumophila Sg 1 was used for the experiments, positive results for all three target genes are expected.
Correlation curves (m = 5 (before aerosolization); m = 4 (aerosol)) between applied concentrations and Ct values measured by qPCR. Results are given for three different genes before (spiked concentration in nebulizer vessel; brighter colors) and after (found concentration in Coriolis® µ vessel; lighter colors) aerosolization. Results for TLC on the left, for ILC on the right. Error bars represent replicate measurements (n = 3)
Plotting of applied concentrations before aerosolization against measured Ct values demonstrates a linear correlation for TLC as well as for ILC in the range of 102–106 cells mL−1 for all three target genes (all ρ ≥ 0.997, m = 5). After the nebulizing and sampling process, no decline in the correlations can be identified (ρ ≥ 0.997, m = 4). This indicates that the extraction process works equally consistent even with different concentrations for Legionella in aerosols and suggests that the measurement system is suitable for these kinds of measurements.
In addition, blank measurements with nebulized Ringer’s solution were performed before and after aerosolization but no Ct value could be obtained. Since with IMS-FCM an increase in blank values after aerosolization was found, this increase would be expected to occur as well with qPCR but was not confirmed. It is likely that the concentrations in the blank may be too low to detect with qPCR. For determination of concentrations of Legionella in aerosols, measurements before aerosolization were used as a calibration. The respective linear equations are summarized in Table S2.
For calculation of LODaerosol, Eq. (4) is applied. Since no value for the blank measurements could be determined, 100 cells mL−1 (TLC) and 98.7 cells mL−1 (ILC) were used as the lower limit of the working range of the method because it was the lowest measured concentration before aerosolization in our experiments that shows a positive signal and is in the linear range. This value is comparable to the LOD of 65 GU mL−1 specified by the manufacturer. The comparability of our results with LODs from literature, as stated before, indicates a suitable DNA extraction with minimal loss. The first step in the extraction process is centrifugation to form a pellet. After adding lysis buffer and performing the extraction, the whole amount of liquid is removed as DNA extract for further measurements. This presumably leads to a high yield of DNA at the end. With Vend = 10 mL; Q = 0.3 m3 min−1; t = 10 min; ηTLC = 0.35; and ηILC = 0.42, LODaerosol, TLC = 9.5 × 102 cells m−3 and LODaerosol, ILC = 7.8 × 102 cells m−3 were calculated.
Cultivation
For cultivation, the nebulized sample concentrations were given in cells mL−1, but results were obtained in CFU mL−1. Comparing applied concentrations to the number of colonies on the plates (Fig. 4), the decrease in found concentration showed that even before aerosolization only 27.5 ± 7.5% of the cells formed a colony.
However, we can state that there is a linear correlation between applied cells and measured concentration before aerosolization (ρ = 0.999, m = 5). By comparing this with results after aerosolization, it can be recognized that there is a reduced linear correlation (ρ = 0.950, m = 4) and recoveryaerosol is less (30.9 ± 18.0%), compared to IMS-FCM and qPCR. It should also be mentioned that some results with aerosols show an error bar’s overlap through high standard deviations. This can be reasoned with the presence of bacteria in the VBNC state which is induced by the nebulizing and sampling procedure of the aerosols. It indicates that the percentage of L. pneumophila in this state is not always the same, which results in high standard deviations. This leads to the conclusion that the Coriolis® µ sampler may impact the physiological state of cells and is also a confirmation for the need to establish culture-independent methods.
LODmethod was calculated considering the recommendation of the German Federal Environmental Agency [42], which states that results are significant when three or more colonies can be counted on the growth medium. In our experiments, we used 0.1 mL as the minimal sampling volume so LODmethod would be 30 CFU mL−1, which equals 1.4 × 102 cells mL−1. With Vend = 10 mL; Q = 0.3 m3 min−1, t = 10 min, and η = 0.31, a LODaerosol = 1.5 × 103 cells m−3 was calculated.
Comparison of applied methods
When comparing the recoveries in the aerosol, it has to be noted that with ILC measurements for IMS-FCM and qPCR, intact cells (active and VBNC) are measured, whereas for cultivation, only culturable cells are determined. With IMS-FCM, only L. pneumophila Sg 1 is detectable through antibodies, while with the applied qPCR kit, three different target genes can be analyzed. With cultivation, it cannot be differentiated between species or serogroups, so only statements about the number of Legionella spp. can be made.
The recoveries of bacteria in aerosols for all three methods are summarized in Table 1. They directly demonstrate the sampling efficiencies of the Coriolis® µ in combination with different analytical methods. With the ratio of ILC to TLC, the biological sampling efficiency can be determined as well.
For IMS-FCM, 63.7 ± 34.1% of TLC and 63.0 ± 13.5% of ILC could be found after the sampling. For the combination of IMS-FCM and Coriolis® µ sampler, this shows a higher medial sampling efficiency, but also higher standard deviation compared to 42 ± 9% found in Langer et al. [39]. There, inactivated bacteria were sampled in the same way but analyzed by microarray. Other samplers, like the All-Glass Impinger 30 (AGI-30) or the Andersen cascade impactor, showed recoveries between 38–77% [39, 43] and 36–71% [44], respectively. Differences compared to the Coriolis® µ can occur through different physical sampling principles and the used analytical method. In addition, the biological sampling efficiency of the Coriolis® µ is 99%, which means that the forces during the sampling procedure are not destroying the cells, just have influence on the physiological state as the results by cultivation showed.
By looking at the results of qPCR, the three target genes show very similar results for TLC with a recoveryaerosol of 35.4 ± 0.4%, whereas for ILC, a recoveryaerosol of 42.4 ± 2.3% was obtained. This would lead to the conclusion that the mean biological sampling efficiency of the sampler would be 120.2 ± 5.0%. Normally, we would expect a decrease in survival due to strong forces in the aerosol sampler, so it is likely that the increase in survival has its source in the extraction or measurement process. The measurements of the DNA extracts for TLC and ILC were performed on different days and with the use of the aerosol factor. Even small differences in Ct values add up in the calibration curve as well as in the aerosol samples and lead to an increase of concentrations at the end. Another explanation can be the use of the D-reagent for ILC measurements that may have an influence on the higher recoveries for ILC measurements.
When comparing the results of IMS-FCM and qPCR, differences between these two methods can be seen. Since measurements of both methods were performed with the same samples, the sampling efficiency of the Coriolis® µ sampler would be expected to be identical, still there are differences between the recoveries. This can be explained either through the sampling or measurement process. For the first one that would indicate that bacteria are changed during the collection in a way that they behave different at the extraction process. During the first centrifugation step in the extraction, bacteria build a pellet on the ground of the vial. Free DNA remains in the supernatant and is therefore removed with it. It was shown before [45, 46] that centrifugation can have an influence on the integrity of cell membranes. In our experiments, it is possible that cell membranes are weakened through the forces in the sampler. Even small forces during centrifugation can now lead to a rupture of weakened cells and to a release of free DNA. Since centrifugation of the sample is not necessary with IMS-FCM, this would explain the higher recoveries with this method.
With 30.9 ± 18.0%, the lowest recoveryaerosol could be found with cultivation, which was expected because of the VBNC state. This confirms, as stated before in previous studies [19,20,21], that there is an underestimation of bacteria concentrations through cultivation. Another disadvantage of this method is the long analysis time of 10 days, whereas with IMS-FCM, a result is obtained within 2 h and with qPCR (including extraction) within 4 h. It is often stated that cultivation has a high sensitivity because even low numbers of colonies can be analyzed. However, by our results, it was demonstrated that not every cell forms a colony. Therefore, only taking colonies into account indicates an underestimation of the real number of bacteria cells. When stating the results in cells mL−1, LODaerosol of cultivation rises above that of qPCR. Comparing this with received LOD by IMS-FCM, values in the same range as by cultivation can be seen. In combination with a better recovery and a lower measurement time, this speaks for the practicality of the established IMS-FCM method. qPCR still shows the lowest LOD but is more laborious due to the needed DNA extraction beforehand.
Previous studies addressed the analysis of real samples of emitted air from water-bearing systems. Ishimatsu et al [47] detected 90 CFU m−3 around cooling towers, whereas Mathieu et al. [48] stated over 103 cells m−3 during an outbreak in France. Blatny et al [49] found 3.3 × 103 CFU m-3 at a biological treatment plant. But as the given data are mostly not stated in cells m−3, it is difficult to compare it to our results. Nevertheless, our analytical methods are promising to detect concentrations that occur in the environment of evaporative cooling systems.
Conclusion
We were able to show that IMS-FCM is suitable for the rapid quantification of viable and dead L. pneumophila Sg 1 cells in bioaerosols with a prior aerosol sampling by the Coriolis® µ. The consistency of the results across all concentrations was demonstrated along with a high biological sampling efficiency of 99%. Additionally, we showed that this culture-independent method provides a wider range of information, such as distribution between intact and damaged cells or a defined serotype. Because of several disadvantages of cultivation regarding detection time and underestimation in aerosols due to bacteria in the VBNC state, more research about culture-independent methods is needed. In comparison to qPCR, no elaborate sample preparation is required, and results are obtained in a shorter time. Furthermore, the results with IMS-FCM showed higher recoveries for TLC and ILC.
We have shown that IMS-FCM is a simple and rapid method that is promising for field measurements to quantify emission of L. pneumophila from evaporative cooling or other nebulizing water systems. With this, emission measurements of L. pneumophila could be performed more frequently to improve Legionnaires’ disease risk assessment.
The entire experimental setup is also promising to be adapted to investigate different types of bioaerosols. This can be useful for conducting studies on the bioanalytical characterization of cultivation-independent methods with viable pathogenic bacteria or active viruses.
References
Maisa A, Brockmann A, Renken F, Lück C, Pleischl S, Exner M, Daniels-Haardt I, Jurke A. Epidemiological investigation and case–control study: a Legionnaires’ disease outbreak associated with cooling towers in Warstein, Germany, August–September 2013. Eurosurveillance. 2015;20. https://doi.org/10.2807/1560-7917.ES.2015.20.46.30064.
Exner M, Kramer A, Eikmann T, Suchenwirth R, Pleischl S, Nissing W, Hartemann P, Koch C, Teichert-Barthel U, Heudorf U, Engelhart S, Churchill WS. Memorandum zu dem Legionellen-Ausbruch in Ulm 2010 aus Sicht von Hygiene und Öffentlicher Gesundheit. Umweltmed Forsch Prax. 2010;15:43–57.
Sabria M, Alvarez J, Dominguez A, Pedrol A, Sauca G, Salleras L, Lopez A, Garcia-Nuñez MA, Parron I, Barrufet MP. A community outbreak of Legionnaires’ disease: evidence of a cooling tower as the source. Clin Microbiol Infect. 2006;12:642–7. https://doi.org/10.1111/j.1469-0691.2006.01447.x.
Burnett LAC, Lunn G, Coico R. Biosafety: guidelines for working with pathogenic and infectious microorganisms. Curr Protoc Microbiol. https://doi.org/10.1002/9780471729259.mc01a01s13.
Kiwull B, Wunderlich A, Herr CEW, Nießner R, Seidel M. Bioaerosolkammer für legionellenhaltige Duschaerosole. Gefahrstoffe-Reinhaltung der Luft. 2016;76:344–5.
World Health Organization. Legionella and the prevention of legionellosis.
Jang H, Kim HS, Moon SC, Lee YR, Yu KY, Lee BK, Youn HZ, Jeong YJ, Kim BS, Lee SH, Kim JS. Effects of protein concentration and detergent on endotoxin reduction by ultrafiltration. BMB Rep. 2009;42:462–6. https://doi.org/10.5483/BMBRep.2009.42.7.462.
Borchardt J, Helbig JH, Lück PC. Occurrence and distribution of sequence types among Legionella pneumophila strains isolated from patients in Germany: common features and differences to other regions of the world. Eur J Clin Microbiol Infect Dis. 2008;27:29–36. https://doi.org/10.1007/s10096-007-0392-3.
Declerck P, Behets J, Delaedt Y, Margineanu A, Lammertyn E, Ollevier F. Impact of non-Legionella bacteria on the uptake and intracellular replication of Legionella pneumophila in Acanthamoeba castellanii and Naegleria lovaniensis. Microb Ecol. 2005;50:536–49. https://doi.org/10.1007/s00248-005-0258-0.
Shaheen M, Scott C, Ashbolt NJ. Long-term persistence of infectious Legionella with free-living amoebae in drinking water biofilms. Int J Hyg Environ Health. 2019;222:678–86. https://doi.org/10.1016/j.ijheh.2019.04.007.
Sturm R. Modeling the deposition of bioaerosols with variable size and shape in the human respiratory tract - a review. J Adv Res. 2012;3:295–304. https://doi.org/10.1016/j.jare.2011.08.003.
Committee on Management of Legionella in Water Systems. Management of Legionella in water systems. https://doi.org/10.17226/25474.
Bonetta S, Bonetta S, Ferretti E, Balocco F, Carraro E. Evaluation of Legionella pneumophila contamination in Italian hotel water systems by quantitative real-time PCR and culture methods. J Appl Microbiol. 2010;108:1576–83. https://doi.org/10.1111/j.1365-2672.2009.04553.x.
Kober C, Niessner R, Seidel M. Quantification of viable and non-viable Legionella spp. by heterogeneous asymmetric recombinase polymerase amplification (haRPA) on a flow-based chemiluminescence microarray. Biosens Bioelectron. 2018;100:49–55. https://doi.org/10.1016/j.bios.2017.08.053.
Boss R, Baumgartner A, Kroos S, Blattner M, Fretz R, Moor D. Rapid detection of viable Legionella pneumophila in tap water by a qPCR and RT-PCR-based method. J Appl Microbiol. 2018;125:1216–25. https://doi.org/10.1111/jam.13932.
Saad M, Chinerman D, Tabrizian M, Faucher SP. Identification of two aptamers binding to Legionella pneumophila with high affinity and specificity. Sci Rep. 2020;10. https://doi.org/10.1038/s41598-020-65973-3.
Dietersdorfer E, Kirschner A, Schrammel B, Ohradanova-Repic A, Stockinger H, Sommer R, Walochnik J, Cervero-Aragó S. Starved viable but non-culturable (VBNC) Legionella strains can infect and replicate in amoebae and human macrophages. Water Res. 2018;141:428–38. https://doi.org/10.1016/j.watres.2018.01.058.
Eble D, Gehrig V, Schubert-Ullrich P, Köppel R, Füchslin HP. Comparison of the culture method with multiplex PCR for the confirmation of Legionella spp. and Legionella pneumophila. J Appl Microbiol. 2021; 131:2600–2609. https://doi.org/10.1111/jam.15103.
Walser SM, Brenner B, Wunderlich A, Tuschak C, Huber S, Kolb S, Niessner R, Seidel M, Höller C, Herr CEW. Detection of Legionella-contaminated aerosols in the vicinity of a bio-trickling filter of a breeding sow facility – a pilot study. Sci Total Environ. 2017;575:1197–202. https://doi.org/10.1016/j.scitotenv.2016.09.191.
Collins S, Stevenson D, Bennett A, Walker J. Occurrence of Legionella in UK household showers. Int J Hyg Environ Health. 2017;220:401–6. https://doi.org/10.1016/j.ijheh.2016.12.001.
Ditommaso S, Ricciardi E, Giacomuzzi M, Arauco Rivera SR, Ceccarelli A, Zotti CM. Overestimation of the Legionella spp. load in environmental samples by quantitative real-time PCR: pretreatment with propidium monoazide as a tool for the assessment of an association between Legionella concentration and sanitary risk. Diagn Microbiol Infect Dis. 2014;80:260–266. https://doi.org/10.1016/j.diagmicrobio.2014.09.010.
Bedrina B, Macián S, Solís I, Fernández-Lafuente R, Baldrich E, Rodríguez G. Fast immunosensing technique to detect Legionella pneumophila in different natural and anthropogenic environments: comparative and collaborative trials. BMC Microbiol. 2013;13.
Kirschner AKT. Determination of viable legionellae in engineered water systems: Do we find what we are looking for? Water Res. 2016;93:276–88. https://doi.org/10.1016/j.watres.2016.02.016.
Nocker A, Schulte-Illingheim L, Frösler J, Welp L, Sperber O, Hugo A. Microbiological examination of water and aerosols from four industrial evaporative cooling systems in regard to risk of Legionella emissions and methodological suggestions for surveillance. Int J Hyg Environ Health. 2020;229. https://doi.org/10.1016/j.ijheh.2020.113591.
Chang CW, Chou FC. Assessment of bioaerosol sampling techniques for viable Legionella pneumophila by ethidium monoazide quantitative PCR. Aerosol Sci Technol. 2011;45:343–51. https://doi.org/10.1080/02786826.2010.537400.
Emerson JB, Adams RI, Román CMB, Brooks B, Coil DA, Dahlhausen K, Ganz HH, Hartmann EM, Hsu T, Justice NB, Paulino-Lima IG, Luongo JC, Lymperopoulou DS, Gomez-Silvan C, Rothschild-Mancinelli B, Balk M, Huttenhower C, Nocker A, Vaishampayan P, Rothschild LJ. Schrödinger’s microbes: tools for distinguishing the living from the dead in microbial ecosystems. Microbiome. 2017;5:86. https://doi.org/10.1186/s40168-017-0285-3.
Kontchou JA, Nocker A. Optimization of viability qPCR for selective detection of membrane-intact Legionella pneumophila. J Microbiol Methods. 2019;156:68–76. https://doi.org/10.1016/j.mimet.2018.12.003.
Rajapaksha P, Elbourne A, Gangadoo S, Brown R, Cozzolino D, Chapman J. A review of methods for the detection of pathogenic microorganisms. Analyst. 2019;144:396–411. https://doi.org/10.1039/c8an01488d.
Gruden C, Skerlos S, Adriaens P. Flow cytometry for microbial sensing in environmental sustainability applications: current status and future prospects. FEMS Microbiol Ecol. 2004;49:37–49. https://doi.org/10.1016/j.femsec.2004.01.014.
Füchslin HP, Kötzsch S, Keserue HA, Egli T. Rapid and quantitative detection of Legionella pneumophila applying immunomagnetic separation and flow cytometry. Cytometry A. 2010;77:264–74. https://doi.org/10.1002/cyto.a.20858.
Keserue HA, Baumgartner A, Felleisen R, Egli T. Rapid detection of total and viable Legionella pneumophila in tap water by immunomagnetic separation, double fluorescent staining and flow cytometry. Microb Biotechnol. 2012;5:753–63. https://doi.org/10.1111/j.1751-7915.2012.00366.x.
Ortí-Lucas RM, Luciano E. New immunomagnetic separation method to analyze risk factors for Legionella colonization in health care centres. J Expo Sci Environ Epidemiol. https://doi.org/10.1038/s41370-022-00421-0.
Keserue H-A. Validation of the Legionella pneumophila SG1 DETECT Kit for quantification of Legionella pneumophila Serogroup 1 bacteria in potable waters, process waters and surface waters: AOAC Performance Tested Method SM 052002. https://doi.org/10.1093/jaoacint/qsaa126/5900662.
Verein Deutscher Ingenieure. VDI 4252 Blatt 3 - Erfassung luftgetragener Mikroorganismen und Viren in der Außenluft - Aktive Probenahme von Bioaerosolen.
Ghosh B, Lal H, Srivastava A. Review of bioaerosols in indoor environment with special reference to sampling, analysis and control mechanisms. Environ Int. 2015;85:254–72. https://doi.org/10.1016/j.envint.2015.09.018.
Lindsley WG, Green BJ, Blachere FM, Martin SB, Law BF, Jensen PA, Schafer MP. Sampling and characterization of bioaerosols. NIOSH Manual of Analytical Methods (NMAM) 2–115.
Abdel-Salam M. Aerosol sampling methods in workplace and ambient environments. J Aerosol Med. 2006;19:434–55.
de Sousa NR, Shen L, Silcott D, Call CJ, Rothfuchs AG. Operative and technical modifications to the Coriolis® μ air sampler that improve sample recovery and biosafety during microbiological air sampling. Ann Work Expo Health. 2020;64:852–65. https://doi.org/10.1093/ANNWEH/WXAA053.
Langer V, Hartmann G, Niessner R, Seidel M. Rapid quantification of bioaerosols containing L. pneumophila by Coriolis® μ air sampler and chemiluminescence antibody microarrays. J Aerosol Sci. 2012;48:46–55. https://doi.org/10.1016/j.jaerosci.2012.02.001.
Allegra S, Leclerc L, Massard PA, Girardot F, Riffard S, Pourchez J. Characterization of aerosols containing Legionella generated upon nebulization. Sci Rep. 2016;6. https://doi.org/10.1038/srep33998.
Carvalho E, Sindt C, Verdier A, Galan C, O’Donoghue L, Parks S, Thibaudon M. Performance of the Coriolis air sampler, a high-volume aerosol-collection system for quantification of airborne spores and pollen grains. Aerobiologia (Bologna). 2008;24:191–201. https://doi.org/10.1007/s10453-008-9098-y.
Umweltbundesamt. Empfehlung des Umweltbundesamtes zur Probenahme und zum Nachweis von Legionellen in Verdunstungskühlanlagen, Kühltürmen und Nassabscheidern.
Zhao Y, Aarnink AJA, Doornenbal P, Huynh TTT, Koerkamp PWGG, Landman WJM, De Jong MCM. Investigation of the efficiencies of bioaerosol samplers for collecting aerosolized bacteria using a fluorescent tracer. II: Sampling efficiency and half-life time. Aerosol Sci Technol. 2011; 45:432–442. https://doi.org/10.1080/02786826.2010.543197.
Xu Z, Wei K, Wu Y, Shen F, Chen Q, Li M, Yao M. Enhancing bioaerosol sampling by Andersen impactors using mineral-oil-spread agar plate. PLoS ONE. 2013;8. https://doi.org/10.1371/journal.pone.0056896.
Pembrey RS, Marshall KC, Schneider RP. Cell surface analysis techniques: what do cell preparation protocols do to cell surface properties? Appl Environ Microbiol. 1999;65:2877–94.
Peterson BW, Sharma PK, van der Mei HC, Busscher HJ. Bacterial cell surface damage due to centrifugal compaction. Appl Environ Microbiol. 2012;78:120–5. https://doi.org/10.1128/AEM.06780-11.
Ishimatsu S, Miyamoto H, Hori H, Tanaka I, Yoshida S-I. Sampling and detection of Legionella pneumophila aerosols generated from an industrial cooling tower. Ann Occup Hyg. 2001;45:421–7.
Mathieu L, Robine E, Deloge-Abarkan M, Ritoux S, Pauly D, Hartemann P, Zmirou-Navier D. Legionella bacteria in aerosols: sampling and analytical approaches used during the Legionnaires disease outbreak in Pas-de-Calais. J Infect Dis. 2006;193:1333–1335. https://doi.org/10.1086/503115.
Blatny JM, Reif BAP, Skogan G, Andreassen O, Høiby EA, Ask E, Waagen V, Aanonsen D, Aaberge IS, Caugant DA. Tracking airborne Legionella and Legionella pneumophila at a biological treatment plant. Environ Sci Technol. 2008;42:7360–7. https://doi.org/10.1021/es800306m.
Acknowledgements
The funding via AiF within the program for promoting the Industrial Collective Research (IGF, FKZ: 21747N) of the Federal Ministry of Economic Affairs and Climate Action (BMWK), based on a resolution of the German Parliament, is gratefully acknowledged.
The authors would like to thank Björn Biedermann and Damien Morger for advice about the IMS-FCM measurements on the rqmicro.COUNT and Analytic Jena for the provision of the qTower3 G.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
L. Heining conceived and conducted the experiments of aerosolization and quantification. L. Heining analyzed the results and wrote the manuscript with input from the co-authors. L. Welp and A. Hugo performed and analyzed the measurements for the droplet spectrum and wrote the corresponding parts of the manuscript. M. Elsner and M. Seidel supervised the project and were responsible for funding acquisition and resources.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Published in the topical collection Recent Trends in (Bio)Analytical Chemistry with guest editors Antje J. Baeumner and Günter Gauglitz.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heining, L., Welp, L., Hugo, A. et al. Immunomagnetic separation coupled with flow cytometry for the analysis of Legionella pneumophila in aerosols. Anal Bioanal Chem 415, 5139–5149 (2023). https://doi.org/10.1007/s00216-023-04738-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-023-04738-z