Abstract
Since the SARS-CoV-2 pandemic, the potential of exhaled breath (EB) to provide valuable information and insight into the health status of a person has been revisited. Mass spectrometry (MS) has gained increasing attention as a powerful analytical tool for clinical diagnostics of exhaled breath aerosols (EBA) and exhaled breath condensates (EBC) due to its high sensitivity and specificity. Although MS will continue to play an important role in biomarker discovery in EB, its use in clinical setting is rather limited. EB analysis is moving toward online sampling with portable, room temperature operable, and inexpensive point-of-care devices capable of real-time measurements. This transition is happening due to the availability of highly performing biosensors and the use of wearable EB collection tools, mostly in the form of face masks. This feature article will outline the last developments in the field, notably the novel ways of EBA and EBC collection and the analytical aspects of the collected samples. The inherit non-invasive character of the sample collection approach might open new doors for efficient ways for a fast, non-invasive, and better diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
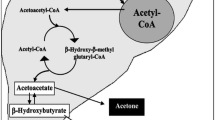
Exhaled breath (EB) analysis has shown great potential to provide valuable insight into the personal health status and is rapidly evolving as a new diagnostic matrix next to blood and urine [1,2,3,4,5,6,7,8,9]. Breath analysis counts on the unique ability of the human lung to provide “biofluids” directly from the organ with every breath. The rich information encoded in EB can be extracted with modern mass spectrometry (MS) instruments, which are able to identify thousand of unique substances in EB [10]. Breathomics has become a steadily evolving field focusing on the understanding of the nature of EB components such as carbon dioxide (CO2), oxygen (O2), or nitric oxide (NO) as well as other volatile organic compounds (VOCs) (e.g., acetone, isoprene, ammonia, ethanol). Upon breathing, various gases, such as nitrogen (80%), oxygen (20%), and other gases (including 0.04% carbon dioxide), enter the lungs and reach the alveoli, the endpoint of the respiratory tract, where gas exchange takes place: oxygen diffuses from the alveoli into the pulmonary capillaries and into the blood to support cells, while the waste from the breakdown of sugars in the cells, CO2, diffuses back into the blood and then into the lungs and is expelled when breathing out, closing the gas exchange circle (Fig. 1).
EB comprises not only gases and VOCs, but also water droplets ranging from < 1 μm (droplets suspended in the air in the form of aerosols) to 1000 μm in size (only briefly suspended aerosols) with around 100 droplets L−1 in healthy patients [11, 12]. With a general breathing rate of 10 L min−1, this accounts for 1000 droplets min−1. The content of these breathing droplets is non-volatile metabolites, salts, lipids, protein biomarkers, and virus and pathogens particles, in fact, anything that was adsorbed or trapped on the surface of the respiratory tract. The condensed water vapor fraction is often referred to as exhaled breath condensate (EBC) [2, 13], whereas the aerosolized particle fraction, when collected separately, is termed exhaled breath aerosols (EBA) [14, 15]. Collecting such respiratory droplets as EBC is achieved by cooling the air exhaled by an object [13, 16, 17] and results in the collection of non-volatile biomarkers for analysis using a range of established analytical techniques. While the use of EBC has a simplified “breath print” compared to EB as it is constituted exclusively of water-soluble non-volatile compounds, surprisingly, it remains less intensively used as medium for analysis compared to EB.
Utilizing EB for disease diagnostics is not a new concept and dates back to Greek civilization where breath was used to diagnose diabetics via the fruity smell of ketoacidosis. The twentieth century witnessed remarkable advancements in the field of breath investigation. Linus Pauling is considered as the father of modern breath analysis. He analyzed frozen breath with gas chromatography (GC) and differentiated > 250 volatile molecules [18]. Despite the demonstration of the potential of EB to mirror pathological processes taking place locally in the lung and systemically via blood circulation, it can be collected in a non-invasive manner, making the approach personalizable. However, technical and statistical challenges have delayed until now the larger translation of EB technology for real-world applications. Although mass spectrometry (MS) continues to play an important role in biomarker discovery, breath analysis needs to move toward online sampling and be connected to portable, room temperature operable, user-friendly analytical technologies to make the transition to clinical steups more timely.
The SARS-CoV-2 pandemic had a positive impact in this field via the proposition of alternative breath collection approaches often mask-based systems [19,20,21], and the consideration of compiling with portable biosensors for immediate analysis, eliminating many of the confounding variables introduced by breath collection and sample storage [19,20,21,22,23,24,25]. The approaches are different from those of bioelectronic noses, and intelligent sensor arrays used to identify gases and vapors [26]. Unlike biosensors, these devices cannot identify the specific compound responsible for the smell print, but detect patterns and are not designed to work for protein biomarkers or viral particle detection. The advances on the use of EBC for protein biomarker detection will be the focus of this feature article and will hopefully generate further work in this exciting area at the interface between analytical chemistry, materials science, and engineering. Before discussion of the analytical aspects, below is some discussion about EBC collection.
EBC collection considerations
The appealing aspect of using EBC as sample collection mode for biomarker detection is related to its non-invasive nature. Compared to blood but also to nasal and bronchoalveoal lavage in case of respiratory diseases, EBC presents a much larger area of the lung respiratorey fluid and does not alter the physiology of the respiratory tract lining (Table 1).
Despite the ease of accessibility, biomarker levels might be affected by a number of physiological and environmental factors and need to be considered and controlled during the collection process. This was exemplified by the sensing of glucose levels in EBC [3]. Most of commercially available EBC collection devices (Fig. 2a) rapidly cool the collected EBC, and the formed condensate forms droplets on surfaces made out of silicon or Teflon. The drawback of this collection approach (Table 2) is the long time required for collecting 1-mL sample volume, necessary in most cases for an accurate analysis. To condense EBC into 1-mL liquid volume, breathing for at least 10 min is required [27]. For glucose sensing, this is inconvenient as it does not allow real-time glucose level changes in small time intervals (< 5 min). Another issue concerns the dilution factor due to water vapor collected in the respiratory fluid as EBC. When respiratory fluid is aerosolized and travels up from the lower airways to the mouth, it is diluted with droplets of water vapor. This makes it difficult to determine if glucose concentration changes are due to dilution or to physiological changes of glucose in the fluid lining. The use of non-volatile reference solutions based on sodium, potassium, or chloride ions has been proposed [28]. Another dilution factor of EBC is the inclusion of anatomic dead space air, the air from the upper respiratory tract (nose, mouth) that does not participate in gas exchange, in the condensed exhaled air samples. Temperature profiling and CO2 measurements can insure to distinguish between dead space and deep lung air (Fig. 2b) [17]. A micromachined silicon chip was proposed by Stanborg et al. recently for the collection of exhaled viral particles (Fig. 2c) [29].
Exhaled breath collection systems. a Polypropylene-based R-tube collector. The ability to pool the sample near the upper end of the tube allows for maximum sample recovery of 75–150 μL min−1 for a child and 100–250 μL min−1 for an adult at normal tidal breathing. b Temperature selective EBC collection approach based on temperature and CO2 profile change during breathing (reprint with permission of ref. [17]). c Design of a disposable sampling device for viral particles in breath together with top view of the sieve (22 × 22 mm2) consisting of an array of 1600 nozzles with a diameter of 150 μm. Exhaled particles are collected on the bottom sieve by inertial impaction, while air and very small particles (< 300 nm) are directed to the outlet nozzles and exit (reprint with permission from Ref. [29])
Masks seem ideally suited for the collection of EBA [20, 23, 24, 31] and EBC [19]. In 2014, Barer and coworkers modified already a FP30 face mask by cutting a 5.5-cm2 opening from the center, into which an equivalent-sized gelatin membrane with 3-mm pore size was attached in a custom-made detachable plastic holder secured with autoclave tape and applied for sampling of Mycobacterium tuberculosis (Fig. 3a) [30]. Integrating a detachable medical adhesive with a porous polycarbonate membrane (200 nm), which ensures airflow to pass and collects viral particles, was proposed as an efficient virus-concentrator-based wearable collector [31]. Different mask-based EBC collection systems have been developed since the onset of the COVID-19 pandemic. Our team together with others has retrofitted commercial face masks with a polytetrafluoroethylene (PTFE)-based cooling trap (Fig. 3b), which upon cooling in a freezer for 30 min allows the collection of 400 ± 150 μL of EBC within 5 min, enough for further analysis by RT-PCR or an electrochemical sensor as we will see later [19].
Mask-based collection of EBC and EBA. a FP30 mask with filter adapted for sampling (reprint with permission of Ref. [30]). b Photograph of a retrofitted face mask with a polytetrafluoroethylene (PTFE)-based cooling trap allowing to collect 400 ± 150 μL of EBC within 5 min [19]. c Intelligent sensing mask based on a layered mask architecture to collect and sense the presence of virus particles (with permission from Ref. [24])
The group of Duan reported at the same time the advantages of an intelligent face mask as part of a point-of-care system [24]. The collection of exhaled breath virus aerosol particles was possible via a three-layered mask, comprising a polycarbonate membrane of 400-nm pore size to collect the sample, and a nanowire assay with ligands as sensing layer deposited on a flexible substrate as bottom-supporting layer to facilitate the adhesion of the sensor to the mask (Fig. 3c). Vaquer et al. trapped viral proteins in surgical masks containing a hydrophobic polypropylene (PP) layer, which provides also liquid barrier protection [23].
Biosensors interfaced with EBC collection
It is well-known that the major mechanisms of COVID-19 spread are airborne and contact infections primarily due to the high resistance of the virus once in aerosol droplets expelled from infected persons. The study by Ryan and coworkers [32] with a 93.5% concordance between RT-PCR results of nasopharyngeal and EBC samples collected with R-tube condensers on volunteers with a positive or negative RT-PCR test for SARS-CoV-2 strongly supported the hypothesis that EBC-collected samples are suitable for SARS-CoV-2 detection [32]. Motivated by this finding, the thermal properties of a silicon impact chip (Fig. 2d) [29] were used to collect EBC from SARS-CoV-2-infected people and used the collection chip for direct RT-qPCR. Of the 40 clinical samples tested, 32 were correctly identified (80% agreement). In a clinical study using engineered face masks (Fig. 3d) [19] and 5-min breathing, some of us could showed lately a 73% positive percentage agreement (PAA) (25 out of 34 positive samples) using a Ct cutoff of 33 and a 100 negative percentage agreement (NPP) (20 out of 20 negative samples) (Fig. 4a). Interestingly, the Ct values measured in EBC were, besides one exception, > 30, equivalent to about (7 ± 2) × 104 copies mL−1 using an experimentally determined correlation between RT-qPCR Ct counts and viral RNA copies mL−1 (Fig. 4b) [33]. With an estimated 200–1400 virus particles exhaled per minute [31], 5-min breathing should result in about (0.1-0.7) × 104 copies mL−1. The viral load collected in the masks seems to be an order of magnitude larger (Fig. 4a) and might point toward the importance of sample collection and a general improvement with a mask-based closed system.
EBC and EBA analyses, a Correlation of Ct values of nasopharyngeal swab and EBC samples collected from the same patient upon breathing for 5-min into a cooled engineered face mask (unpublished results, clinical trial: Masken Sensor: Elektronischer Biosensor für die Exhalationskondensatdiagnostik zum Nachweis von SARS-CoV-2. GZ: DPU-EK/016, agreement 22.02.2022. b Correlation of RT-qPCR Ct counts and viral RNA copies mL−1 of SARS-CoV-2 clade 20A.EU2 (EU variant). The results are expressed as the mean ± SEM of at least 3 independent electrodes for each group [34]
In addition to proper control for collecting EBC, EBC analysis needs to be integrated into the collection concept for reaching a point-of-care testing device. Biosensors, which are analytical devices that incorporate biologically derived recognition elements converting analyte-biorecognition events into detectable signal changes, are ideally suited. One of the first approaches is that by Shen et al. [35], who demonstrated the selective detection of influenza A viruses down to 2.9 × 104 copies mL−1 in EBC samples within minutes using silicon nanowire (SiNW) sensor devices [35]. Gold nanoparticles modified with anti-nucleoprotein antibodies were used to reveal the presence of SARS-CoV-2 viral particles on the polymer lining of breathing masks after wearing for 30–120 min [23]. A linear relation between 0.3 and 100 ng mL−1 N-protein was determined with the possibility to discriminate infected and non-infected people upon colorimetric readout (Fig. 5a). Using porcine transmissible gastroenteritis virus (TGEV) as model for virus aerosols, an impedimetric sensor integrated in a face mask with cell phone-based readout could detect TGEV spiked breath at 7 pfu mL−1 (Fig. 5b) [24]. This detection limit is reasonable when compared to the infectivity limit for SARS-CoV-2 clade 20A.EU2 (EU variant), determined as10 ± 1 pfu mL−1 (5.9 × 104 copies mL−1) [33].
Biosensors for EBC-based virus analysis. a Concept of colorimetric detection of SARS-CoV-2 viral particles via Au NPs modified with anti-nucleoprotein antibodies (inset) and optical signal (S) of volunteers having been breathing for 30 min (reprint with permission of Ref. [23]). b Peak impedance values of breath spiked with different TGEV viral loads: yellow: 0 pfu mL−1 (control), red: 7 pfu mL−1, blue: 700 pfu mL−1, orange: 700 pfu mL−1 of adenovirus. c Dose-dependent response curve toward SARS-CoV-2 virus clade 20A.EU2 (black). All the values are displayed as means ± SEM (n = 5) [19]. c Surface acoustic wave-based aptamer sensor for CEA in EBC collected with a commercial collection device (EcoScreen, Jaeger, Germany) (reprint with permission from Ref. [36]). d Schematics of face-based viral sensor: puncture of the waste reservoir results in moving viral particles collected via respiration to the downstream freeze-dried reactions integrated into the microfluids with final readout using a LFA (reprint with permission from Ref. [21])
Our team has lately used an electrochemical aptasensor, targeting the S1 protein of SARS-CoV-2 with nanomolar affinity, to analyze EBC collected in engineered breathing masks [19]. The sensing sensitivity of the aptasensor to cultured patient-derived SARS-CoV-2 viral particles using differential pulse voltammetry (DPV) readout and ferrocenemethanol as redox mediator was determined to be 10 pfu mL−1 (Fig. 5c). In a proof of principle study, nasopharyngeal and EBC samples of the same volunteer were collected and analyzed by RT-q-PCR and with our aptasensor. Seven of the nasopharyngeal samples were identified as SARS-CoV-2 positive and seven as SARS-CoV-2 negative by targeting the N structural protein as well as the RNA-dependent RNA polymerase (RdRp) nonstructural protein via RT-qPCR. A 100% NPP (7 out of 7) and 71% PPA (5 out of 7) were determined by RT-qPCR as well as with the aptasensor in EBC.
An EBC-based SARS-CoV-2 detection in a face mask based on a combination of technologies notable freeze-dried, cell-free (FDCF) genetic circuits was proposed by Collines and coworkers [21] (Fig. 5d) with a detection limit of 5.0 × 102 copies. The face mask-based sensor contains a reservoir for EB hydration, an EBC collection pat, a waxed-patterned microfluid and a lateral flow assay strip for sensing of lysed virus (Fig. 5d).
Next to virus sensing, there are some reports on the detection of protein biomarkers in EBC [36, 37]. Carcinoembryogenic antigen (CEA), a reported biomarker for lung cancer, was found to be present in EBC collected in a commercial collection device (EcoScreen, Jaeger, Germany) when the temperature of the collection chamber was set to − 10 °C. Using a surface acoustic wave (SAW)-based immunosensor, a limit of detection of 1 ng mL−1 CEA was reached. Investigating EBC samples of 15 healthy subjects with CEA ≤ 5 ng mL−1 and 15 patients with lung cancer and combining chemiluninescence assays with the SAW assay revealed a good correlation (Fig. 6a). We recently added to this field with the demonstration of the presence of a cardiac biomarker, N-terminal-pro hormone BNP (NT-proBNP) in EBC (Fig. 6b) [38] when collecting with engineered face masks, as illustrated in Fig. 2d. Validation on both EBC and blood samples from patients suffering from heart failure secondary to valvular and/or ischemic heart disease during the peri-operative management for cardiac surgery and using ELISA testing showed a concentration-related correlation between EBC NT-proBNP and serum level.
Biosensors for EBC-based protein analysis. a Correlation of EBC carcinoembryogenic antigen concentrations detected by an electrochemical aptasensor or by a chemiluminesence-based ELISA (reprint with permission from Ref. [37]). b Comparison of concentration levels of NT-proBNP in plasma and EBC collected with engineered mask from 14 patients, as determined by the human proBNP IQELISA™ kit (RAyBiotech, IQH-proBNP-1) [38]
Outlook
Breathing is central to life as it gives the human body the required fuel to sustain itself. With each breath, thousands of volatile and non-volatile molecules are expelled and when collected and analyzed adequately are a fingerprint of our health status. Face masks are not only the first-line barriers to help limit the spread of exhaled viral particles, but can be a cost-effective and cost-efficient means to provide us with a non-invasive manner to collect a biological fluid, which can be used for reliable direct diagnosis of individuals with acute respiratory infections and other diseases. Different research groups have targeted this exciting field from the materials as well as molecular diagnostics point of view. The collected samples are currently analyzed with standard molecular analysis approaches, such as polymerase chain reaction (PCR), with mass spectrometry (MS) having been proposed in parallel in some cases. More lately, the integration of biosensors into mask-based EBC collectors with wireless data readout has emerged as an efficient means and a point-of-care testing option. Currently, the examples are limited to a handful and are mainly based on sensing of viral particles. The field is expected to largely open up in the future to the investigation of other respiratory-based diseases. In parallel, considering face mask-based protein biomarker collection and sensing would provide patients with plenty of benefits. In a preclinical study, some of us have validated lately the presence of NT-proBNP in EBC samples collected with engineered facial masks. Cardiovascular diseases (CVDs) remain one of the leading causes of death worldwide and improving therapeutic outcomes and reducing health care costs, as well as obtaining a better understanding of disease-specific variation across cardiac patients, are needed. Emerging technologies such as EBC-based cardiac biomarker sensing will provide opportunities for patients with cardiovascular problems in the form of home diagnosis and therapy. All these activities will require clinical studies to benchmark if and how quantitively blood-derived biomarkers relate to EBC-based biomarker sources. The know-how and input of analytical scientists for protein screening to identification of novel EBC-based biomarkers until the design of sensitive and specific biosensors will be needed to drive this field further. The involvement of clinicians to validate the concept and approve its interest from a clinical point of view as well as the patient itself will be of ultimate need as these approaches put the patient into the center of action. The development of a patient-centered approach to medicine is gradually allowing more patients to be involved in their own medical decisions. This change is not happening at the same rate in clinical research, where research generally continues to be carried out on patients, but not with patients. Mask-based sensors might be one way to bridge both worlds with a benefit for all of us.
References
Vasilescu A, Hrinczenko B, Swain GM, Peteu SP. Exhaled breath biomarker sensing. Biosens Bioelectron. 2022;182:113193.
Nwanochie E, Linnes JC. Review of non-invasive detection of SARS-CoV-2 and other respiratory pathogens in exhaled breath condensate. J Breath Res. 2022;6:024002.
Tanissala D, Linnes JC. Noninvaive glucose detection in exhaled breath condensate. Transl Res. 2019;213:213–22.
Ibrahim W, Carr L, Cordell R, Wilde MJ, Salman D, et al. Breathomics for the clinician: the use of volatile organic compounds in respiratory diseases. Thorax. 2021;76:514.
Cikach FS, Dweik RA. Cardiovascular biomarkers in exhaled breath. Prog Cardiovasc Dis. 2012;55:34–43.
Saktiawati AMI, Putera DD, Setyawan A, Mahendradhata Y. Diagnosis of tuberculosis through breath test: a systematic review. EBioMedicine. 2019;46:202–14.
Orbe DV, Park HJ, Kwack M-J, Lee H-K, Kim DY, et al. Breath analyzer for personalized monitoring of exercise-induced metabolic fat burning. Sens Actuators B. 2022;369:132192.
Wang P, Huang Q, Meng S, Mu T, Liu Z, et al. Identification of lung cancer breath biomarkers based on perioperative breathomics testing: a prospective observational study. eClinicalMedicine. 2022;47:101384.
Güntner AT, Abegg S, Königstein K, Gerber PA, Schmidt-Trucksäss A, et al. Breath sensors for health monitoring. ACS Sens. 2019;4:268–80.
Beccaria M, Mellors TR, Petion JS, Rees CA, Nasir M, et al. Preliminary investigation of human exhaled breath for tuberculosis diagnosis by multidimensional gas chromatography - time of flight mass spectrometry and machine learning. J Chromatogr B Analyt Technol Biomed Life Sci. 2018;1074–1075:46–50.
Almstrand AC, Ljungström E, Lausmaa J, Bake B, Sjövall P, et al. Airway monitoring by collection and mass spectrometric analysis of exhaled particles. Anal Chem. 2009;81:662–8.
Dbouk T, Drikakis D. On respiratory droplets and face masks. Phys Fluid. 2020;32:063303.
Horváth I, Hunt J, Barnes PJ, Alving K, Antczak A, et al. Exhaled breath condensate: methodological recommendations and unresolved questions. Eur Respir J. 2005;26:523–48.
Hu B. Recent advances in facemask devices for in vivo sampling of human exhaled breath aerosols and inhalable environmental exposures. Trend Anal Chem. 2022;151:116600.
Yuan Z-C, Li W, Wu L, Huang D, Wu M, et al. Solid-phase microextraction fiber in face mask for in vivo sampling and direct mass spectrometry analysis of exhaled breath aerosol. Anal Chem. 2020;92:11543–7.
Mutlu GM, Garey KW, Robbins RA, Danzinger LH, Rubinstein I. Collection and analysis of exhaled breath condensate in humans. Am J Respir Crit Care Med. 2001;164:731–7.
Tankasala D, Ng GP, Smith MS, Bendell JR, Linnes JC. Selective collection and condensation of exhaled breath for glucose detection. Annu Int Conf IEEE Eng Med Biol Soc. 2018;218:3892–3.
Pauling L, Robinson AB, Teranishi R, Cary P. Quantitative analysis of urine vapor and breath by gas-liquid partition chromatography. Proc Natl Acad Sci USA. 1971;68(10):2374–6.
Daniels J, Wadekar S, DeCubellis K, Jackson GW, Chiu AS, et al. A mask-based diagnostic platform for point-of-care screening of Covid-19 Biosens. Bioelectron. 2021;192:113486.
Kim H-S, Lee H, Park J, Abbas N, Kang S, et al. Collection and detection of SARS-CoV-2 in exhaled breath using face mask. PLOs Ones. 2022;17:e0270765.
Nguyen PQ, Soenksen LR, Donghia NM, Angenent-Mari NM, de Puig H, et al. Wearable materials with embedded synthetic biology sensors for biomolecule detection. Nat Biotechnol. 2021;39:1366–74.
Xue Q, Kan X, Pan Z, Li Z, Pan W, et al. An intelligent face mask integrated with high density conductive nanowire array for directly exhaled coronavirus aerosols screening. Biosens Bioelectron. 2021;186:113286.
Vasquer A, Alba-Patiño A, Adrover-Jaume C, Russell SM, Aranda M, et al. Nanoparticle transfer biosensors for the non-invasive detection of SARS-CoV-2 antigens trapped in surgical face masks. Sens Actuators B. 2021;345:130347.
Xue Q, Kan X, Pan Z, Li Z, Pan W, et al. An intelligent face mask integrated with high density conductive nanowire array for directly exhaled coronavirus aerosols screening Biosens. Bioelectron. 2021;186:113286.
Galliani M, Ferrari LM, Ismailova E. Interdigitated organic sensor in multimodal facemask’s barrier integrity and wearer’s respiration monitoring. Biosensors. 2022;12:305.
Dung TT, Oh Y, Choi S-J, Kim I-D, Oh M-K, et al. Applications and advances in bioelectronic noses for odour sensing. Sensors. 2018;18:103.
Hunt J. Exhaled breath condensate—an overview. Immunol Allergy Clin North Am. 2007;27:587.
Effros RM, Hoagland KW, Bosbous M, Castillo D, Foss B, et al. Dilution of respiratory solutes in exhaled condensates. Am J Respir Crit Care Med. 2002;165:663–9.
Stakenborg T, Raymenants J, Taher A, Marchal E, Verbruggen B, et al. Molecular detection of SARS-COV-2 in exhaled breath at the point-of-need. Biosens Bioelectron. 2022;217:114663.
Williams CML, Cheah ESG, Malkin J, Patel H, Otu J, et al. Face mask sampling for the detection of Mycobacterium tuberculosis in expelled aerosols. PLOs Ones. 2014;9:e104921.
Soto F, Ozen MO, Guimarães CF, Wang J, Hokanson K, et al. Wearable collector for noninvasive sampling of SARS-CoV-2 from exhaled breath for rapid detection. ACS Appl Mater Interfaces. 2021;13:41445–53.
Ryan DJ, Toomey S, Madden SF, Casey M, Breathnach OS, et al. Use of exhaled breath condensate (EBC) in the diagnosis of SARS-COV-2 (COVID-19). Thorax. 2021;76:86–8.
Pagneux Q, Roussel A, Saada H, Cambillau C, Amigues J, et al. SARS-CoV-2 detection using a nanobody-functionalized voltammetric device. Commun Med. 2022;2:56.
Dӧrfler H, Ladage D, Daniel J, Wadekar S, Boukherroub R, Szunerits S. RT-qPCR based diagnosis of the presence of SARS-CoV-2 in exhaled breath condensate collected with novel face maks. unpublished results.
Shen F, Wang J, Xu Z, Wu Y, Chen Q, et al. Rapid flu diagnosis using silicon nanowire sensor. Nano Lett. 2012;12:3722–30.
Zou Y, Zhou Y, Chen Y, Zhang X, Ran C. Love wave based portable sensing system for on-line detection of carcinoembryonic antigen in exhaled breath condensate. Biomed Microdev. 2020;22:78.
Zhang X, Zou Y, An C, Ying K, Chen X, et al. Sensitive detection of carcinoembryonic antigen in exhaled breath condensate using surface acoustic wave immunosensor. Sens Actuators B. 2015;217:100–6.
Pagneux Q, Woitrain E, Maud H, Daniel J, Wadekar S, et al. (2022) Exhaled NT-proBNP as a exhaled breath biomarker. unpublished results.
Funding
This work received financial support from the Centre National de la Recherche Scientifique (CNRS) and the University of Lille.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Szunerits, S., Dӧrfler, H., Pagneux, Q. et al. Exhaled breath condensate as bioanalyte: from collection considerations to biomarker sensing. Anal Bioanal Chem 415, 27–34 (2023). https://doi.org/10.1007/s00216-022-04433-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-022-04433-5