Abstract
Ketamine has received considerable attention for its rapid and robust antidepressant response over the past decade. Current evidence, in clinical populations, predominantly relates to parenterally administered ketamine, which is reported to produce significant undesirable side effects, with additional concerns regarding long-term safety and abuse potential. Attempts to produce a similar drug to ketamine, without the psychotomimetic side effects, have proved elusive. Orally administered ketamine has a different pharmacological profile to parentally administered ketamine, suggesting it may be a viable alternative. Emerging evidence regarding the efficacy and tolerability of oral ketamine suggests that it may be a favourable route of administration, as it appears to obtain similarly beneficial treatment effects, but without the cost and medical resources required in parenteral dosing. The pharmacological effects may be due to the active metabolite norketamine, which has been found to be at substantially higher levels via oral dosing, most likely due to first-pass clearance. Despite bioavailability and peak plasma concentrations both being lower than when administered parenterally, evidence suggests that low-dose oral ketamine is clinically effective in treating pain. This may also be due to the actions of norketamine and therefore, its relevance to the mental health context is explored in this narrative review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ketamine, an N-methyl-D-aspartate (NMDA) receptor antagonist, is one of only a handful of drugs that acts primarily on the glutamatergic system. Whilst it has been used as an anaesthetic agent for the past 50 years, only recently has it generated interest in the mental health arena (Nowacka and Borczyk 2019). Its rapid acting antidepressant effects have been well documented in the treatment of depression and other stress related disorders via intravenous (IV) dosing (Murrough et al. 2013; Feder et al. 2014; Taylor et al. 2018). Its rapid effect is related to the pharmacokinetics, with high lipid solubility, low levels of protein binding, fast penetration of the blood–brain barrier, rapid redistribution and rapid elimination (2–3 h post-dosing) (Palucha-Poniewiera 2018). More recently, oral ketamine has garnered attention (Rosenblat et al. 2019) and it potentially provides a more practical and less costly treatment option in a real-world setting, where it is highly scalable to meet clinical demand. Though the bioavailability of oral ketamine is significantly lower at between 17 and 25%, most likely due to first-pass metabolism, compared to intravenous (IV) dosing at 97% (Palucha-Poniewiera 2018) it presents an interesting case showing comparable efficacy to intravenous dosing (Can et al. 2021). Whilst the exact mechanism for this is unknown it has been postulated to be due to the effects of the main metabolite, norketamine. Studies show blood concentrations of norketamine are substantially higher following oral administration than when administered by other routes (Clements and Nimmo 1981, Clements et al. 1982) and this may contribute to the efficacy observed in oral dosing. Additionally, evidence from pain research indicates analgesic effectiveness at lower blood concentrations and a greater longevity of response with oral administration (Grant et al. 1981), than observed in parenteral or intramuscular (IM) dosing, further supporting this notion. Moreover, ketamine’s glutamatergic action is pivotal to both analgesic and antidepressant effects (Peltoniemi et al. 2016), and thus, this review considers the clinical evidence for low-dose oral ketamine, the pharmacological rationale which may underpin the observed treatment effect and the relevance of pain studies for ketamine use in psychiatry. We posit that oral administration of ketamine for depression and suicidality similarly benefits from the norketamine effect observed in analgesia studies and further assert that oral administration of ketamine may be the route of choice, providing desirable clinical effects with less undesirable side effects associated with parenteral dosing. This narrative review was conducted utilising articles found after searches in various databases including SCOPUS, PubMed and Google Scholar with the following key terms: ‘oral’, ‘ketamine’, ‘pharmacokinetics’, ‘pharmacodynamics’, ‘pain’ and/or ‘depression’. Furthermore, manual searches of the reference lists of the papers identified in the database search were undertaken. Finally, the search was conducted in English and only English-language studies were included.
Clinical use in psychiatry
Reports of ketamine’s antidepressant action date back to the 1970s, with preclinical evidence suggesting that ketamine induced similar antidepressant effects as classic antidepressant drugs, in rodent models. Sofia and Harakal reported that oral ketamine displayed significant antidepressant drug activity in mice over a range of doses up to 40 mg/kg (Sofia and Harakal 1975). Whilst, in 1973, a human study of IV ketamine at 0.2–1 mg/kg was reported to result in an improvement in the condition of 100 psychiatric inpatients (Khorramzadeh and Lofty 1973), but it was not until the year 2000 that Berman et al. conducted a placebo-controlled randomised controlled trial (RCT) and established the antidepressant efficacy of ketamine in patients with depression, reporting a robust and rapid treatment response to a 40-min IV infusion of 0.5 mg/kg ketamine versus saline solution (Berman et al. 2000). Zarate et al. replicated this with a double-blinded, placebo-controlled RCT in 2006 (Zarate et al. 2006). They reported treatment response became evident just 2 h post-infusion and lasted for an average of 7 days, in patients with treatment-resistant depression. Murrough et al. introduced the active placebo midazolam in an RCT, reporting ketamine showed a higher response rate (64%) compared to midazolam (28%) in patients with treatment-resistant depression (Murrough et al. 2013). A meta-analysis of 9 RCTs using IV ketamine further supported ketamine’s clinical efficacy, with a significant improvement in depression scores compared to placebo, in 226 patients with major depressive disorder (MDD) or bipolar depression, with duration of effect in longitudinal studies reported at 2–3 days (Fond et al. 2014). The question of whether repeated dosing could induce a more prolonged effect was considered by Singh et al. (2016). A multicentre double-blind trial assessed the efficacy of twice-weekly or thrice-weekly dosing in 68 patients with treatment-resistant depression, for up to 4 weeks. Both dosing regimens were reported as similarly effective, whilst the clinical effect persisted for up to 15 days (Singh et al. 2016). Subsequent studies have shown significant anti-suicidal effects, with reductions in suicidal ideation (Grunebaum et al. 2017, 2018) and anhedonia reported (Murrough et al. 2015; Ballard et al. 2017).
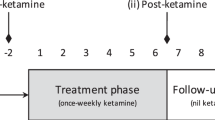
In comparison, reports of oral ketamine have been slower to emerge, potentially due to concerns regarding lower bioavailability (compared to IV), which has been assumed to impact treatment response. However, although numbers are limited, reports of oral ketamine for mental health treatment use, have been largely positive. In 2010, a retrospective study reported oral ketamine (0.5 mg/kg) use in 14 palliative care patients who had comorbid depression and anxiety symptoms. All 8 who completed the 28-day trial reported significant improvement in their mood and anxiety symptoms, with no serious adverse events reported (Irwin et al. 2013). A further early report of 2 patients with chronic suicidal ideation and at least 2 significant past suicide attempts, who received oral ketamine (0.5–3 mg/kg) as an augmentation to existing treatment, indicated an initial improvement within 24 h of the first treatment (De Gioannis and De Leo 2014). Furthermore, the clinical improvement was reported to be sustained with remission of symptoms after additional treatments (every 2–4 weeks) and a high degree of tolerability and no adverse events. A 2019 systematic review on the efficacy and tolerability of oral ketamine found only 13 published articles including 2 RCTs (Rosenblat et al. 2019). They reported the studies were largely low quality, with a high risk for bias and noted heterogeneity in the treatment regimens further hindered analysis. However, the limited evidence indicated that oral ketamine has significant antidepressant effects and is well tolerated, though onset of treatment effect may not be as rapid as observed with IV ketamine (Rosenblat et al. 2019). Whilst, a recent (2023) systematic review of twenty-two studies including four RCTs, a case review, five open-label trials and six retrospective chart review studies, which involved 2336 patients with depression, concluded that significant clinical benefit was derived from oral ketamine treatment and that treatment was well tolerated, with no serious adverse effects reported (Meshkat et al. 2023). Additionally, our group has recently reported a study in which weekly subanaesthetic oral ketamine resulted in similar positive outcomes in a highly complex clinical population (n = 32), with chronic suicidality (Can et al. 2021). Tolerability and feasibility were considered as key aspects of the oral dosing and significant neurobiological outcomes which correlated with the clinical results, were subsequently reported across the six-week treatment period (Gallay et al. 2021; Can et al. 2023a, b). Moreover, anecdotally, the family of participants reported life-changing benefits, which in some cases were sustained well beyond the trial period. Thus, though studies on oral ketamine are limited in numbers and with significant design limitations, early outcomes in human subjects are promising. Additionally, preclinical and clinical evidence strongly suggests that the primary metabolites contribute to ketamine’s therapeutic effects, with norketamine significantly contributing to ketamine’s actions, particularly when administered orally (Grant et al. 1981; Ebert et al. 1997; Shimoyama et al. 1999).
Safety
Whilst it has been shown that oral ketamine is relatively safe in research settings, it is still to be established in a real-world community setting. Though generally considered to be well tolerated, concerns regarding psychotomimetic side effects and abuse potential have been reported (Krystal et al. 1994; Zarate 2022) and non-medical ketamine use (abuse) has been associated with significant urological complications such as dysuria, increased frequency and urgency, incontinence, haematuria and ketamine-associated ulcerative cystitis, which can be irreversible (Ng et al. 2021). Ketamine has been shown to be toxic to the urothelial cells in the bladder and evidence from cystoscopy revealed oedema and epithelial inflammation in populations using long-term non-medical ketamine (Chu et al. 2008). Imaging of non-medically prescribed users further show bladder wall thickening and perivesicular inflammation with one report indicating a case of urinary urgency and incontinence at subanesthetic dosing levels (0.1 mg/kg per h IV over 12 h) (Mason et al. 2010; Vickers et al. 2017). Though evidence suggests most non-medical use of ketamine is via nasal insufflation (30–400 mg), there are reports of non-medical oral ketamine (100–500 mg) use, with plasma concentrations of 50–200 ng/ml enhancing sensory perception, emotional connectedness, feelings of unreality and out of body experiences, in a dose-dependent manner (Zanos et al. 2018). At peak plasma levels, ketamine may induce extreme dissociative experiences characterised by altered states of consciousness and sensory detachment, with these effects often accompanied by blurred vision, dizziness, vomiting and nausea, palpitations and chest pain (Wolff and Winstock 2006). However, the majority of ketamine’s side effects are dose dependent and demonstrated to be transient and self-resolving (Loo et al. 2016) and despite some reinforcing effects, ketamine dependence is considered to be a rare occurrence (Blier et al. 2012). Furthermore, whilst no studies have directly compared ketamine abuse liability across different routes of administration, oral dosing is considered to be less attractive in this regard, due to slower onset of effect when compared to IV and nasal insufflation (Muetzelfeldt et al. 2008). Indeed, our group has identified a pattern of sensitivity where human participants in a longitudinal study required a lowering of dose and this was particularly evident in those who were responsive to the rapid-acting effects (Can et al. 2023a, b). However, caution should be exercised in treating patients with ketamine, particularly in contexts outside of research and where concomitant opioid medications or alcohol use is present. In these situations, a high degree of monitoring for dependence is warranted (Freedman et al. 2018).
Concerns regarding neurotoxic effects have emerged in both preclinical and clinical studies in substance use disorder models/populations, whereby daily high-dose ketamine use has been associated with specific neuropathologies, including Olney lesions (Nogo et al. 2022). Long-term repeated treatment or single high doses of ketamine in rodents also indicate the potential for selective irreversible damage, though these changes were not apparent at lower, clinically relevant doses (Zanos et al. 2018). Additionally, studies in non-human primates indicate a pattern of reduced white matter integrity in fronto-thalamo-temporal connections after 3 months of daily IV administration (Li et al. 2017). Taken together preclinical and clinical evidence indicates specific neuropathologies may be associated with chronic high-dose ketamine exposure, exceeding therapeutic subanaesthetic dosing and given the increasing interest in ketamine use, these concerns require further investigation.
Evidence regarding ketamine’s safety and utility in a community setting has been reported in the extant pain literature. Ketamine has been used as a take-home self-administered treatment in patients with chronic pain, with efficacy and safety data reported. A 5-year retrospective study reported on 51 patients with intractable pain, who were transitioned from IV ketamine infusion to self-administered oral treatment in the home (Marchetti et al. 2015). Daily treatment began at 0.5 mg/kg and titrated up, with 2 mg/kg reported as the mean effective oral dose, with treatment continued for 3 months, followed by a progressive withdrawal. Half of the patients reported adverse effects and 8 ceased treatment due to tolerability issues with three withdrawals due to headaches and four due to psychotomimetic side effects (Marchetti et al. 2015). In a double-blind, RCT of 40 patients with mild to moderate depression and chronic pain, oral ketamine (150 mg per day in 3 divided 50 mg doses) was compared to the same dose of diclofenac across a 6-week treatment period (Jafarinia et al. 2016). Medication was self-administered and adherence was monitored through patient self-reports and weekly capsule counts. Safety data showed that oral ketamine was safe and well tolerated, with no difference in adverse effects between the two groups reported and no patient withdrawal during the treatment period. Both treatments produced similar analgesic efficacy, but ketamine showed a significantly greater improvement in depression (as measured using the Hospital and Anxiety Depression Scale) scores post-treatment (Jafarinia et al. 2016).
However, despite increasing numbers of positive reports, concerns have persisted regarding ketamine’s side effects (Zarate 2022), and thus, efforts have been made to identify alternate targets for drug discovery, based on ketamine’s mechanism of action, with investigations undertaken into candidate drugs which capture ketamine’s beneficial effects, without its less desirable features. NMDA receptor antagonists were thoroughly investigated and whilst some demonstrated partial effectiveness, they lacked ketamine’s rapid and robust effect, as well as its capacity to illicit a sustained response after a single dose and its broad therapeutic potential to treat other stress-induced disorders (Zarate and Machado-Vieira 2017). Furthermore, investigations into AMPA-positive modulators showed variable results with toxicity concerns (Menniti et al. 2013) whilst studies into other glutamate receptor modulating drugs such as glycine site modulators, sub-unit specific NMDA receptor antagonists and mammalian target of rapamycin complex 1 (mTORC1) activators have yielded modest results, when compared to racemic ketamine (Henter et al. 2021).
Chemical properties and pharmacokinetic profile
Chemically, ketamine is a 2-(2-chlorophenyl)-2-(methylamino)-cyclohexane and phencyclidine derivative, with a molecular weight of 237.73 (Zanos et al. 2018). It is highly lipid soluble, but also soluble in water to 20% and has a chiral structure with equal amounts of the two optical enantiomers, S( +) -ketamine and R( −) -ketamine, due to an asymmetrical carbon atom in the C2 position (Schmid et al. 1999; Peltoniemi et al. 2016). Racemic ketamine, as a HCL salt, is commonly utilised for use in humans, though both the S ( +) and R ( −) enantiomers have been investigated, in an effort to manage the side effect profile of parenterally administered ketamine (Zanos et al. 2018; Kaur et al. 2021). Recent evidence indicated R ( −) ketamine may exert neuroprotective effects and longer lasting antidepressant effects, when compared to S ( +) ketamine (Passie et al. 2021).
Analyses report the bioavailability of oral ketamine to be between 16 and 29%, most likely due to extensive first-pass metabolism by the liver, with peak plasma concentrations occurring within 20–120 min (Grant et al. 1981; Clements et al. 1982). After systemic absorption, ketamine’s high degree of lipid solubility and low levels of plasma protein binding (10–30%) facilitate rapid transfer across the blood–brain barrier and distribution into highly perfused tissue, including the brain. A large steady-state volume of distribution (160–550 L/70 kg) follows (Peltoniemi et al. 2016), with the initial effects subsiding as the drug moves from highly perfused tissue into less perfused compartments. Biotransformation occurs in the liver via the cytochrome p450 liver enzyme system, with the major metabolic pathway nitrogen demethylation of the parent drug, by hepatic enzymes CYP2B6 and CYP3A4, to norketamine (Mion and Villevieille 2013). Demethylation occurs in a stereoselective manner with S- ketamine selectively metabolised by CYP3A4 more rapidly than R ketamine (Zanos et al. 2018). Norketamine is subsequently hydroxylated to 6-hydroxynorketamine by CYP2B6 and CYP2A6 enzymes or to dehydroxynorketamine (DHNK) by CYP2B6 (Mion and Villevieille 2013). Elimination occurs through the kidneys after norketamine and other metabolites undergo glucuronide conjugation into water soluble compounds and are finally excreted in the urine and bile, with only a minor percentage of unchanged drug (Haas and Harper 1992). A secondary metabolic pathway is the direct hydroxylation of ketamine to hydroxynorketamine (HNK) and in animal models this may additionally occur in the intestines, liver and lungs (Zanos et al. 2018). Notably, oral administration is associated with higher serum levels of the active metabolite norketamine, compared to other routes of administration. Thus, the bioavailability of ketamine 0.5/mg/kg given orally, is reported at approximately 20% of the availability of parenterally administered treatment, such as an IV infusion. However, importantly, Chong et al. noted that the oral bioavailability of ketamine may reach 59 ± 16%, when allowance is made for norketamine’s contribution (Chong et al. 2006). Additionally, Grant et al. (1981) noted that though the bioavailability of norketamine is similar between the intramuscular and oral routes of administration, significantly higher peak plasma concentrations are found after oral administration (see Table 1).
Similar findings were reported in a small comparison study of ketamine and norketamine plasma concentrations after IV, oral, intranasal, sublingual and rectal administration in healthy volunteers. The area under the plasma concentration–time curve of norketamine was highest for oral administration (500 ng h/ml) in both enantiomers, followed by sublingual and rectal administration (280–460 ng h/ml), with intranasal administration delivering low concentrations of norketamine (100 ng h/ml) in both enantiomers (Yanagihara et al. 2003). Furthermore, the pain literature indicates that the analgesic effects of IM and IV ketamine are observed to occur at plasma levels of 100–200 ng/ml, whereas effective analgesia in oral dosing is achieved at just 40 ng/ml (Grant et al. 1981; Blonk et al. 2010). Taken together, this suggests norketamine may play a significant role in the analgesic effect of orally administered ketamine and this could reasonably also be the case in the antidepressant effect of oral ketamine. Moreover, evidence indicates the high levels of norketamine may contribute to the extended duration of treatment effect after oral administration in pain studies, due to norketamine’s slower rate of elimination, and this is further coupled with enhanced treatment tolerability due to norketamine’s favourable safety profile (White et al. 1982, Holtman et al. 2008.
Ketamine has a high rate of clearance and a short elimination half-life of 2–4 h; however, the therapeutic effect may be prolonged through the active metabolites DHNK, HNK and norketamine, which is reported to have a half-life of up to 12 h (Soto et al. 2012; Zanos et al. 2018). Though recent evidence has questioned the antidepressant efficacy of secondary HNK metabolites (Abdallah 2020). A study on bipolar depression reported evidence of metabolites DHNK and HNK, 3 days after administration, whilst a paediatric study found norketamine was present in the urine 14 days after administration and ketamine 11 days post-administration (Adamowicz and Kala 2005). Furthermore, when compared to adults, children have been shown to metabolise ketamine twice as rapidly (Haas and Harper 1992), suggesting a prolonged exposure to norketamine after oral administration in adults, which may contribute to the therapeutic effect. Additionally, repeated dosing may result in a reduced elimination, with one study of three 0.75–1.59 mg/kg single infusions across a 2-year period reporting decreased clearance on subsequent treatments compared to the first treatment, despite the third treatment being 2 years later (Adamowicz and Kala 2005). Moreover, norketamine accumulation may account for the majority of ketamine’s effect in repeat dosing, and this may explain the reduced need for ketamine in clinical settings, over time (Mion and Villevieille 2013).
However, oral ketamine is more susceptible to individual factors which may affect the bioavailability, including the drug preparation, cytochrome enzyme phenotypes and liver enzyme induction. Ketamine metabolism is a function of liver blood flow with a high hepatic extraction ratio (0.9), and thus, its clearance is sensitive to changes in hepatic blood flow (Haas and Harper 1992). Further factors affecting clearance include the high degree of variability in the expression and catalytic action of the CYP enzymes responsible for ketamine’s metabolism in humans (Nottage et al. 2023). Genetic variability, including CYP2B6 genotypes, may also contribute to the heterogeneity of treatment response, particularly in regard to side effects. The CYP2B6*6 allele is shown to significantly reduce ketamine metabolism resulting in greater plasma concentrations and an associated increase in adverse effects (Li et al. 2015). Furthermore, the influence of enzyme inhibitors and inducers need to be considered, with both shown to have a significant effect on ketamine concentrations after oral administration in healthy volunteers (Peltoniemi et al. 2012). Enzyme induction by rifampicin was shown to significantly reduce the plasma concentrations of both S-ketamine and S-norketamine after oral administration, with the mean area under the plasma concentration–time curve (AUC) decreased by 86% and the peak plasma concentration by 81% (Peltoniemi et al. 2012). Thus, concomitant use of drugs which interfere with ketamine’s CYP3A4- and CYP2B6-mediated elimination will affect the bioavailability of oral treatment.
Additionally, the form of administration may contribute to the treatment outcomes due to differing compounding formulations, as oral ketamine is not commercially available. Oral administration, utilising a sublingual ketamine wafer preparation, has been shown to provide an absolute bioavailability of 29%, notwithstanding the norketamine component, in a study of eight healthy male volunteers (Rolan et al. 2014). Peak plasma concentration was reported at 45 min, though ranged from 25 min to 1 h. Interestingly, the first quantifiable plasma ketamine concentration was recorded within just 5 min when taken orally, which is comparable to IV dosing. However, protocols for oral dosing require further investigation with studies demonstrating considerable heterogeneity in dosing regimens to date (Table 2). Given the pharmacokinetic profile of orally administered racemic ketamine, daily dosing may not be required. Our work (Can et al. 2021) corroborates earlier studies and shows promising evidence for single weekly dosing (De Gioannis and De Leo 2014), though this requires larger scale replication.
Thus, oral ketamine is highly susceptible to pharmacokinetic interactions. Gene-drug interactions and differential drug metabolism due to cytochrome enzyme polymorphisms may affect the efficacy and safety and further impact dosing requirements in clinical practice (Zanos et al. 2018).
Pharmacodynamic effects
Pharmacokinetic studies have reported delayed time to maximum plasma concentrations in oral ketamine dosing compared to other routes; however, the therapeutic effect may be more sustained with oral dosing, in line with the pharmacokinetics of the oral compound (Grant et al. 1981; Chong et al. 2006). Orally administered ketamine undergoes significant first-pass clearance, resulting in lower circulation concentrations and delayed onset of therapeutic effects. However, norketamine has a slower clearance rate and, thus, is thought to be responsible for the more persistent therapeutic effects observed after oral dosing (Mion and Villevieille 2013). Ketamine pharmacodynamics, more generally, have been poorly studied in a mental health context, with limited data regarding optimal AUC values which correlate with the therapeutic effects, pharmacodynamic target engagement and clinical efficacy and toxicity. Additionally, neuronal mechanisms are still to be fully characterised (Lazarevic et al. 2021). Here, we summarise relevant evidence regarding key molecular targets and mechanisms associated with ketamine’s therapeutic effects (see Zanos et al., for a detailed review (Zanos et al. 2018)).
The neuropharmacology of ketamine is complex as it targets several receptors in humans, including nicotinic, muscarinic, mu, delta and kappa opioid receptors, as well as interacting with monoaminergic and voltage gated calcium channels (Mion and Villevieille 2013). It also blocks peripheral and central nervous system sodium channels and further acts as a non-competitive antagonist at the phencyclidine binding site in the NMDA receptor complex channel, where it induces a use-dependent blockade, paradoxically disinhibiting glutamate release (Abdallah et al. 2018). Ketamine is shown to increase the cortical rate of conversion of 13C-glutamate to 13C-glutamine, which is indicative of glutamate release (Abdallah et al. 2018) and through its action at GluN2B subunits enhances synaptic connectivity and plasticity, through increased levels of brain derived neurotrophic factor and increased shuttling of AMPA receptors to the synapse (Krystal et al. 2019). Enhanced activation of the AMPA receptor is considered critical to ketamine’s action and this is thought to work synergistically with the NMDA receptor at the tripartite glutamatergic synapse (Zarate and Machado-Vieira 2017). Thus, ketamine’s initial NMDA receptor blockade increases glutamate release from synapses and the subsequent preferential activation of AMPA facilitates the plasticity signalling cascades, particularly in the cortico-limbic-striatal circuitry, where it enhances synaptic strength (Abdallah et al. 2018). The resulting downstream plasticity effects are responsible for ketamine’s longer lasting effects (beyond actual drug levels) such as altered gene expression and protein regulation and these are reviewed by others (Zarate and Machado-Vieira 2017; Dutton et al. 2022).
Thus, the role of the NMDA receptor in nociception, as well as the neural plasticity processes implicated in mental disorders, has prompted increasing interest in understanding ketamine’s mechanisms of action. Its unique non-competitive antagonism at the NMDA receptor is use dependent, with agonism at a separate receptor site facilitating binding (Mion and Villevieille 2013). Also, the open state is required for ketamine to subsequently dissociate from the binding site, with entrapment in the receptor channel a potential mechanism for ketamine accumulation (Schmid et al. 1999; Mion and Villevieille 2013). Hence, ketamine may be considered a high entrapment antagonist (86%) with a slow off-rate, creating a prolonged tonic blockade and resulting alterations to physiological functions and subsequent clinical effects (Sleigh et al. 2014). Additionally, NMDA receptor activation plays a fundamental role in long-term potentiation but also in opioid hyperalgesia and its analgesic effects are also thought to result from the non-competitive antagonism of the ionotropic NMDA receptors, which are involved in enhanced nociceptive processing in the spine and supraspinal regions (Haas and Harper 1992). NMDA receptor blockage effectively reduces signal propagation in pain neural circuitry resulting in effective analgesia. Opioid receptor binding additionally mediates the analgesic response, with ketamine preferentially binding to mu receptors, and this is thought to be at least partially associated with the antidepressant effect, though potentially through modulation of endogenous opioid pathways with lower risk of dependence (Grunebaum et al. 2020). Though some suggest ketamine’s effects are not analgesic in the traditional sense of the word, rather the NMDA receptor effects reduce ‘wind up’ and central sensitisation, resulting in an additive effect in combination pain management (Schmid et al. 1999). Whilst its distinctive dissociative anaesthetic effects, characterised by profound amnesia, catalepsy and analgesia, are attributed to a functional and electrophysiological separation between the limbic and thalamoneocortical systems (Haas and Harper 1992; Peltoniemi et al. 2016). The dissociative state arises from the brains inability to differentiate afferent impulses because of altered sensory cortex input, with patients in a non-communicative cataleptic state (Marchetti et al. 2015). Imaging studies have further indicated that physical pain activates similar brain areas as emotional pain (i.e. depression, suicidality), with both activating the insula and somatosensory cortex, and the antidepressant effect is thought to contribute to the analgesic response (Romero-Sandoval 2011; Mion and Villevieille 2013). Ketamine further enhances the inhibitory descending serotonergic pathway (Mion and Villevieille 2013). Recent evidence suggests a role for the endocannabinoid system, with CB1 receptor activation implicated in the analgesic effect of ketamine (d’Andrea et al. 2023), whilst blockade of lateral habernula NMDA receptor-dependent burst firing induced significant antidepressant effects and this may be due to ketamine’s modulation of hippocampal theta-band frequencies with resulting disinhibition of downstream monoaminergic reward centres (Yang et al. 2018). Ketamine has been further shown to produce significant increases in neural gamma oscillations in EEG studies and this potential pharmacodynamic biomarker is associated with clinical antidepressant effects (Gilbert and Zarate 2020). Interestingly, a clinical study reported low-range gamma oscillations were associated with higher levels of HNK metabolites and these were associated with poorer clinical outcomes (Farmer et al. 2020) whilst norketamine exposure positively correlated with improved clinical outcomes in another recent EEG study and oral administration of the similar acting glutamatergic antidepressant d-cycloserine (DCS) produced more sustained frontal enhancements compared to the transient effects of IV ketamine, in line with the pharmacokinetics of the oral compound (Nottage et al. 2023).
Discussion and future directions
The emergence of ketamine as a rapid-acting antidepressant has perhaps been the most significant event in the treatment of depression and suicidality in the last decade. However, whilst numerous studies report ketamine’s robust rapid-acting effects, the optimal route of administration is still being elucidated. Recently, oral ketamine has garnered attention for its ease of administration, excellent tolerability and comparable efficacy (Can et al. 2021). Intravenous infusions show efficacy but involve medical complexity (Bahji et al. 2021) and are costly in comparison to orally administered treatment. Additionally, the ambulatory outpatient treatment associated with oral administration offers a more practical and accessible solution that does not require hospital resources. Furthermore, a recent systematic review examined the influence of formulation and route of administration on ketamine’s safety and tolerability, reporting the extent of first-pass metabolism and time to peak plasma concentrations were significantly associated with cardiovascular changes and psychotomimetic effects and concluding that formulations which maximise first-pass metabolism and delay absorption (such as oral formulations) may optimise safety and tolerability (Glue et al. 2021), whilst maintaining the desired clinical effects. Whilst evidence from a recent systematic review on the efficacy of oral ketamine in n = 1667 MDD patients indicated significant clinical improvement without serious adverse events, though limitations included a small number of RCTs and methodological bias (Meshkat et al. 2023). Moreover, two clinical studies reported increased hydroxynorketamine exposure after ketamine infusion was associated with poorer clinical response both short and long term in treatment-resistant depression (Farmer et al. 2020) and suicidal depression (Grunebaum et al. 2019), whilst a high-frequency EEG study reported positive correlations between maximum norketamine concentrations and antidepressant potential (Nottage et al. 2023). However, scepticism has remained regarding the bioavailability of oral ketamine which is perceived as an impediment to treatment. Though evidence is limited, the pharmacokinetic/pharmacodynamic profile of oral ketamine is shown to support oral dosing as a viable treatment option with high levels of metabolism and the more persistent action of the active metabolite norketamine, producing promising clinical outcomes with fewer adverse effects (Glue et al. 2021; Meshkat et al. 2023).
Additionally, ongoing concerns regarding ketamine’s abuse potential may be overstated, with little data presented in support of dependency liability and furthermore, evidence suggests interactions at opioid receptors are ‘opioid sparing’, potentially due to ketamine’s NMDA receptor effects, which may protect against tolerance (Swainson et al. 2022). However, contrarily, Williams et al. (2018) report that opioid pathways are integral to ketamine’s action, stating that 50 mg of naltrexone significantly blocked ketamine’s antidepressant effects, though others have suggested this work should be treated with caution, after a small study showed naltrexone 380 mg failed to attenuate ketamine’s antidepressant effects (Yoon et al. 2019) and earlier preclinical evidence suggests that ketamine isomers may be weak partial agonists at the mu opioid receptor (Hirota et al. 1999). Thus, the role of opiodergic and other mechanisms in the therapeutic and safety profile of ketamine is still to be fully investigated via sufficiently powered studies. Taken together, with demonstrated tolerability and safety, and comparable efficacy, low-dose oral ketamine shows some advantages over other routes, and therefore, any concerns about its clinical use should be reconsidered. However, judicious clinical prescribing is warranted, as with other well-established treatments such as stimulants or benzodiazepines with potential for misuse, risks and benefits should be considered together (Swainson et al. 2022).
Thus, the evidence presented here from psychiatric and pain research suggests that the pharmacological nature of orally administered racemic ketamine and the resulting high levels of norketamine may account for its reported therapeutic effects. That is, despite reports of low bioavailability and peak plasma concentrations, there is increasing evidence in clinical populations showing the considerable promise of oral ketamine. Indeed, though it is yet to be thoroughly and rigorously examined, early evidence suggests oral ketamine is worthy of larger scale investigations for mental health treatment uses, due to both improved tolerability and possible sustained treatment effects associated with the pharmacokinetics of the oral formulation. Our group reported 50% of trial participants with MDD and suicidality demonstrated a prolonged treatment response, 4 weeks after the final oral ketamine dose; however, this requires replication (Can et al. 2021). Thus, future studies are particularly required in long-term use, where oral ketamine may offer greater utility, to establish treatment protocols and examine the potential for adverse effects including neurotoxic effects, with some reports indicating the potential for an associated decline in cognition and memory (Liu et al. 2019; Driver et al. 2022) or addiction (Schak et al. 2016) in longer term use.
Based on the evidence to date, there is more work to be done regarding dosing and formulations. Further investigations into the optimal compounding formulas for oral preparations and treatment regimens are also of primary importance. Whilst the oral preparations are demonstrated to be efficacious with excellent general tolerability due to reduced psychotomimetic effects, the issue remains that absorption and bioavailability are highly variable. It could be argued that the extensive metabolism to norketamine is a desirable feature of oral administration, resulting in a therapeutic effect which is slower to develop but more sustained, due to the suspected, though yet to be fully investigated, activity of norketamine. Additionally, absorption may be improved by the addition of mucosal adhering agents to oral formulations. This addition may facilitate increased absorption, thus potentially contributing to a reduction in individual pharmacokinetic variability. Mucoadhesion is shown to improve absorption through prolongation of residence time in the gastrointestinal tract, resulting in improved bioavailability (Shaikh et al. 2011). This feature is of particular benefit to drug molecules that are not suited to oral dosing, including those that undergo extensive first-pass metabolism. Our group have utilised a mucosal adhering agent in the compounded oral solution, potentially contributing to treatment outcomes and this is an area which requires further investigation. Interestingly, a study on sublingual dosing observed a significant reduction (35–50%) in the Cmax and AUC when the sublingual product was held in the mouth and not swallowed with saliva, suggesting that ketamine administered sublingually is substantially absorbed in the gastrointestinal tract after swallowing (Yanagihara et al. 2003). Also requiring urgent attention is the development of recommended treatment guidelines for oral administration, as this route is likely to be favoured by mental health clinicians utilising ketamine in an off-label capacity, due to its ease of use and favourable safety profile. These often-solitary practitioners must be able to look to the literature for guidance in this regard and the current lack of consensus as demonstrated by reported treatment regimens of multiple times a day to monthly, in oral ketamine studies is problematic, particularly given the current interest in off-label use in psychiatry. A dosing regimen which provides optimal benefits with least side effects should be considered through individual patient risk/benefit analysis (Swainson et al. 2022). Current evidence demonstrates a dose response effect in antidepressant efficacy, with repeated dosing shown to produce a robust and longer lasting effect, preclinically and clinically (Zarate and Machado-Vieira 2017), though this needs to be confirmed in larger prospective studies. Given a single dose is reported to induce a treatment effect for up to 2 weeks (Krystal et al. 2019), weekly dosing may offer efficacy, with a reduced risk of adverse effects. However, the effect of age and sex is yet to be fully elucidated in clinical populations, though preclinical models indicate oestrogen receptor activity results in enhanced sensitivity to ketamine’s antidepressant effects and this may be mediated by oestradiol facilitation of transcriptional inductive expression of AMPA receptors (Ho et al. 2018). Additionally, clinically, women are shown to experience higher rates of MDD and sex-specific patterns of glutamate receptor gene expression may contribute to this (Gray et al. 2015), whilst oestrogen mediated sensitivity may also contribute to treatment response and this area also requires future exploration.
In conclusion, emerging evidence suggests oral ketamine is a viable mental health treatment option; however, further research is required to provide a greater pharmacological understanding of oral ketamine, to inform dosing regimens for effective treatment and patient safety. Considering the current lack of evidence and consensus regarding a dosing protocol for oral ketamine, individually titrated dosing, within a risk versus benefit framework, is likely to be necessary to maximise both clinical response and safety and tolerability.
References
Abdallah CG (2020) (2R,6R)-Hydroxynorketamine (HNK) plasma level predicts poor antidepressant response: is this the end of the HNK pipeline? Neuropsychopharmacology 45(8):1245–1246
Abdallah CG, Sanacora G, Duman RS, Krystal JH (2018) The neurobiology of depression, ketamine and rapid-acting antidepressants: is it glutamate inhibition or activation? Pharmacol Ther 190:148–158
Adamowicz P, Kala M (2005) Urinary excretion rates of ketamine and norketamine following therapeutic ketamine administration: method and detection window considerations. J Anal Toxicol 29(5):376–382
Al Shirawi MI, Kennedy SH, Ho KT, Byrne R, Downar J (2017) Oral ketamine in treatment-resistant depression: a clinical effectiveness case series. J Clin Psychopharmacol 37(4):464–467
Arabzadeh S, Hakkikazazi E, Shahmansouri N, Tafakhori A, Ghajar A, Jafarinia M, Akhondzadeh S (2018) Does oral administration of ketamine accelerate response to treatment in major depressive disorder? Results of a double-blind controlled trial. J Affect Disord 235:236–241
Bahji A, Vazquez GH, Zarate CA (2021) Comparative efficacy of racemic ketamine and esketamine for depression: a systematic review and meta-analysis. J Affect Disord 278:542–555
Ballard ED, Wills K, Lally N, Richards EM, Luckenbaugh DA, Walls T, Ameli R, Niciu MJ, Brutsche NE, Park L (2017) Anhedonia as a clinical correlate of suicidal thoughts in clinical ketamine trials. J Affect Disord 218:195–200
Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, Krystal JH (2000) Antidepressant effects of ketamine in depressed patients. Biol Psychiat 47(4):351–354
Blier P, Zigman D, Blier J (2012) On the safety and benefits of repeated intravenous injections of ketamine for depression. Biol Psychiatry 72(4):e11-12
Blonk MI, Koder BG, van den Bemt PMLA, Huygen FJPM (2010) Use of oral ketamine in chronic pain management: a review. Eur J Pain 14(5):466–472
Buvanendran A, Kroin JS, Rajagopal A, Robison SJ, Moric M, Tuman KJ (2018) Oral ketamine for acute pain management after amputation surgery. Pain Med 19(6):1265–1270
Can AT, Hermens DF, Dutton M, Gallay CC, Jensen E, Jones M, Scherman J, Beaudequin DA, Yang C, Schwenn PE, Lagopoulos J (2021) Low dose oral ketamine treatment in chronic suicidality: an open-label pilot study. Transl Psychiatry 11(1):101
Can AT, Hermens DF, Mohamed AZ, Shan ZY, Dutton M, Gallay C, Forsyth G, Jamieson D, Lagopoulos J (2023a) Treatment response with ketamine in chronic suicidality: an open label functional connectivity study. J Affect Disord 331:92–100
Can AT, Schwenn PE, Isbel B, Beaudequin D, Bouças AP, Dutton M, Jones M, Gallay CC, Forsyth G, Bennett MR, Lagopoulos J, Hermens DF (2023b) Electrophysiological phenotypes of suicidality predict prolonged response to oral ketamine treatment. Prog Neuropsychopharmacol Biol Psychiatry 123:110701
Chong CC, Schug SA, Page-Sharp M, Ilett KF (2006) Bioavailability of ketamine after oral or sublingual administration. Pain Med 7(5):469–469
Chu PSK, Ma WK, Wong SCW, Chu RWH, Cheng CH, Wong S, Tse Man-li J, Lau FL, Yiu MK, Man CW (2008) The destruction of the lower urinary tract by ketamine abuse: a new syndrome. BJU Int 102(11):1616–1622
Clements J, Nimmo W, Grant IS (1982) Bioavailability, pharmacokinetics, and analgesic activity of ketamine in humans. J Pharm Sci 71(5):539–542
Clements J, Nimmo WS (1981) “Pharmacokinetics and analgesic effect of ketamine in man” 53:1 27–30
Cvrcek P (2008) Side effects of ketamine in the long-term treatment of neuropathic pain. Pain Med 9(2):253–257
d’Andrea G, Pettorruso M, Lorenzo GD, Mancusi G, McIntyre RS, Martinotti G (2023) Rethinking ketamine and esketamine action: are they antidepressants with mood-stabilizing properties? Eur Neuropsychopharmacol 70:49–55
De Gioannis A, De Leo D (2014) Oral ketamine augmentation for chronic suicidality in treatment-resistant depression. Aust N Z J Psychiatry 48(7):686
Domany Y, Bleich-Cohen M, Tarrasch R, Meidan R, Litvak-Lazar O, Stoppleman N, Schreiber S, Bloch M, Hendler T, Sharon H (2019) Repeated oral ketamine for out-patient treatment of resistant depression: randomised, double-blind, placebo-controlled, proof-of-concept study. Br J Psychiatry 214(1):20–26
Driver C, Jackson TNW, Lagopoulos J, Hermens DF (2022) Molecular mechanisms underlying the N-methyl-d-aspartate receptor antagonists: highlighting their potential for transdiagnostic therapeutics. Prog Neuropsychopharmacol Biol Psychiatry 119:110609
Dutton M, Can AT, Lagopoulos J, Hermens DF (2022) Stress, mental disorder and ketamine as a novel, rapid acting treatment. Eur Neuropsychopharmacol 65:15–29
Ebert B, Mikkelsen S, Thorkildsen C, Borgbjerg FM (1997) Norketamine, the main metabolite of ketamine, is a non-competitive NMDA receptor antagonist in the rat cortex and spinal cord. Eur J Pharmacol 333(1):99–104
Enarson MC, Hays H, Woodroffe MA (1999) Clinical experience with oral ketamine. J Pain Symptom Manage 17(5):384–386
Farmer CA, Gilbert JR, Moaddel R, George J, Adeojo L, Lovett J, Nugent AC, Kadriu B, Yuan P, Gould TD, Park LT, Zarate CA Jr (2020) Ketamine metabolites, clinical response, and gamma power in a randomized, placebo-controlled, crossover trial for treatment-resistant major depression. Neuropsychopharmacology 45(8):1398–1404
Feder A, Parides MK, Murrough JW, Perez AM, Morgan JE, Saxena S, Kirkwood K, Aan Het Rot M, Lapidus KAB, Wan LB, Iosifescu D, Charney DS (2014) Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry 71(6):681–688
Fond G, Loundou A, Rabu C, Macgregor A, Lançon C, Brittner M, Micoulaud-Franchi JA, Richieri R, Courtet P, Abbar M, Roger M, Leboyer M, Boyer L (2014) Ketamine administration in depressive disorders: a systematic review and meta-analysis. Psychopharmacology 231(18):3663–3676
Freedman R, Brown AS, Cannon TD, Druss BG, Earls FJ, Escobar J, Hurd YL, Lewis DA, López-Jaramillo C, Luby J, Mayberg HS, Moffitt TE, Oquendo M, Perlis RH, Pine DS, Rush AJ, Tamminga CA, Tohen M, Vieta E, Wisner KL, Xin Y (2018) Can a framework be established for the safe use of ketamine? Am J Psychiatry 175(7):587–589
Gallay CC, Forsyth G, Can AT, Dutton M, Jamieson D, Jensen E, Hermens DF, Bennett MR, Lagopoulos J (2021) Six-week oral ketamine treatment for chronic suicidality is associated with increased grey matter volume. Psychiatry Res Neuroimaging 317:111369
Gilbert JR, Zarate CA Jr (2020) Electrophysiological biomarkers of antidepressant response to ketamine in treatment-resistant depression: gamma power and long-term potentiation. Pharmacol Biochem Behav 189:172856
Glue P, Medlicott NJ, Neehoff S, Surman P, Lam F, Hung N, Hung CT (2020) Safety and efficacy of extended release ketamine tablets in patients with treatment-resistant depression and anxiety: open label pilot study. Adv Psychopharmacol 10:2045125320922474
Glue P, Russell B, Medlicott NJ (2021) Influence of formulation and route of administration on ketamine’s safety and tolerability: systematic review. Eur J Clin Pharmacol 77(5):671–676
Grant IS, Nimmo WS, Clements JA (1981) Pharmacokinetics and analgesic effects of I.M. and oral ketamine. Br J Anaesth 53(8):805–810
Gray AL, Hyde TM, Deep-Soboslay A, Kleinman JE, Sodhi MS (2015) Sex differences in glutamate receptor gene expression in major depression and suicide. Mol Psychiatry 20(9):1057–1068
Grunebaum MF, Ellis SP, Keilp JG, Moitra VK, Cooper TB, Marver JE, Burke AK, Milak MS, Sublette ME, Oquendo MA, Mann JJ (2017) Ketamine versus midazolam in bipolar depression with suicidal thoughts: a pilot midazolam-controlled randomized clinical trial. Bipolar Disord 19(3):176–183
Grunebaum MF, Galfalvy HC, Choo TH, Keilp JG, Moitra VK, Parris MS, Marver JE, Burke AK, Milak MS, Sublette ME, Oquendo MA, Mann JJ (2018) Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. Am J Psychiatry 175(4):327–335
Grunebaum MF, Galfalvy HC, Choo TH, Parris MS, Burke AK, Suckow RF, Cooper TB, Mann JJ (2019) Ketamine metabolite pilot study in a suicidal depression trial. J Psychiatr Res 117:129–134
Grunebaum MF, Galfalvy HC, Liu J, Huang YY, Marcott S, Burke AK, Mann JJ (2020) Opioid receptor μ-1 and ketamine effects in a suicidal depression trial: a post hoc exploration. J Clin Psychopharmacol 40(4):420–422
Haas DA, Harper DG (1992) Ketamine: a review of its pharmacologic properties and use in ambulatory anesthesia. Anesth Prog 39(3):61
Hartberg J, Garrett-Walcott S, De Gioannis A (2018) Impact of oral ketamine augmentation on hospital admissions in treatment-resistant depression and PTSD: a retrospective study. Psychopharmacology 235(2):393–398
Henter ID, Park LT, Zarate CA (2021) Novel glutamatergic modulators for the treatment of mood disorders: current status. CNS Drugs 35(5):527–543
Hirota K, Okawa H, Appadu BL, Grandy DK, Devi LA, Lambert DG (1999) Stereoselective interaction of ketamine with recombinant [micro sign], [small kappa, Greek], and [small delta, Greek] opioid receptors expressed in Chinese Hamster ovary cells. Anesthesiology 90(1):174–182
Ho M-F, Correia C, Ingle JN, Kaddurah-Daouk R, Wang L, Kaufmann SH, Weinshilboum RM (2018) Ketamine and ketamine metabolites as novel estrogen receptor ligands: induction of cytochrome P450 and AMPA glutamate receptor gene expression. Biochem Pharmacol 152:279–292
Holtman JR Jr, Crooks PA, Johnson-Hardy JK, Hojomat M, Kleven M, Wala EP (2008) Effects of norketamine enantiomers in rodent models of persistent pain. Pharmacol Biochem Behav 90(4):676–685
Irwin SA, Iglewicz A, Nelesen RA, Lo JY, Carr CH, Romero SD, Lloyd LS (2013) Daily oral ketamine for the treatment of depression and anxiety in patients receiving hospice care: a 28-day open-label proof-of-concept trial. J Palliat Med 16(8):958–965
Jafarinia M, Afarideh M, Tafakhori A, Arbabi M, Ghajar A, Noorbala AA, Saravi MA, Agah E, Akhondzadeh S (2016) Efficacy and safety of oral ketamine versus diclofenac to alleviate mild to moderate depression in chronic pain patients: a double-blind, randomized, controlled trial. J Affect Disord 204:1–8
Kaur U, Pathak BK, Singh A, Chakrabarti SS (2021) Esketamine: a glimmer of hope in treatment-resistant depression. Eur Arch Psychiatry Clin Neurosci 271(3):417–429
Khorramzadeh E, Lofty AO (1973) The use of ketamine in psychiatry. Psychosomatics 14(6):344–346. https://doi.org/10.1016/S0033-3182(73)71306-2
Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD, Heninger GR, Bowers MB, Charney DS (1994) Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatr 51(3):199–214
Krystal JH, Abdallah CG, Sanacora G, Charney DS, Duman RS (2019) Ketamine: a paradigm shift for depression research and treatment. Neuron 101(5):774–778
Lara DR, Bisol LW, Munari LR (2013) Antidepressant, mood stabilizing and procognitive effects of very low dose sublingual ketamine in refractory unipolar and bipolar depression. Int J Neuropsychopharmacol 16(9):2111–2117
Lazarevic V, Yang Y, Flais I, Svenningsson P (2021) Ketamine decreases neuronally released glutamate via retrograde stimulation of presynaptic adenosine A1 receptors. Mol Psychiatry 26(12):7425–7435
Li Y, Jackson KA, Slon B, Hardy JR, Franco M, William L, Poon P, Coller JK, Hutchinson MR, Currow DC, Somogyi AA (2015) CYP2B6*6 allele and age substantially reduce steady-state ketamine clearance in chronic pain patients: impact on adverse effects. Br J Clin Pharmacol 80(2):276–284
Li Q et al (2017) Chronic Ketamine Exposure Causes White Matter Microstructural Abnormalities in Adolescent Cynomolgus Monkeys. Front Neurosci 11:285. https://doi.org/10.3389/fnins.2017.00285
Liu J et al (2019) The Role of NMDA Receptors in Alzheimer’s Disease. Front Neurosci 13:43. https://doi.org/10.3389/fnins.2019.00043
Loo CK, Gálvez V, O’Keefe E, Mitchell PB, Hadzi-Pavlovic D, Leyden J, Harper S, Somogyi AA, Lai R, Weickert CS (2016) Placebo-controlled pilot trial testing dose titration and intravenous, intramuscular and subcutaneous routes for ketamine in depression. Acta Psychiatr Scand 134(1):48–56
Marchetti F, Coutaux A, Bellanger A, Magneux C, Bourgeois P, Mion G (2015) Efficacy and safety of oral ketamine for the relief of intractable chronic pain: a retrospective 5-year study of 51 patients. Eur J Pain 19(7):984–993
Mason K, Cottrell AM, Corrigan AG, Gillatt DA, Mitchelmore AE (2010) Ketamine-associated lower urinary tract destruction: a new radiological challenge. Clin Radiol 65(10):795–800
Menniti FS, Lindsley CW, Conn PJ, Pandit J, Zagouras P, Volkmann RA (2013) Allosteric modulators for the treatment of schizophrenia: targeting glutamatergic networks. Curr Top Med Chem 13(1):26–54
Meshkat S et al (2023) Oral Ketamine for Depression: An Updated Systematic Review. World J Biol Psychiatry 24(7):545–557. https://doi.org/10.1080/15622975.2023.2169349
Mion G, Villevieille T (2013) Ketamine pharmacology: an update (Pharmacodynamics and Molecular Aspects, Recent Findings). CNS Neurosci Ther 19(6):370–380
Muetzelfeldt L, Kamboj SK, Rees H, Taylor J, Morgan CJA, Curran HV (2008) Journey through the K-hole: phenomenological aspects of ketamine use. Drug Alcohol Depend 95(3):219–229
Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Green CE, Perez AM, Iqbal S, Pillemer S, Foulkes A, Shah A, Charney DS, Mathew SJ (2013) Antidepressant efficacy of ketamine in treatment-resistant major depression: A two-site randomized controlled trial. Am J Psychiatry 170(10):1134–1142
Murrough JW, Soleimani L, Dewilde KE, Collins KA, Lapidus KA, Iacoviello BM, Lener M, Kautz M, Kim J, Stern JB, Price RB, Perez AM, Brallier JW, Rodriguez GJ, Goodman WK, Iosifescu DV, Charney DS (2015) Ketamine for rapid reduction of suicidal ideation: a randomized controlled trial. Psychol Med 45(16):3571–3580
Ng J, Lui LMW, Rosenblat JD, Teopiz KM, Lipsitz O, Cha DS, Xiong J, Nasri F, Lee Y, Kratiuk K, Rodrigues NB, Gill H, Subramaniapillai M, Mansur RB, Ho R, Cao B, McIntyre RS (2021) Ketamine-induced urological toxicity: potential mechanisms and translation for adults with mood disorders receiving ketamine treatment. Psychopharmacology 238(4):917–926
Nogo D, Nazal H, Song Y, Teopiz KM, Ho R, McIntyre RS, Lui LMW, Rosenblat JD (2022) A review of potential neuropathological changes associated with ketamine. Expert Opin Drug Saf 21(6):813–831
Nottage JF, Gabay A, De Meyer K, Herrik KF, Bastlund JF, Christensen SR, Gijsen S, Mehta MA (2023) The effect of ketamine and D-cycloserine on the high frequency resting EEG spectrum in humans. Psychopharmacology 240(1):59–75
Nowacka A, Borczyk M (2019) Ketamine applications beyond anesthesia - a literature review. Eur J Pharmacol 860:172547
Palucha-Poniewiera A (2018) The role of glutamatergic modulation in the mechanism of action of ketamine, a prototype rapid-acting antidepressant drug. Pharmacol Rep 70(5):837–846
Passie T, Adams H-A, Logemann F, Brandt SD, Wiese B, Karst M (2021) Comparative effects of (S)-ketamine and racemic (R/S)-ketamine on psychopathology, state of consciousness and neurocognitive performance in healthy volunteers. Eur Neuropsychopharmacol 44:92–104
Peltoniemi MA, Saari TI, Hagelberg NM, Laine K, Kurkinen KJ, Neuvonen PJ, Olkkola KT (2012) Rifampicin has a profound effect on the pharmacokinetics of oral S-ketamine and less on intravenous S-ketamine. Basic Clin Pharmacol Toxicol 111(5):325–332
Peltoniemi MA, Hagelberg NM, Olkkola KT, Saari TI (2016) Ketamine: a review of clinical pharmacokinetics and pharmacodynamics in anesthesia and pain therapy. Clin Pharmacokinet 55:1059–1077
Rolan P, Lim S, Sunderland V, Liu Y, Molnar V (2014) The absolute bioavailability of racemic ketamine from a novel sublingual formulation. Br J Clin Pharmacol 77(6):1011–1016
Romero-Sandoval EA (2011) Depression and pain: does ketamine improve the quality of life of patients in chronic pain by targeting their mood? Anesthesiology 115(4):687–688
Rosenblat JD, Carvalho AF, Li M, Lee Y, Subramanieapillai M, McIntyre RS (2019) Oral ketamine for depression: a systematic review. J Clin Psychiatr 80:3
Schak KM, Vande Voort JL, Johnson EK, Kung S, Leung JG, Rasmussen KG, Palmer BA, Frye MA (2016) Potential risks of poorly monitored ketamine use in depression treatment. Am J Psychiatry 173(3):215–218
Schmid RL, Sandler AN, Katz J (1999) Use and efficacy of low-dose ketamine in the management of acute postoperative pain: a review of current techniques and outcomes. Pain 82(2):111–125
Shaikh R, Raj Singh TR, Garland MJ, Woolfson AD, Donnelly RF (2011) Mucoadhesive drug delivery systems. J Pharm Bioallied Sci 3(1):89–100
Shimoyama M, Shimoyama N, Gorman AL, Elliott KJ, Inturrisi CE (1999) Oral ketamine is antinociceptive in the rat formalin test: role of the metabolite, norketamine. Pain 81(1–2):85–93
Singh JB, Fedgchin M, Daly EJ, De Boer P, Cooper K, Lim P, Pinter C, Murrough JW, Sanacora G, Shelton RC, Kurian B, Winokur A, Fava M, Manji H, Drevets WC, Van Nueten L (2016) A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. Am J Psychiatry 173(8):816–826
Sleigh J, Harvey M, Voss L, Denny B (2014) Ketamine – more mechanisms of action than just NMDA blockade. Trends Anaesth Crit Care 4(2):76–81
Sofia RD, Harakal JJ (1975) Evaluation of ketamine HCl for anti-depressant activity. Arch Int Pharmacodyn Ther 214(1):68–74
Soto E, Stewart DR, Mannes AJ, Ruppert SL, Baker K, Zlott D, Berger Handel D, AM, (2012) Oral ketamine in the palliative care setting: a review of the literature and case report of a patient with neurofibromatosis type 1 and glomus tumor-associated complex regional pain syndrome. Am J Hospice Palliat Med® 29(4):308–317
Swainson J, Klassen LJ, Brennan S, Chokka P, Katzman MA, Tanguay RL, Khullar A (2022) Non-parenteral ketamine for depression: a practical discussion on addiction potential and recommendations for judicious prescribing. CNS Drugs 36(3):239–251
Taylor JH, Landeros-Weisenberger A, Coughlin C, Mulqueen J, Johnson JA, Gabriel D, Reed MO, Jakubovski E, Bloch MH (2018) Ketamine for social anxiety disorder: a randomized, placebo-controlled crossover trial. Neuropsychopharmacology 43(2):325–333
Vickers BA, Lee W, Hunsberger J (2017) A case report: subanesthetic ketamine infusion for treatment of cancer-related pain produces urinary urge incontinence. A&a Practice 8(9):219–221
White PF, Way WL, Trevor AJ (1982) Ketamine—its pharmacology and therapeutic uses. J Am Soc Anesthesiologists 56(2):119–136
Williams NR, Heifets BD, Blasey C, Sudheimer K, Pannu J, Pankow H, Hawkins J, Birnbaum J, Lyons DM, Rodriguez CI, Schatzberg AF (2018) Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry 175(12):1205–1215
Wolff K, Winstock AR (2006) Ketamine: from medicine to misuse. CNS Drugs 20:199–218
Yanagihara Y, Ohtani M, Kariya S, Uchino K, Hiraishi T, Ashizawa N, Aoyama T, Yamamura Y, Yamada Y, Iga T (2003) Plasma concentration profiles of ketamine and norketamine after administration of various ketamine preparations to healthy Japanese volunteers. Biopharm Drug Dispos 24(1):37–43
Yang Y, Cui Y, Sang K, Dong Y, Ni Z, Ma S, Hu H (2018) Ketamine blocks bursting in the lateral habenula to rapidly relieve depression. Nature 554(7692):317–322
Yoon G, Petrakis IL, Krystal JH (2019) Association of combined naltrexone and ketamine with depressive symptoms in a case series of patients with depression and alcohol use disorder. JAMA Psychiat 76(3):337–338
Zanos P, Moaddel R, Morris PJ, Riggs LM, Highland JN, Georgiou P, Pereira EFR, Albuquerque EX, Thomas CJ, Zarate CA Jr, Gould TD (2018) Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev 70(3):621–660
Zarate CA (2022) Glutamate modulators and beyond: a neuroscience revolution in the making. Eur Neuropsychopharmacol: J Eur Coll Neuropsychopharmacol 54:72–74
Zarate CA, Machado-Vieira R (2017) Ketamine: translating mechanistic discoveries into the next generation of glutamate modulators for mood disorders. Mol Psychiatry 22(3):324–327
Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK (2006) A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 63(8):856–864
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
M.D.: conceptualisation, wrote first draft.
A.C.: review and editing of manuscript, resources
J.L.: conceptualisation, review and editing of the manuscript
D.H.: conceptualisation, review and editing of the manuscript
All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dutton, M., Can, A.T., Lagopoulos, J. et al. Oral ketamine may offer a solution to the ketamine conundrum. Psychopharmacology 240, 2483–2497 (2023). https://doi.org/10.1007/s00213-023-06480-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-023-06480-x