Abstract
Background
Sleep disturbances are common in smoking cessation attempts and are predictive of relapse. Despite this knowledge, there is no established animal model to study the effect of nicotine abstinence on sleep and EEG parameters.
Objectives
The present study was conducted to characterize sleep and wakefulness in male C57BL/6J mice during periods of oral nicotine administration and abstinence.
Methods
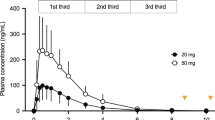
Male C57BL/6J mice were implanted with EEG/EMG recording devices. EEG/EMG data were recorded continuously for a period of 4 weeks. At the beginning of week 2, 200 μg/ml of nicotine was added to the 0.2% saccharin vehicle drinking solution. Following a 2-week period of oral nicotine administration, abstinence was initiated by excluding the nicotine from the 0.2% saccharin vehicle drinking solution. EEG/EMG were analyzed at pre-nicotine baseline, during nicotine administration, and on days 1, 2, and 5 of abstinence from nicotine.
Results
Oral nicotine administration decreased total sleep time during the active phase, consistent with the stimulant actions of nicotine. In contrast, NREM sleep quantity was increased during the active phase on nicotine abstinence day 1 and REM sleep was decreased during days 2 and 5 of abstinence. Further, sleep fragmentation was increased during the inactive phase on all days of abstinence. Oral nicotine administration and abstinence from nicotine also altered EEG relative power frequencies during the inactive and active phase.
Conclusions
Both oral nicotine administration and abstinence lead to sleep disturbances in mice. Similarities between this model and human reports on the effect of nicotine/nicotine withdrawal on sleep support its utility in examining the molecular mechanisms that modulate the relationship between sleep, nicotine, and nicotine abstinence/withdrawal.










Similar content being viewed by others
References
Aguirre CG, Madrid J, Leventhal AM (2015) Tobacco withdrawal symptoms mediate motivation to reinstate smoking during abstinence. J Abnorm Psychol 124(3):623–634. https://doi.org/10.1037/abn0000060
Baud MO, Magistretti PJ, Petit JM (2015) Sustained sleep fragmentation induces sleep homeostasis in mice. Sleep 38(4):567–579. https://doi.org/10.5665/sleep.4572
Bjorvatn B, Fagerland S, Ursin R (1998) EEG power densities (0.5–20 Hz) in different sleep-wake stages in rats. Physiol Behav 63:413–417. https://doi.org/10.1016/S0031-9384(97)00460-5
Brown RE, Basheer R, McKenna JT, Strecker RE, McCarley RW (2012) Control of sleep and wakefulness. Physiol Rev 92(3):1087–1187
Centers for Disease Control and Prevention (2011) Quitting smoking among adults – United States – 2001-2010. Morb Mortal Wkly Rep 60(44):1513–1519
Clasadonte J, McIver SR, Schmitt LI, Halassa MM, Haydon PG (2014) Chronic sleep restriction disrupts sleep homeostasis and behavioral sensitivity to alcohol by reducing the extracellular accumulation of adenosine. J Neurosci 34(5):1879–1891
Colrain IM, Trinder J, Swan GE (2004) The impact of smoking cessation on objective and subjective markers of sleep: review, synthesis, and recommendations. Nicotine Tob Res 9(6):913–925
Corwin EJ, Klein LC, Rickelman K (2002) Predictors of fatique in healthy young adults: moderating effects of cigarette smoking and gender. Biol Res Nurs 3(4):163–164
Crocq MA (2003) Alcohol, nicotine, caffeine, and mental disorders. Dialogues Clin Neurosci 5(2):175–185
Cummings KM, Giovino G, Jaén CR, Emrich LJ (1985) Reports of smoking withdrawal symptoms over a 21 day period of abstinence. Addict Behav 10(4):373–381
Domino et al (2009) Tobacco smoking produces widespread dominant brain wave alpha frequency increases. Int J Psychophysiol 74(3):192–198. https://doi.org/10.1016/j.ijpsycho.2009.08.011
Ernst M, Heishman SJ, Spurgeon L, London ED (2001) Smoking history and nicotine effects on cognitive performance. Neuropsychopharmacology 25(3):313–319
Foulds J, McSorley K, Sneddon J, Feyerabend C, Jarvis MJ, Russell MA (1994) Effect of subcutaneous nicotine injections on EEG alpha frequency in non-smokers: a placebo-controlled pilot study. Psychopharmacology 115(1–2):163–166
Foulds J, Stapleton J, Swettenham J, Bell N, McSorley K, Russell MAH (1996) Cognitive performance effects of subcutaneous nicotine in smokers and never-smoker. Pyschopharmacology 127:31–38
Grabus SD, Martin BR, Batman AM, Tyndale RF, Sellers E, Damaj MI (2005) Nicotine physical dependence and tolerance in the mouse following chronic oral administration. Psychpharmacology (Berl) 178(102):183–192
Grove JR, Wilkinson A, Dawson B, Eastwood P, Heard P (2006) Effects of exercise on aspects of sleep during tobacco withdrawal. Aust Psychol 41(1):69–76. https://doi.org/10.1080/00050060500395127
Hamidovic A, de Wit H (2009) Sleep deprivation increases cigarette smoking. Pharmacol Biochem Behav 93(3):263–269. https://doi.org/10.1016/j.pbb.2008.12.005.
Hatsukami D, Hughes JR, Pickens R (1985) Characterization of tobacco withdrawal: physiological and subjective effects. NIDA Res Monogr 53:56–67
Hatsukami DK, Dahlgren L, Zimmerman R, Hughes JR (1988) Symptoms of tobacco withdrawal from total cigarette cessation versus partial cigarette reduction. Psychopharmacology 94(2):242–247
Hughes JR (2007) Effects of abstinence from tobacco: valid symptoms and time course. Nicotine and Tobacco Research 9(3):315–327. https://doi.org/10.1080/14622200701188919
Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA (1986) Prevalence of smoking among psychiatric outpatients. Am J Psychiatr 143:993–997
Hughes JR, Higgins ST, Bickel WK (1994) Nicotine withdrawal versus other drug withdrawal syndromes: similarities and dissimilarities. Addiction 89(11):1461–1470
Institute of Medicine (US) Committee on Sleep Medicine and Research (2006) Sleep disorders and sleep deprivation: an unmet public health problem. National Academic Press, Washington (DC)
Jaehne A, Loessl B, Bárkai Z, Riemann D, Hornyak M (2009) Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Med Rev 13(5):363–377. https://doi.org/10.1016/j.smrv.2008.12.003
Jaehne A, Unbehaun T, Feige B, Cohrs S, Rodenbeck A, Riemann D (2015) Sleep changes in smokers before, during and 3 months after nicotine withdrawal. Addict Biol 20(4):747–755. https://doi.org/10.1111/adb.12151
Johnson RF, Beltz TG, Thunhorst RL, Johnson AK (2003) Investigations on the physiological controls of water and saline intake in C57BL/6 mice. Am J Phyiol Regul Integr Comp Physiol 285(2):394–403
Jorenby DE, Hatsukami DK, Smith SS, Fiore MC, Allen S, Jensen J, Baker TB (1996) Characterization of tobacco withdrawal symptoms: transdermal nicotine reduces hunger and weight gain. Psychopharmacology 128(2):130–138
Kim SC, Lee MH, Jang C, Kwon JW, Park JW (2013) The effect of alpha rhythm sleep on EEG activity and individuals’ attention. J Phys Ther Sci 25(12):15151518–15151518. https://doi.org/10.1589/jpts.25.1515
Knott VJ, Harr A, Ilivitsky V, Mahoney C (1998) The cholinergic basis of the smoking induced EEG activation profile. Neuropsyschobiology 38(2):97–107
Kumari V, Gray JA, ffytche DH, Mitterschiffthaler MT, Das M, Zachariah E, Vythelingum GN, Williams SCR, Simmons A, Sharma T (2003) Cognitive effects of nicotine in humans: an fMRI study. Neuroimage 19(3):1003–1013. https://doi.org/10.1016/S1053-8119(03)00110-1
Lena C, Popa D, Grailhe R, Escourrou P, Changeux JP, Adrien J (2004) Beta2 containing nicotinic receptors contribute to the organization of sleep and regulate putative micro-arousals in mice. J Neurosci 24:5711–5718
Malin DH, Goyarzu P (2009) Rodent models of nicotine withdrawal. In: Henningfield JE et al (eds) Nicotine psychopharmacology, handbook of experimental pharmacology. Springer-Verlag, Berlin, pp 401–434
McKenna et al (2008) Assessing sleepiness in the rat: a multiple sleep latencies test compared to polysomnographic measurers of sleepiness. J Sleep Res 17(4):365–375. https://doi.org/10.1111/j.13652869.2008.00686
Medic G, Wille M, Hemels MEH (2017) Short- and long-term health consequences of sleep disruption. Nat Sci Sleep 9:151–161. https://doi.org/10.2147/NSS.S134864
Okun ML, Levine MD, Patricia H, Perkins KA, Marcus MD (2011) Subjective sleep disturbance during a smoking cessation program: associations with relapse. Addict Behav 36(8):861–864. https://doi.org/10.1016/j.addbeh.2011.03.001
Parrott AC (1993) Cigarette smoking: effects upon self-rated stress and arousal over the day. Addict Behav 18(4):389–395
Patterson LM, Nutt DJ, Wilson SJ (2011) Sleep and its disorders in translational medicine. J Psychopharmacol 25(9):1226–1234. https://doi.org/10.1177/0269881111400643
Pietila K, Ahtee L (2000) Chronic nicotine administration in the drinking water affects the striatal dopamine in mice. Pharmacol Biochem Behav 66(1):95–103
Prosise GL, Bonnet MH, Berry RB, Dickel MJ (1994) Effects of abstinence from smoking on sleep and daytime sleepiness. Chest 105:1136–1141
Rechtschaffen A, Bergmann BM, Gilliand MA, Bouer K (1999) Effects of method, duration, and sleep stage on rebound from sleep deprivation in the rat. Sleep 22(1):11–31
Salin-Pascual RJ, Moro-Lopez ML, Gonzalez-Sanchez H, Blanco-Centurion C (1999) Changes in sleep after acute and repeated administration of nicotine in the rat. Psychopharmacology 145(2):133–138. https://doi.org/10.1007/s002130051041
Shiffman S, Paty JA, Gnys M, Kassel JD, Elash C (1995) Nicotine withdrawal in chippers and regular smokers: subjective and cognitive effects. Health Psychol 14(4):301–309
Shiffman S, Patten C, Gwaltney C, Paty J, Gnys M, Kassel J, Hickcox M, Waters A, Balabanis M (2006) Natural history of nicotine withdrawal. Addiction 101(12):1822–1832. https://doi.org/10.1111/j.1360-0443.2006.01635.x
Soldatos CR, Kales JD, Scharf MB, Bixler EO, Kales A (1980) Cigarette smoking associated with sleep difficulty. Science 207(4430):551–553
Sparks JA, Pauly JR (1999) Effects of continuous oral nicotine administration on brain nicotinic receptors and responsiveness to nicotine in C57Bl/6 mice. Psychopharmacology 141(2):145–153
Swan GE, Lessov-Schlaggar CN (2007) The effects of tobacco smoke on nicotine cognition and the brain. Neuropsychol Rev 17(3):259–273
Vyazovskiy VV, Tobler I (2005) Theta activity in the waking EEG is a marker of sleep propensity in the rat. Brain Res 1050(1–2):64–71
Weinberger AH, Platt J, Shuter J, Goodwin RD (2016) Gender Differences in self-reported withdrawal symptoms and reducing or quitting smoking three years later: A prospective, longitudinal examination of U.S. adults. Drug Alcohol Depend 165:253–259. https://doi.org/10.1016/j.drugalcdep.2016.06.013
Wesnes KA, Edgar CJ, Kezic I, Salih HM, de Boer P (2013) Effect of nicotine withdrawal on cognition in a clinical trial setting. Psychopharmacology 229(1):133–140. https://doi.org/10.1007/s00213-013-3089-6
Wetter DW, Fiore MC, Young TB, McClure JB, de Moor CA (1999) Gender differences in response to nicotine replacement therapy: objective and subjective indexes of tobacco withdrawal. Exp Clin Psychopharamacol 7(2):135–144. https://doi.org/10.1037/1064-1297.7.2.135
Zhang L, Samet J, Caffo B, Punjabi NM (2006) Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol 164(6):529–537
Zhang L, Samet J, Caffo B, Bankman I, Punjabi NM (2008) Power spectral analysis of EEG activity during sleep in cigarette smokers. Chest 133(2):427–432
Zhou X, Nonnemaker J, Sherrill B, Gilsenan AW, Coste F, West R (2009) Attempts to quit smoking and relapse: factors associated with success or failure from the ATTEMPT study. Addict Behav 34(4):365–373. https://doi.org/10.1016/j.addbeh.2008.11.013
Funding
Grant #: T32DA017637-12, National Institute on Drug Abuse.
Title: Research Training–Genetics of Substance Abuse.
PI: John K. Hewitt.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were approved by the University of Colorado’s Institutional Animal Care and Use Committee and followed the National Institutes of Health guide for the care and use of laboratory animals.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mathews, H.L., Stitzel, J.A. The effects of oral nicotine administration and abstinence on sleep in male C57BL/6J mice. Psychopharmacology 236, 1335–1347 (2019). https://doi.org/10.1007/s00213-018-5139-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-018-5139-6