Abstract
Rationale
The stress-induced hyperthermia (SIH) model is an anxiety model that uses the transient rise in body temperature in response to acute stress. Benzodiazepines produce anxiolytic as well as sedative side effects through nonselective binding to GABAA receptor subunits. The GABAA receptor α1 subunit is associated with sedation, whereas the GABAA receptor α2 and α3 subunits are involved in anxiolytic effects.
Objectives
We therefore examined the effects of (non)subunit-selective GABAA receptor agonists on temperature and locomotor responses to novel cage stress.
Results
Using telemetric monitoring of temperature and locomotor activity, we found that nonsubunit-selective GABAA receptor agonist diazepam as well as the α3 subunit-selective receptor agonist TP003 dose-dependently attenuated SIH and locomotor responses. Administration of GABAA receptor α1-selective agonist zolpidem resulted in profound hypothermia and locomotor sedation. The GABAA receptor α1-selective antagonist βCCt antagonized the hypothermia, but did not reverse the SIH response attenuation caused by diazepam and zolpidem. These results suggest an important regulating role for the α1 subunit in thermoregulation and sedation. Ligands of extrasynaptic GABAA receptors such as alcohol and nonbenzodiazepine THIP attenuated the SIH response only at high doses.
Conclusions
The present study confirms a putative role for the GABAA receptor α1 subunit in hypothermia and sedation and supports a role for α2/3 subunit GABAA receptor agonists in anxiety processes. In conclusion, we show that home cage temperature and locomotor responses to novel home cage stress provide an excellent tool to assess both anxiolytic and sedative effects of various (subunit-selective) GABAAergic compounds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The involvement of the GABAA receptor in anxiety has been extensively studied and confirmed (Nemeroff 2003). The pentameric GABAA receptor consists of five subunits (α1–6, β1–3, γ1–3, δ, ɛ, θ, and π), and the assembly of different combinations of subunits allows the construction of different types of GABAA receptors, each having specific functional and pharmacological properties (Korpi et al. 2002). The majority of GABAA receptors are composed of two α subunits, two β subunits, and one γ subunit (Tretter et al. 1997). Classical benzodiazepines bind to GABAA receptors containing α1, α2, α3, and/or α5 subunits, while binding affinity to α4-containing and α6-containing subunits is extremely weak (Rudolph and Mohler 2004). Besides the preferred anxiolytic action, the use of benzodiazepines is associated with dependence, anticonvulsant activity, sedation, amnesia, and daytime drowsiness (Stewart and Westra 2002). These different benzodiazepine effects are thought to be mediated through different GABAA receptor subtypes. Therefore, the search for new anxiolytics focuses on subunit-selective GABAA receptor agonists. Both genetic and pharmacological studies suggest a major role of the α2 and the α3 GABAA receptor subunit in mediating anxiolysis (Atack et al. 2005; Dias et al. 2005; Low et al. 2000; Rudolph and Mohler 2004). Consistent with this role, the α2 and the α3 GABAA receptor subunits are expressed in anxiety-involved areas like the amygdala and bed nucleus of the stria terminalis (Pirker et al. 2000). The GABAA receptor α1 subunit is associated with sedative and amnesic effects, while it is not involved in anxiolysis (McKernan et al. 2000; Rowlett et al. 2005; Rudolph et al. 1999). Compounds lacking activity at the α1-containing GABAA receptor while still modulating the α2 and/or α3 GABAA receptor subunit appear to be prime candidates for nonsedating anxiolytic drugs (de Haas et al. 2007; Huang et al. 2000). The research for novel anxiolytics has focused on compounds with selective efficacy at different subunits (while binding to all subunits) rather than compounds with different affinities for the subunits (Atack 2005). We therefore aimed to characterize the effects of different GABAA ligands on temperature and locomotor responses to novel cage stress in rats, using home cage telemetry, in order to deduce the relative contributions of α subunits of the GABAA receptor. Somatic stress symptoms are mediated by the autonomic nervous system and constitute a functional response in both humans and animals. The stress-induced hyperthermia (SIH) paradigm uses the physiological transient rise in body temperature in response to stress as a new and translational alternative in anxiety research (Bouwknecht et al. 2007; Vinkers et al. 2008). Using this paradigm, anxiolytic drugs including most benzodiazepines have been shown to dose-dependently attenuate the SIH response (Bouwknecht et al. 2007; Olivier et al. 2002; Van Bogaert et al. 2006). Using telemetry, stress-induced home cage temperature and locomotor activity responses can be simultaneously recorded, thus facilitating the comparison of effects on body temperature and locomotor activity caused by various GABAergic drugs. We hypothesized that anxiolytic effects would cause the SIH response to decrease without influencing basal body temperature and stress-induced locomotor activity responses. GABAergic sedative effects on the other hand would be characterized by a decrease in locomotor activity as well as general hypothermic state.
In the present study, we investigated the nonsubunit-selective GABAA receptor agonist diazepam (Pritchett et al. 1989), the intermediate selective α1 subunit GABAA receptor agonist zolpidem, as well as the selective α3 subunit GABAA receptor agonist TP003 (Dias et al. 2005). Zolpidem is approximately fivefold to tenfold more selective for α1 subunit-containing GABAA receptors than α2 and α3 subunit-containing receptors (Ebert et al. 2006; Petroski et al. 2006). However, zolpidem may demonstrate less selectivity in vivo compared to studies using recombinant receptors (Atack et al. 1999). TP003 has lower efficacies at the different α subtypes with less than 15% potentiation at the α2 and α5 subunit compared to diazepam (Dias et al. 2005). Exposure to higher drug doses may lead to loss of selectivity. We combined these compounds with the selective α1 subunit GABAA receptor antagonist beta-carboline-carboxy-tert-butyl ester (βCCt; Huang et al. 1999).
Less abundant populations of a δ subunit-containing GABAA receptors are often located extrasynaptically and perisynaptically and are thought to be involved in a continuous active inhibitory tone instead of the phasic inhibitory tone caused by intrasynaptic agonists (Jia et al. 2005; Nusser et al. 1998). Alcohol is anxiolytic at low doses and has been shown to bind to extrasynaptic GABAA receptors containing α4 or α6 and δ subunits (Wallner et al. 2003). However, at higher doses, ethanol can modulate excitatory N-methyl-d-aspartic acid (NMDA) and non-NMDA glutamate receptors, serotonin and glycine receptors, as well as potassium and calcium channels (Crews et al. 1996; Davies 2003; Harris 1999). Also, the fact that δ-deficient mice demonstrated a normal anxiolytic and hypothermic response to ethanol and that the alcohol sensitivity of α4β3δ GABAA receptors could not be replicated (Borghese et al. 2006) indicates that the discussion on the mechanism by which ethanol activates the GABAA receptor is still ongoing (Mihalek et al. 2001). Generally, the sedative and anxiolytic effects of alcohol were not altered after deletion of the α1 subunit, suggesting that other yet unexplained factors may play a role (Kralic et al. 2003). Moreover, we studied the nonbenzodiazepine hypnotic drug THIP (gaboxadol) that also binds to extrasynaptic GABAA receptor δ subunits with putative anxiolytic effects (Elfline et al. 2004; Wafford and Ebert 2006).
Materials and methods
Animals
Male Wistar rats (Harlan Zeist, The Netherlands) were used in the current study. Rats were housed socially in a controlled environment with a nonreversed 12 h light/dark cycle (white lights on from 7 am to 7 pm). Animals had unlimited access to food (standard laboratory chow) and water. One week after arrival, telemetry transmitters were implanted. After recovery from surgery, rats were housed in groups of four in type IV Macrolon® cages with a plastic tube as cage enrichment. Food (standard laboratory chow) and tap water were available ad libitum. Once a week, an experimental procedure was carried out. All experiments were carried out with the approval of the ethical committee on animal experiments of the Faculties of Sciences, Utrecht University, The Netherlands, and in accordance with the Declaration of Helsinki.
Surgery
A telemetric device (type ETA-F20, Data Sciences International, St. Paul, MN, USA) was implanted in the abdominal cavity as described earlier (Pattij et al. 2001). Prior to surgery, rats received a subcutaneous (s.c.) injection (2 mL/kg) of the antibiotic Baytrill® (2.5% enrofloxacin). Rats were anesthetized using O2/NO2/isoflurane gas anesthesia. Carprofen (5 mg/kg, s.c.) was given as an analgesic immediately after surgery and twice daily for 2 days after surgery. After surgery, animals were housed individually for 1 week and recovery from surgery was monitored (weight, heart rate, temperature). Also, all rats had access to wet food and solid drinks (gel formula as a water replacement) for 2 days after surgery. Wound recovery was regularly checked. One animal repeatedly opened the abdomen wound and, therefore, had to be sacrificed and replaced. During the experiments, one rat was removed from the experiments due to an inflammation surrounding the telemetry device.
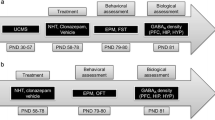
Experimental procedure
On the afternoon before an experimental day, rats were weighed and housed individually in a type III Macrolon® cage, located on a telemetric receiver. The telemetric transmitters were activated using a magnet. Data collection was subsequently started. The day after, the SIH procedure was initiated, consisting of an injection (intraperitoneal [i.p.] or oral [p.o.]) with vehicle or a certain drug dose. Immediately after injection, rats were placed back into their individual cage. Rats were placed in a novel cage (clean cage with fresh bedding and a paper tissue) 60 min later and left undisturbed for approximately 2 h afterwards. At the end of the experimental day, rats were group-housed again and transmitters were turned off. To prevent habituation to the novel cage procedure, the interval between two experiments was set to be at least 1 week. A within-subject design was used, and all animals received all (combined) doses of the drugs.
Drugs
Diazepam, zolpidem, alcohol, and THIP HCl (gaboxadol) were obtained from Sigma Aldrich. βCCt was synthesized by the laboratory of Dr. J. M. Cook, University of Wisconsin-Milwaukee. TP003 was synthesized according to published methods (Dias et al. 2005; Goodacre et al. 2003; Humphries et al. 2006). An injection volume of 2 mL/kg was used for intraperitoneal injections of all drugs, except THIP HCl (5 mL/kg, i.p.) and alcohol (5 mL/kg p.o.). Diazepam, zolpidem, βCCt, TP003, and gaboxadol were suspended in gelatin–mannitol 0.5%/5%. When βCCt was combined with diazepam or zolpidem, βCCt at a dose of 10 mg/kg was injected 10 min prior to diazepam/zolpidem injection. Fresh solutions and suspensions were prepared each testing day.
Data analysis
All data were collected in 5-min blocks and are displayed ±SEM. All experiments were carried out with a within-subject design. Body temperature and locomotor activity were analyzed during the first hour after novel cage using a univariate repeated-measures analysis of variance (ANOVA) with manipulations time and treatment as within-subject factors. Simple contrast tests were used to compare drug with vehicle conditions whenever a significant main effect for drug (indicating an effect on the basal body temperature) or a significant drug × time interaction effect (indicating an effect on the SIH response) was observed. Also, the SIH response was calculated from the telemetry data for each individual rat by subtracting the body temperature at t = 0 from the maximum temperature reached within the first 30 min after the novel cage procedure and compared using a repeated-measures ANOVA with drug as within-subject factor and simple contrasts to compare drug with vehicle conditions. In addition, cumulative locomotor activity after the first 60 min after injection and cumulative locomotor activity after the first 60 min after the novel cage procedure were calculated and compared using repeated-measures ANOVA. A probability level of p < 0.05 was set as statistically significant; probability levels between p = 0.05 and p = 0.1 were regarded as trends.
Results
Diazepam
Summary
Diazepam dose-dependently attenuated the SIH response to novel cage stress without affecting basal body temperature and reduced locomotor activity levels before and after the novel cage procedure only at higher doses (Fig. 1a, c; n = 11).
The effects of diazepam with and without βCCt on the novel cage-induced temperature and locomotor responses (t = −60 injection, t = 0 novel cage stress). *p < 0.05; **p < 0.01; ***p < 0.001. Inset calculated SIH response from the telemetry data. a Diazepam (0–4 mg/kg) dose-dependently reduced the SIH response. Inset calculated SIH response from the telemetry data. b Diazepam at a dose of 4 mg/kg reduced core body temperature and the SIH response. Prior injection with βCCt (10 mg/kg) prevented basal core body temperature reduction without affecting the diazepam-induced reduction of the SIH response *p < 0.05, diazepam effect and diazepam × βCCt interaction. Inset calculated SIH response from the telemetry data. c Diazepam (4 mg/kg) reduced stress-induced locomotor activity responses [Inset white bar cumulative locomotor activity t = −60 to t = 0 (after injection), gray bar cumulative locomotor activity t = 0 to t = 60 (after novel cage)]. d Diazepam (4 mg/kg) reduced stress-induced locomotor activity responses with no effect of βCCt [Inset white bar cumulative locomotor activity t = −60 to t = 0 (after injection), gray bar cumulative locomotor activity t = 0 to t = 60 (after novel cage)]. e βCCt (0–20 mg/kg) did not affect SIH responses Inset calculated SIH response from the telemetry data
Body temperature
The novel cage SIH response (F(12,120) = 22.0, p < 0.001) was reduced by diazepam (diazepam × time interaction: F(36,360) = 4.31, p < 0.001). Diazepam did not influence basal body temperature (diazepam effect: F(3,30) = 1.04, p = 0.39, NS) (Fig. 1a). The calculated SIH response revealed a diazepam effect on the SIH response (F(3,30) = 12.74, p < 0.001). Simple contrasts revealed SIH attenuation at higher doses (1 mg/kg–vehicle: F(1,10) = 3.85, p = 0.08, trend; 2 mg/kg–vehicle: F(1,10) = 6.03, p < 0.05; 4 mg/kg–vehicle: F(1,10) = 33.51, p < 0.001) (Fig. 1a, inset).
Locomotor activity
The novel cage stress-induced locomotor activity response (F(12,120) = 20.55, p < 0.001) was overall diminished by diazepam (diazepam effect: F(3,30) = 4.98, p < 0.01), although not dependent upon time (diazepam × time interaction: F(3,30) = 1.33, p = 0.11, NS). Only the higher doses of diazepam influenced locomotor activity [planned comparisons: vehicle–1 mg/kg (F(1,10) = 1.68, p = 0.22, NS), vehicle–2 mg/kg (F(1,10) = 8.18, p < 0.05), and vehicle–4 mg/kg (F(1,10) = 7.03, p < 0.05)]. When cumulating locomotor activity levels after injection and after stress (Fig. 1c, inset), diazepam reduced locomotor activity levels at higher doses (main diazepam effect: F(3,30) = 3.03, p < 0.05; simple contrasts: 2 mg/kg vs vehicle F(1,10) = 3.85, p = 0.08, NS; 4 mg/kg vs vehicle F(1,10) = 5.19, p < 0.05). Activity levels were larger after the novel cage procedure than after injection stress (stress effect: F(1,10) = 8.55, p < 0.05).
βCCt
Body temperature
βCCt alone did not affect the SIH response (time effect: F(12,120) = 53.00, p < 0.001; βCCt effect: F(3,30) = 0.70, p = 0.56, NS; βCCt × time interaction: F(36,360) = 1.17, p = 0.24, NS) (Fig. 1e; n = 11).
The calculated SIH response revealed no βCCt effect on the SIH response (F(3,30) = 0.33, p = 0.80, NS). Simple contrasts revealed that there was no attenuation of the SIH response at any dose (3 mg/kg–vehicle: F(1,10) = 0.06, p = 0.83, NS; 10 mg/kg–vehicle: F(1,10) = 0.29, p = 0.61, NS; 20 mg/kg–vehicle: F(1,10) = 0.13, p = 0.72, NS) (Fig. 1e, inset).
Locomotor activity
βCCt did not influence the stress-induced locomotor activity responses (time effect: F(12,120) = 13.72, p < 0.001; βCCt effect: F(3,30) = 0.23, p = 0.88, NS; βCCt × time interaction: F(36,360) = 1.02, p = 0.45, NS) (data not shown).
Diazepam and βCCt
Summary
βCCt was able to partially reverse the diazepam-induced hypothermia without affecting diazepam’s ability to reduce the SIH response. βCCt was not able to reverse the diazepam-induced locomotor reduction (Fig. 1b, d; n = 8).
Body temperature
When combined with βCCt, the SIH response (time effect: F(12,84) = 9.85, p < 0.001) was overall reduced by diazepam (diazepam × time interaction: F(12,84) = 5.17, p < 0.001). βCCt did not influence the SIH response (βCCt × time interaction: F(12,84) = 1.38, p = 0.19, NS). Diazepam reduced basal body temperature (diazepam effect: F(1,7) = 6.96, p < 0.05) and βCCt influenced the diazepam-induced hypothermia (diazepam × βCCt interaction: F(1,7) = 6.18, p < 0.05) without altering the body temperature itself (βCCt effect: F(1,7) = 1.24, p = 0.30, NS). The calculated SIH response revealed that diazepam reduced the SIH response (diazepam effect: F(1,7) = 16.94, p < 0.01). βCCt itself did not affect the SIH response (βCCt effect: F(1,7) = 1.86, p = 0.22, NS) nor did βCCt affect the attenuation of the SIH response by diazepam (diazepam × βCCt interaction: F(1,7) = 0.68, p = 0.44, NS) (Fig. 1b, inset).
Locomotor activity
When diazepam was injected after βCCt, the stress-induced locomotor activity response (time effect: F(12,84) = 7.65, p < 0.001) was generally and time-dependently reduced by diazepam (diazepam effect: F(1,7) = 9.48, p < 0.05; diazepam × time interaction: F(12,84) = 3.45, p < 0.001) with no effect of βCCt (βCCt effect: F(1,7) = 0.20, p = 0.68, NS; βCCt × time interaction: F(12,84) = 0.32, p = 98, NS; βCCt × diazepam interaction: F(1,7) = 0.02, p = 0.88, NS). When cumulating locomotor activity levels after injection and after stress (Fig. 1d, inset), diazepam generally reduced locomotor activity levels (main diazepam effect: F(1,7) = 10.86, p = 0.01; stress effect: F(1,7) = 2.47, p = 0.16, NS) without effect of βCCt (βCCt effect: F(1,7) = 0.05, p = 0.82, NS; βCCt × diazepam interaction: F(1,7) = 0.21, p = 0.66, NS).
Zolpidem
Summary
Zolpidem dose-dependently reduced basal body temperature and the SIH response and attenuated stress-induced and basal locomotor activity levels (Fig. 2a, c; n = 12).
The effects of zolpidem with and without βCCt on the novel cage-induced temperature and locomotor responses (t = −60 injection, t = 0 novel cage stress). *p < 0.05; **p < 0.01; ***p < 0.001. a Zolpidem (0–30 mg/kg) dose-dependently reduced the SIH response and basal body temperature. Inset calculated SIH response from the telemetry data. b Zolpidem at a dose of 10 mg/kg reduced core body temperature and the SIH response. Prior injection with βCCt (10 mg/kg) reversed basal core body temperature reduction without affecting the zolpidem-induced reduction of the SIH response. **p < 0.01, zolpidem effect; *p < 0.05, zolpidem × βCCt interaction. Inset calculated SIH response from the telemetry data. c Zolpidem (0–30 mg/kg) dose-dependently reduced stress-induced locomotor activity responses. Inset: white bar cumulative locomotor activity t = −60 to t = 0 (after injection), gray bar cumulative locomotor activity t = 0 to t = 60 (after novel cage). d Zolpidem (10 mg/kg) reduced stress-induced locomotor activity responses. βCCt partially reversed zolpidem-induced locomotor sedation. *p < 0.05, zolpidem × βCCt interaction. Inset: white bar cumulative locomotor activity t = −60 to t = 0 (after injection), gray bar cumulative locomotor activity t = 0 to t = 60 (after novel cage)
Body temperature
Zolpidem reduced basal body temperature (main zolpidem effect: F(3,33) = 9.85, p < 0.001). Basal body temperature was found to be reduced in all three dosages [planned comparisons: vehicle–3 mg/kg (F(1,11) = 8.89, p < 0.05), vehicle–10 mg/kg (F(1,11) = 27.98, p < 0.001), and vehicle–30 mg/kg (F(1,11) = 26.73, p < 0.001)]. The SIH response (time effect: F(12,132) = 15.70, p < 0.001) was reduced by zolpidem (zolpidem × time interaction: F(36,396) = 10.12, p < 0.001). The calculated SIH response revealed that zolpidem reduced the SIH response (F(3,33) = 12.71, p < 0.001). Simple contrasts revealed SIH attenuation at all doses (3 mg/kg–vehicle: F(1,11) = 18.17, p < 0.001; 10 mg/kg–vehicle: F(1,11) = 100.61, p < 0.001; 30 mg/kg–vehicle: F(1,11) = 24.10, p < 0.001) (Fig. 2a, inset).
Locomotor activity
The stress-induced locomotor response (main time effect: F(12,132) = 12.48, p < 0.001) was reduced by zolpidem (main zolpidem effect: F(3,33) = 7.41, p < 0.001; zolpidem × time interaction: F(36,396) = 1.98, p < 0.001). Locomotor activity was found to be reduced in all three dosages [planned comparisons: vehicle–3 mg/kg (F(1,11) = 8.27, p < 0.05), vehicle–10 mg/kg (F(1,11) = 12.25, p < 0.01), and vehicle–30 mg/kg (F(1,11) = 13.34, p < 0.01)]. When cumulating locomotor activity levels after injection and after novel cage stress (Fig. 2c, inset), zolpidem was found to reduce overall locomotor activity (main zolpidem effect: F(3,33) = 12.21, p < 0.001; zolpidem × stress interaction: F(3,33) = 0.31, p = 0.69, NS). Simple contrasts showed that all doses of zolpidem reduced cumulative locomotor activity (vehicle–3 mg/kg: F(1,11) = 12.28, p < 0.01; vehicle–10 mg/kg: F(1,11) = 12.37, p < 0.01; vehicle–30 mg/kg: F(1,11) = 25.11, p < 0.001). Novel cage-induced locomotor levels were larger than injection-induced locomotor levels (stress effect: F(3,33) = 17.18, p < 0.01).
Zolpidem and βCCt
Summary
βCCt was able to partially reverse the overall zolpidem-induced hypothermia as well as time-dependently partially reverse the zolpidem-induced locomotor sedation (Fig. 2b, d; n = 8).
Body temperature
When combined with βCCt, zolpidem did not significantly reduce the SIH response (main time effect: F(12,84) = 9.75, p < 0.001; zolpidem × time interaction: F(12,84) = 0.93, p = 0.54, NS). Also, βCCt did not influence the SIH response (βCCt × time interaction: F(12,84) = 0.92, p = 0.53, NS). Zolpidem reduced basal body temperature (main zolpidem effect: F(1,7) = 11.12, p < 0.01), and βCCt influenced the zolpidem-induced hypothermia (zolpidem × βCCt interaction: F(1,7) = 6.31, p < 0.05) without altering the body temperature itself (βCCt effect: F(1,7) = 2.54, p = 0.16, NS). The calculated SIH response revealed that zolpidem reduced the SIH response (diazepam effect: F(1,7) = 11.31, p = 0.01). βCCt itself did not affect the SIH response (βCCt effect: F(1,7) = 0.01, p = 0.97, NS) nor did βCCt affect the attenuation of the SIH response by zolpidem (zolpidem × βCCt interaction: F(1,7) = 0.25, p = 0.63, NS) (Fig. 2b, inset).
Locomotor activity
When combined with βCCt, zolpidem overall reduced locomotor responses (main zolpidem effect: F(1,7) = 7.80, p < 0.05; zolpidem × time interaction: F(1,7) = 1.99, p < 0.05). βCCt had no overall effect on locomotor responses (βCCt effect: F(1,7) = 1.94, p = 0.21, NS). However, βCCt reversed locomotor activity in the zolpidem group dependent upon time (zolpidem × βCCt × time interaction: F(12,84) = 1.91, p < 0.05; zolpidem × βCCt interaction: F(1,7) = 0.18, p = 0.69, NS). When cumulating locomotor activity levels after injection and after novel cage stress (Fig. 2d, inset), zolpidem reduced basal and stress-induced locomotor activity (zolpidem effect: F(1,7) = 16.73, p < 0.01; stress effect: F(1,7) = 1.61, p = 0.25, NS) without overall effect of βCCt (βCCt effect: F(1,7) = 2.09, p = 0.19, NS; βCCt × zolpidem interaction: F(1,7) = 1.47, p = 0.26, NS).
TP003
Summary
TP003 reduced the SIH response at higher doses as well as reduced basal body temperature and attenuated novel cage-induced activity more than injection-induced activity (Fig. 3a, b; n = 10).
The effects of TP003 (0–3 mg/kg, a and b), alcohol (0–3 g/kg, c and d), and THIP (0–10 mg/kg, e and f) on the novel cage-induced temperature and locomotor responses (t = −60 injection, t = 0 novel cage stress). *p < 0.05; **p < 0.01; ***p < 0.001. a TP003 reduced the SIH response at higher doses. Inset: calculated SIH response from the telemetry data. b TP003 dose-dependently reduced stress-induced locomotor activity responses (***). Inset graphs: white bar cumulative locomotor activity t = −60 to t = 0 (after injection stress), gray bar cumulative locomotor activity t = 0 to t = 60 (after novel cage stress). [TP003 reduced overall locomotor activity (TP003 effect: *p < 0.001), but more so after the novel cage procedure (TP003 × stress effect, *p < 0.001)]. c Alcohol at the highest dose reduced the SIH response (***) and basal body temperature (**). Inset calculated SIH response from the telemetry data. d Alcohol did not affect stress-induced locomotor activity responses. Inset graphs: white bar cumulative locomotor activity t = −60 to t = 0 (after injection stress), gray bar cumulative locomotor activity t = 0 to t = 60 (after novel cage stress). e THIP at the highest dose reduced the SIH response (***) and basal body temperature (**). Inset: calculated SIH response the telemetry data. f THIP at the highest dose reduced stress-induced locomotor activity responses. Inset THIP did not reduce overall locomotor activity, but did reduce locomotor activity after the novel cage procedure (gaboxadol × stress effect, ***p < 0.05)
Body temperature
The SIH response (main time effect: F(12,108) = 19.27, p < 0.001) was attenuated by TP003 (TP003 × time interaction: F(36,324) = 1.93, p < 0.01). TP003 did influence basal core body temperature (F(3,27) = 2.96, p = 0.050). Planned comparisons revealed a significant difference between the vehicle and 1 mg/kg condition (F(1,9) = 6.26, p < 0.05), a trend for a difference between vehicle and 3 mg/kg condition (F(1,9) = 3.65, p = 0.09, NS), and no difference between vehicle and 0.3 mg/kg condition (F(1,9) = 0.27, p = 0.62,NS). The calculated SIH response revealed TP003 reduced the SIH response (F(3,27) = 12.57, p < 0.001). Simple contrasts revealed SIH attenuation at all doses (0.3 mg/kg–vehicle: F(1,9) = 22.25, p < 0.001; 1 mg/kg–vehicle: F(1,9) = 25.50, p < 0.001; 3 mg/kg–vehicle: F(1,9) = 27.79, p < 0.001) (Fig. 3a, inset).
Locomotor activity
Stress-induced locomotor responses (main time effect: F(12,108) = 22.43, p < 0.001) were reduced by TP003 (TP003 effect: F(3,27) = 14.43, p < 0.001; TP003 × time interaction: F(36,324) = 1.42, p = 0.06). All three TP003 doses resulted in significant activity reduction after novel cage stress compared to the vehicle group (F(1,9) = 23.94, p < 0.001 for vehicle–0.3 mg/kg, F(1,9) = 25.56, p < 0.001 for vehicle–1 mg/kg, and F(1,9) = 14.09, p < 0.01 for vehicle–3 mg/kg, simple contrasts). When cumulating locomotor activity levels after injection and after novel cage stress (Fig. 3b, inset), TP003 reduced locomotor activity levels after novel cage stress more than after injection (TP003 effect: F(3,27) = 9.34, p < 0.001; TP003 × pre–post interaction: F(1,9) = 9.81, p < 0.001), Although activity levels were comparable after both injection and novel cage (stress effect: F(1,9) = 1.63, p = 0.23, NS).
Alcohol
Summary
Alcohol reduced the SIH response and basal body temperature only at higher doses. Alcohol did not affect locomotor activity levels after injection and after novel cage stress (Fig. 3c, d; n = 11).
Body temperature
Novel cage stress led to a significant increase in temperature (time effect: F(12,120) = 15.68, p < 0.001) and alcohol reduced the SIH response (time × alcohol interaction: F(36,360) = 2.56, p < 0.001). Alcohol decreased basal body temperature (main alcohol effect: F(3,30) = 4.82, p < 0.01). Simple contrasts revealed differences only between vehicle and 3 g/kg regarding basal body temperature (dose contrasts: vehicle–0.3 g/kg: F(1,10) = 0.79, NS; vehicle–1 g/kg: F(1,10) = 0.01, p = 0.98, NS; vehicle–3 g/kg: F(1,10) = 5.71, p < 0.05). The calculated SIH response showed a trend for alcohol to reduce the SIH response (F(3,30) = 2.30, p = 0.09, NS). Simple contrasts revealed SIH attenuation at higher doses (1 g/kg–vehicle: F(1,10) = 1.32, p = 0.28, NS; 2 g/kg–vehicle: F(1,10) = 5.19, p < 0.05; 4 g/kg–vehicle: F(1,10) = 5.12, p < 0.05) (Fig. 3c, inset).
Locomotor activity
The locomotor reaction in response to novel cage stress (time effect: F(12,120) = 16.87, p < 0.001) was not affected by alcohol (main alcohol effect: F(3,30) = 0.62, p = 0.61, NS; alcohol × time interaction: F(36,360) = 1.23, p = 0.18, NS). When cumulating locomotor activity levels after injection and after novel cage stress (Fig. 3d, inset), alcohol did not affect locomotor activity levels after injection and after novel cage stress (alcohol effect: F(3,30) = 1.67, p = 0.20, NS; alcohol × stress: F(3,30) = 0.90, p = 0.45, NS).
THIP
Summary
THIP reduced the SIH response and basal body temperature at its highest dose. THIP reduced locomotor activity after novel cage stress (Fig. 3e, f; n = 10).
Body temperature
Basal body temperature was overall reduced by THIP (THIP effect: F(3,27) = 5.44, p < 0.01). Also, the SIH response (time effect: F(12,108) = 12.59, p < 0.001) was reduced by THIP (THIP × time interaction: F(36,324) = 4.25, p < 0.001). Simple contrasts revealed a significant difference in basal body temperature between the vehicle and 10 mg/kg condition (F(1,9) = 15.40, p < 0.01), whereas the other doses did not affect basal body temperature (vehicle–0.3 mg/kg condition F(1,9) = 1.11, p = 0.32, NS; vehicle–3 mg/kg condition F(1,9) = 0.11, p = 0.75, NS). The calculated SIH response revealed that THIP reduced the SIH response (F(3,27) = 4.64, p = 0.01). Simple contrasts revealed that only the highest dose reduced the SIH response (0.3 mg/kg–vehicle: F(1,9) = 0.31, p = 0.59, NS; 3 mg/kg–vehicle: F(1,9) = 0.25, p = 0.63; 10 mg/kg–vehicle: F(1,10) = 6.15, p < 0.05) (Fig. 3e, inset).
Locomotor activity
The stress-induced locomotor response (time effect: F(12,108) = 12.35, p < 0.001) was reduced by THIP (THIP × time interaction: F(36,324) = 1.96, p < 0.001; THIP effect: F(3,27) = 2.43, p = 0.09, trend). When cumulating locomotor activity levels after injection and after novel cage stress (Fig. 3f, inset), THIP reduced locomotor activity levels only after the novel cage procedure (THIP × stress interaction: F(1,9) = 3.37, p < 0.05), although overall locomotor activity was not reduced (THIP effect: F(3,27) = 1.18, p = 0.34, NS) and overall locomotor activity levels after injection and novel cage stress were not different (stress effect: F(1,9) = 0.18, p = 0.68, NS).
Discussion
In the present study, we examined the effects of various GABAAergic compounds on temperature and locomotor responses to acute stress. The SIH model uses the rise in body temperature in response to stress to assess anxiolytic drug effects and provides a translational approach to anxiety research (Vinkers et al. 2008). We found that the administration of the nonselective GABAA receptor agonist diazepam resulted in a dose-dependent attenuation of the SIH and basal and stress-induced locomotor activity responses, indicating that diazepam induces both anxiolytic and sedative effects. These findings support and extend previous studies on diazepam in the SIH paradigm in mice (Olivier et al. 2002). Zolpidem, an intermediate selective GABAA receptor α1 subunit agonist, decreased basal core body temperature and attenuated basal and stress-induced locomotor and temperature responses in a dose-dependent fashion. The sedative effect of zolpidem in vivo is mediated by the α1 subunit (Crestani et al. 2000), and zolpidem does not possess any anxiolytic properties (Kralic et al. 2002; Mathiasen et al. 2007). However, we cannot exclude that the results of the higher doses of zolpidem may be the result of nonspecific GABAA receptor activation. Also, the reduction of the SIH response by zolpidem is most likely the result of strong hypothermic effects on basal body temperature, disturbing physiological homeostatic mechanisms (Olivier et al. 2003).
βCCt shows a high affinity for the GABAA receptor α1 subunit with considerably lower affinity for GABAA receptor α2, α3, and α4 subunits and has comparable low efficacy at all α subunits. (Basile et al. 2006; Huang et al. 2000). Administration of βCCt alone had no effect on either basal body temperature or novel cage-induced temperature and locomotor activity responses. However, prior injection with βCCt antagonized hypothermic effects of both diazepam and zolpidem and reversed zolpidem-induced locomotor sedation (Figs. 1 and 2). In contrast, βCCt did not antagonize the diazepam-induced locomotor sedation, which may be attributed to the fact that diazepam exerts a broader pharmacological GABAA agonistic profile while zolpidem action is restricted to the GABAA receptor α1 subunit. Basal body temperature reduction after diazepam administration was only observed in the combination βCCt/diazepam experiment and not when solely diazepam was injected. We do not have an explanation for this puzzling observation; the only experimental difference was the presence of a double injection within 10 min. Mice do consistently show a reduction in basal body temperature after administration of diazepam (Olivier et al. 2002; Van Bogaert et al. 2006), and better regulated homeostasis in the rat may account for an absent hypothermia when diazepam was administered. Our results suggest a role for the GABAA receptor α1 subunit in hypothermic and locomotor sedative actions of GABAAergic drugs. Some studies have suggested that anxiolytic effects of benzodiazepines can be reversed with βCCt (Belzung et al. 2000; Griebel et al. 1999). However, this may be the result of decreased sedation rather than a reversal of anxiolytic effects, since sedation caused by diazepam and zolpidem has been shown to be reversible with high doses of βCCt (Basile et al. 2006; Griebel et al. 1999). The hypothermic effects after activation of the GABAA receptor α1 subunit has been extensively studied in mice (Van Bogaert et al. 2006). The α1 subunit is abundantly expressed throughout the brain, and a higher expression of the α1 subunit is present in the hypothalamic preoptic area and dorsomedial hypothalamus compared to the α2 and α3 subunits (Pirker et al. 2000). These areas are thought to play a major role in thermoregulation (Boulant 2000; Dimicco and Zaretsky 2007; Nagashima et al. 2000) and may account for the α1 involvement in the regulation of basal body temperature.
A putative role for the GABAA receptor α3 subunit in anxiety was confirmed with GABAA receptor α3 subunit agonist TP003 that attenuated the SIH response without affecting basal body temperature levels (Fig. 3a). Also, when combined with GABAA receptor α1 subunit antagonist βCCt, diazepam still reduced the SIH response, putatively through activation of the α2/3 subunit. Although transgenic mice lacking benzodiazepine sensitivity in the α3 subunit did not show altered anxiolytic actions of diazepam (Low et al. 2000; Rudolph and Mohler 2004), pharmacological studies have pointed to a role for this subunit in anxiolysis (Atack et al. 2005; Atack et al. 2006; Dias et al. 2005) as might be expected from high α3 subunit expression in brain areas involved in acute stress responses (Pirker et al. 2000). Anxiolytic effects of TP003 were found in the elevated plus maze (rats) and in a conditioned emotional response test (squirrel monkeys) (Dias et al. 2005). Our findings support and extend previous experiments suggesting GABAA receptor α2 and α3 subunits as the main regulatory subunits mediating anxiolytic effects (Atack et al. 2005; Dias et al. 2005). Stress-induced locomotor responses after novel cage stress were reduced at all TP003 doses, but only after novel cage stress and not immediately after injection like in the case of diazepam and zolpidem (Fig. 3b). This contrasts with another study in mice that did not show any sedative locomotor effects of TP003 (Dias et al. 2005). Although being α3 subunit-selective, TP003 also has low modulation via α1-, α2-, and α5-containing subtypes (Dias et al. 2005). Also, differences in metabolizing enzymes exist between animal species, resulting in different clearance rates which are frequently thought to be responsible for differences in behavioral responses. For GABAA receptor agonists, one study of nitrazepam found much higher plasma levels in rats than in mice after a dose of nitrazepam (Takeno et al. 1993), whereas another study found that the oral bioavailability of L-838417, a α1 subunit antagonist and α2/α3 partial subunit agonist, in mice was very poor compared to bioavailability in rats (Scott-Stevens et al. 2005). Therefore, a lack of sedative action of TP003 in mice compared to rats can possibly be ascribed to lower plasma levels of TP003 caused by a more rapid metabolism of TP003 in mice.
Locomotor activity responses to stress are used as an output parameter in various anxiety paradigms such as the elevated plus maze, the open field test, and the light/dark test. Open-arm entries, a lit box, or center of a field all putatively lead to an anxiety state, but also cage exchange as used in the current experiments leads to similar increases in distances traveled and velocities (de Visser et al. 2006). In general, stress-induced behavior in rodents consists of exploration on one hand and anxiety-driven avoidance behavior on the other hand, and there is no easy way of establishing the relationship between exploration and anxiety. Anxiolytic drugs increase explorative behavior and locomotor activity (Belzung and Berton 1997), but in higher doses cause general locomotor sedation, interfering with a good test interpretation (Dawson et al. 1995). Therefore, sedative effects of both diazepam and zolpidem cause a decrease in locomotor activity (Davies et al. 1994; Elliot and White 2001). However, the sedative effects of benzodiazepines in the elevated plus maze are no longer present after a point mutation of the α1 subunit (McKernan et al. 2000; Rudolph et al. 1999), indicating that the α1 subunit is closely involved in benzodiazepine-induced locomotor activity reduction. McKernan et al. showed that diazepam (3 mg/kg) even increased locomotor activity in α1 subunit point-mutated mice compared to wild-type controls. In contrast, myorelaxant effects of diazepam in the rotarod assay remain present in the α1 subunit KO mice, suggesting that the locomotor activity attenuation is not the mere result of muscle relaxation. Other studies showed that βCCt antagonized the locomotor depressant effects of zolpidem and diazepam on open field locomotor activity in mice (Griebel et al. 1999) as well as the elevated plus maze (Savic et al. 2004). All in all, there is ample evidence that locomotor depressant actions of zolpidem and the benzodiazepines are mediated via the α1 subunit of the GABAA receptor. Anxiolytic drugs completely devoid of sedative side effects would, therefore, either increase or not affect locomotor activity parameters after novelty-induced stress.
Alcohol reduced basal body temperature at higher doses without affecting stress-induced locomotor responses (Fig. 3c). Only the highest dose reduced the SIH response, an effect that was already earlier observed in mice (Olivier et al. 2003). Although acute administration of alcohol is known to possess an anxiolytic profile, the effects are known to be different from benzodiazepines (Langen et al. 2002) as alcohol binds to extrasynaptic GABAA receptors containing α4 or α6 and δ subunits (Wallner et al. 2003). However, we used higher doses that could have lost extrasynaptic binding selectivity. Also, alcohol at higher doses may act on NMDA, serotonin, and glycine receptors (Crews et al. 1996; Davies 2003; Harris 1999). THIP reduced basal body temperature and SIH and locomotor activity responses only at the highest dose tested (10 mg/kg), whereas lower doses did not have any effect (Fig. 3e). THIP has been shown to enhance sleep episodes (Lancel and Langebartels 2000) with little affinity for benzodiazepine receptors. Rather, THIP binds to extrasynaptic GABAA receptors containing a δ subunit (Wafford and Ebert 2006), and a role for the GABAA receptor δ subunit in neurosteroid-mediated anxiolytic effects has been proposed (Mihalek et al. 1999). However, it seems more likely that the strong hypothermic effects of the highest dose of THIP are due to interference with physiological thermoregulation (Olivier et al. 2003). Interaction between effects on sleep and thermoregulation are possible because of common neural pathways within the preoptic area and anterior hypothalamus (Frosini et al. 2004). Indeed, THIP synchronized hypothermic and EEG effects in rabbits (Frosini et al. 2004). Interestingly, alcohol did not affect locomotor activity at all doses and THIP affected locomotor activity only at high doses (Fig. 3d, f), whereas the other synaptic compounds all reduced locomotor activity to some extent. Other studies have found that alcohol impaired rotarod performance at lower doses (Zaleski et al. 2001). Although our high doses may have lost extrasynaptic selectivity, this indicates that locomotor activity may be differentially controlled by extrasynaptic and synaptic receptor populations. This is supported by a lack of cross-tolerance in the rotarod test between zolpidem and THIP (Voss et al. 2003).
The SIH amplitude decreased over the course of the experiments from 0.7°C at the start of the experiments to 0.2–0.3°C in the final experiments, as did locomotor activity levels after novel cage stress. Habituation to the experimental procedure may account for a decreased SIH response, although previous methodological testing has not revealed any habituation using a 1-week interval, even when testing occurred for over a year (Bouwknecht et al. 2007; Olivier et al. 2003; Van der Heyden et al. 1997). Also, the manually calculated SIH response from the time graphs is generally in complete agreement with the time graphs. Only when drugs are tested at doses that markedly decrease body temperature, there appears to be a small difference between the calculated SIH response and the time graphs. This difference is attributable to the fact that the calculated SIH response is based on the maximum temperature during the first 30 min after stress. In those cases in which body temperature is decreasing after stress induction, the maximum is likely to be close to the start of that 30-min period. In this way, the calculated SIH response in these cases is likely to yield a result close to 0°C, whereas a decreasing basal body temperature seems to indicate a negative SIH response. The differences, however, are small and do not change the interpretation of our data.
The most important finding in the present study is that the GABAA receptor modulates temperature and locomotor stress responses as well as basal body temperature processes through different GABAA receptor subunits. More specifically, the GABAA α1 receptor subunit was found to be essential for basal body temperature regulation and for inducing locomotor sedation, whereas the GABAA receptor α2 and α3 subunit exerted anxiolytic effects by attenuating the SIH response. Nonbenzodiazepine GABAA activity is less involved in thermoregulation and locomotor sedation, as suggested by the effects of alcohol and THIP. In conclusion, we show that the use of home cage temperature and locomotor stress responses provides a successful approach to anxiety research and possesses an enormous potential to pharmacologically study the effects of GABAAergic drugs. The SIH model uses a simultaneously collected independent parameter and may possess additional value over locomotor activity parameters only.
References
Atack JR (2005) The benzodiazepine binding site of GABA(A) receptors as a target for the development of novel anxiolytics. Expert Opin Investig Drugs 14:601–618
Atack JR, Smith AJ, Emms F, McKernan RM (1999) Regional differences in the inhibition of mouse in vivo [3H]Ro 15-1788 binding reflect selectivity for alpha 1 versus alpha 2 and alpha 3 subunit-containing GABAA receptors. Neuropsychopharmacology 20:255–262
Atack JR, Hutson PH, Collinson N, Marshall G, Bentley G, Moyes C, Cook SM, Collins I, Wafford K, McKernan RM, Dawson GR (2005) Anxiogenic properties of an inverse agonist selective for alpha3 subunit-containing GABA A receptors. Br J Pharmacol 144:357–366
Atack JR, Wafford KA, Tye SJ, Cook SM, Sohal B, Pike A, Sur C, Melillo D, Bristow L, Bromidge F, Ragan I, Kerby J, Street L, Carling R, Castro JL, Whiting P, Dawson GR, McKernan RM (2006) TPA023 [7-(1,1-dimethylethyl)-6-(2-ethyl-2H-1,2,4-triazol-3-ylmethoxy)-3-(2-fluor ophenyl)-1,2,4-triazolo[4,3-b]pyridazine], an agonist selective for alpha2-and alpha3-containing GABAA receptors, is a nonsedating anxiolytic in rodents and primates. J Pharmacol Exp Ther 316:410–422
Basile C, Lippa AS, Skolnick P (2006) GABAA receptor modulators as anxioselective anxiolytics. Drug Discov Today 3:475–481
Belzung C, Berton F (1997) Further pharmacological validation of the BALB/c neophobia in the free exploratory paradigm as an animal model of trait anxiety. Behav Pharmacol 8:541–548
Belzung C, Le Guisquet AM, Griebel G (2000) Beta-CCT, a selective BZ-omega1 receptor antagonist, blocks the anti-anxiety but not the amnesic action of chlordiazepoxide in mice. Behav Pharmacol 11:125–131
Borghese CM, Storustovu S, Ebert B, Herd MB, Belelli D, Lambert JJ, Marshall G, Wafford KA, Harris RA (2006) The delta subunit of gamma-aminobutyric acid type A receptors does not confer sensitivity to low concentrations of ethanol. J Pharmacol Exp Ther 316:1360–1368
Boulant JA (2000) Role of the preoptic-anterior hypothalamus in thermoregulation and fever. Clin Infect Dis 31(Suppl 5):S157–S161
Bouwknecht JA, Olivier B, Paylor RE (2007) The stress-induced hyperthermia paradigm as a physiological animal model for anxiety: a review of pharmacological and genetic studies in the mouse. Neurosci Biobehav Rev 31:41–59
Crestani F, Martin JR, Mohler H, Rudolph U (2000) Mechanism of action of the hypnotic zolpidem in vivo. Br J Pharmacol 131:1251–1254
Crews FT, Morrow AL, Criswell H, Breese G (1996) Effects of ethanol on ion channels. Int Rev Neurobiol 39:283–367
Davies M (2003) The role of GABAA receptors in mediating the effects of alcohol in the central nervous system. J Psychiatry Neurosci 28:263–274
Davies MF, Onaivi ES, Chen SW, Maguire PA, Tsai NF, Loew GH (1994) Evidence for central benzodiazepine receptor heterogeneity from behavior tests. Pharmacol Biochem Behav 49:47–56
Dawson GR, Crawford SP, Collinson N, Iversen SD, Tricklebank MD (1995) Evidence that the anxiolytic-like effects of chlordiazepoxide on the elevated plus maze are confounded by increases in locomotor activity. Psychopharmacology (Berl) 118:316–323
de Haas SL, de Visser SJ, van der Post JP, de Smet M, Schoemaker RC, Rijnbeek B, Cohen AF, Vega JM, Agrawal NG, Goel TV, Simpson RC, Pearson LK, Li S, Hesney M, Murphy MG, van Gerven JM (2007) Pharmacodynamic and pharmacokinetic effects of TPA023, a GABA(A) alpha(2,3) subtype-selective agonist, compared to lorazepam and placebo in healthy volunteers. J Psychopharmacol 21:374–383
de Visser L, van den Bos R, Kuurman WW, Kas MJ, Spruijt BM (2006) Novel approach to the behavioural characterization of inbred mice: automated home cage observations. Genes Brain Behav 5:458–466
Dias R, Sheppard WF, Fradley RL, Garrett EM, Stanley JL, Tye SJ, Goodacre S, Lincoln RJ, Cook SM, Conley R, Hallett D, Humphries AC, Thompson SA, Wafford KA, Street LJ, Castro JL, Whiting PJ, Rosahl TW, Atack JR, McKernan RM, Dawson GR, Reynolds DS (2005) Evidence for a significant role of alpha 3-containing GABAA receptors in mediating the anxiolytic effects of benzodiazepines. J Neurosci 25:10682–10688
Dimicco JA, Zaretsky DV (2007) The dorsomedial hypothalamus: a new player in thermoregulation. Am J Physiol Regul Integr Comp Physiol 292:R47–R63
Ebert B, Wafford KA, Deacon S (2006) Treating insomnia: current and investigational pharmacological approaches. Pharmacol Ther 112:612–629
Elfline GS, Branda EM, Babich M, Quock RM (2004) Antagonism by NOS inhibition of the behavioral effects of benzodiazepine and GABAA receptor agonists in the mouse elevated plus-maze. Neuropsychopharmacology 29:1419–1425
Elliot EE, White JM (2001) The acute effects of zolpidem compared to diazepam and lorazepam using radiotelemetry. Neuropharmacology 40:717–721
Frosini M, Valoti M, Sgaragli G (2004) Changes in rectal temperature and ECoG spectral power of sensorimotor cortex elicited in conscious rabbits by i.c.v. injection of GABA, GABA(A) and GABA(B) agonists and antagonists. Br J Pharmacol 141:152–162
Goodacre SCH, David J, Humphries AC, Jones P, Kelly SM, Merchant KJ, Moore KW, Reader M (2003) Preparation of 8-fluoro-3-phenylimidazo[1,2-a]pyridine derivatives as ligands for gamma-aminobutyric acid (GABA) receptors. PCT Int. Appl. United States Patent 7,279,580
Griebel G, Perrault G, Letang V, Granger P, Avenet P, Schoemaker H, Sanger DJ (1999) New evidence that the pharmacological effects of benzodiazepine receptor ligands can be associated with activities at different BZ (omega) receptor subtypes. Psychopharmacology (Berl) 146:205–213
Harris RA (1999) Ethanol actions on multiple ion channels: which are important? Alcohol Clin Exp Res 23:1563–1570
Huang Q, Cox ED, Gan T, Ma C, Bennett DW, McKernan RM, Cook JM (1999) Studies of molecular pharmacophore/receptor models for GABAA/benzodiazepine receptor subtypes: binding affinities of substituted beta-carbolines at recombinant alpha x beta 3 gamma 2 subtypes and quantitative structure–activity relationship studies via a comparative molecular field analysis. Drug Des Discov 16:55–76
Huang Q, He X, Ma C, Liu R, Yu S, Dayer CA, Wenger GR, McKernan R, Cook JM (2000) Pharmacophore/receptor models for GABA(A)/BzR subtypes (alpha1beta3gamma2, alpha5beta3gamma2, and alpha6beta3gamma2) via a comprehensive ligand-mapping approach. J Med Chem 43:71–95
Humphries AC, Gancia E, Gilligan MT, Goodacre S, Hallett D, Merchant KJ, Thomas SR (2006) 8-Fluoroimidazo[1,2-a]pyridine: synthesis, physicochemical properties and evaluation as a bioisosteric replacement for imidazo[1,2-a]pyrimidine in an allosteric modulator ligand of the GABAA receptor. Bioorg Med Chem Lett 16:1518–1522
Jia F, Pignataro L, Schofield CM, Yue M, Harrison NL, Goldstein PA (2005) An extrasynaptic GABAA receptor mediates tonic inhibition in thalamic VB neurons. J Neurophysiol 94:4491–4501
Korpi ER, Grunder G, Luddens H (2002) Drug interactions at GABA(A) receptors. Prog Neurobiol 67:113–159
Kralic JE, O’Buckley TK, Khisti RT, Hodge CW, Homanics GE, Morrow AL (2002) GABA(A) receptor alpha-1 subunit deletion alters receptor subtype assembly, pharmacological and behavioral responses to benzodiazepines and zolpidem. Neuropharmacology 43:685–694
Kralic JE, Wheeler M, Renzi K, Ferguson C, O’Buckley TK, Grobin AC, Morrow AL, Homanics GE (2003) Deletion of GABAA receptor alpha 1 subunit-containing receptors alters responses to ethanol and other anesthetics. J Pharmacol Exp Ther 305:600–607
Lancel M, Langebartels A (2000) gamma-aminobutyric Acid(A) (GABA(A)) agonist 4,5,6, 7-tetrahydroisoxazolo[4,5-c]pyridin-3-ol persistently increases sleep maintenance and intensity during chronic administration to rats. J Pharmacol Exp Ther 293:1084–1090
Langen B, Dietze S, Fink H (2002) Acute effect of ethanol on anxiety and 5-HT in the prefrontal cortex of rats. Alcohol 27:135–141
Low K, Crestani F, Keist R, Benke D, Brunig I, Benson JA, Fritschy JM, Rulicke T, Bluethmann H, Mohler H, Rudolph U (2000) Molecular and neuronal substrate for the selective attenuation of anxiety. Science 290:131–134
Mathiasen LS, Rodgers RJ, Mirza NR (2007) Comparative effects of nonselective and subtype-selective gamma-aminobutyric acidA receptor positive modulators in the rat-conditioned emotional response test. Behav Pharmacol 18:191–203
McKernan RM, Rosahl TW, Reynolds DS, Sur C, Wafford KA, Atack JR, Farrar S, Myers J, Cook G, Ferris P, Garrett L, Bristow L, Marshall G, Macaulay A, Brown N, Howell O, Moore KW, Carling RW, Street LJ, Castro JL, Ragan CI, Dawson GR, Whiting PJ (2000) Sedative but not anxiolytic properties of benzodiazepines are mediated by the GABA(A) receptor alpha1 subtype. Nat Neurosci 3:587–592
Mihalek RM, Banerjee PK, Korpi ER, Quinlan JJ, Firestone LL, Mi ZP, Lagenaur C, Tretter V, Sieghart W, Anagnostaras SG, Sage JR, Fanselow MS, Guidotti A, Spigelman I, Li Z, DeLorey TM, Olsen RW, Homanics GE (1999) Attenuated sensitivity to neuroactive steroids in gamma-aminobutyrate type A receptor delta subunit knockout mice. Proc Natl Acad Sci USA 96:12905–12910
Mihalek RM, Bowers BJ, Wehner JM, Kralic JE, VanDoren MJ, Morrow AL, Homanics GE (2001) GABA(A)-receptor delta subunit knockout mice have multiple defects in behavioral responses to ethanol. Alcohol Clin Exp Res 25:1708–1718
Nagashima K, Nakai S, Tanaka M, Kanosue K (2000) Neuronal circuitries involved in thermoregulation. Auton Neurosci 85:18–25
Nemeroff CB (2003) The role of GABA in the pathophysiology and treatment of anxiety disorders. Psychopharmacol Bull 37:133–146
Nusser Z, Sieghart W, Somogyi P (1998) Segregation of different GABAA receptors to synaptic and extrasynaptic membranes of cerebellar granule cells. J Neurosci 18:1693–1703
Olivier B, Bouwknecht JA, Pattij T, Leahy C, van Oorschot R, Zethof TJ (2002) GABAA-benzodiazepine receptor complex ligands and stress-induced hyperthermia in singly housed mice. Pharmacol Biochem Behav 72:179–188
Olivier B, Zethof T, Pattij T, van Boogaert M, van Oorschot R, Leahy C, Oosting R, Bouwknecht A, Veening J, van der Gugten J, Groenink L (2003) Stress-induced hyperthermia and anxiety: pharmacological validation. Eur J Pharmacol 463:117–132
Pattij T, Hijzen TH, Groenink L, Oosting RS, van der Gugten J, Maes RA, Hen R, Olivier B (2001) Stress-induced hyperthermia in the 5-HT(1A) receptor knockout mouse is normal. Biol Psychiatry 49:569–574
Petroski RE, Pomeroy JE, Das R, Bowman H, Yang W, Chen AP, Foster AC (2006) Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors. J Pharmacol Exp Ther 317:369–377
Pirker S, Schwarzer C, Wieselthaler A, Sieghart W, Sperk G (2000) GABA(A) receptors: immunocytochemical distribution of 13 subunits in the adult rat brain. Neuroscience 101:815–850
Pritchett DB, Luddens H, Seeburg PH (1989) Type I and type II GABAA-benzodiazepine receptors produced in transfected cells. Science 245:1389–1392
Rowlett JK, Platt DM, Lelas S, Atack JR, Dawson GR (2005) Different GABAA receptor subtypes mediate the anxiolytic, abuse-related, and motor effects of benzodiazepine-like drugs in primates. Proc Natl Acad Sci USA 102:915–920
Rudolph U, Mohler H (2004) Analysis of GABAA receptor function and dissection of the pharmacology of benzodiazepines and general anesthetics through mouse genetics. Annu Rev Pharmacol Toxicol 44:475–498
Rudolph U, Crestani F, Benke D, Brunig I, Benson JA, Fritschy JM, Martin JR, Bluethmann H, Mohler H (1999) Benzodiazepine actions mediated by specific gamma-aminobutyric acid(A) receptor subtypes. Nature 401:796–800
Savic MM, Obradovic DI, Ugresic ND, Cook JM, Yin W, Bokonjic DR (2004) Bidirectional effects of benzodiazepine binding site ligands in the elevated plus-maze: differential antagonism by flumazenil and beta-CCt. Pharmacol Biochem Behav 79:279–290
Scott-Stevens P, Atack JR, Sohal B, Worboys P (2005) Rodent pharmacokinetics and receptor occupancy of the GABAA receptor subtype selective benzodiazepine site ligand L-838417. Biopharm Drug Dispos 26:13–20
Stewart SH, Westra HA (2002) Benzodiazepine side-effects: from the bench to the clinic. Curr Pharm Des 8:1–3
Takeno S, Hirano Y, Kitamura A, Sakai T (1993) Comparative developmental toxicity and metabolism of nitrazepam in rats and mice. Toxicol Appl Pharmacol 121:233–238
Tretter V, Ehya N, Fuchs K, Sieghart W (1997) Stoichiometry and assembly of a recombinant GABAA receptor subtype. J Neurosci 17:2728–2737
Van Bogaert M, Oosting R, Toth M, Groenink L, van Oorschot R, Olivier B (2006) Effects of genetic background and null mutation of 5-HT1A receptors on basal and stress-induced body temperature: modulation by serotonergic and GABAA-ergic drugs. Eur J Pharmacol 550:84–90
Van der Heyden JA, Zethof TJ, Olivier B (1997) Stress-induced hyperthermia in singly housed mice. Physiol Behav 62:463–470
Vinkers CH, van Bogaert MJ, Klanker M, Korte SM, Oosting R, Hanania T, Hopkins SC, Olivier B, Groenink L (2008) Translational aspects of pharmacological research into anxiety disorders: the stress-induced hyperthermia (SIH) paradigm. Eur J Pharmacol 585:407–425
Voss J, Sanchez C, Michelsen S, Ebert B (2003) Rotarod studies in the rat of the GABAA receptor agonist gaboxadol: lack of ethanol potentiation and benzodiazepine cross-tolerance. Eur J Pharmacol 482:215–222
Wafford KA, Ebert B (2006) Gaboxadol—a new awakening in sleep. Curr Opin Pharmacol 6:30–36
Wallner M, Hanchar HJ, Olsen RW (2003) Ethanol enhances alpha 4 beta 3 delta and alpha 6 beta 3 delta gamma-aminobutyric acid type A receptors at low concentrations known to affect humans. Proc Natl Acad Sci USA 100:15218–15223
Zaleski MJ, Nunes Filho JR, Lemos T, Morato GS (2001) GABA(B) receptors play a role in the development of tolerance to ethanol in mice. Psychopharmacology (Berl) 153:415–424
Acknowledgements
We would like to thank Ruud van Oorschot and Koen Westphal for their excellent technical assistance. The authors declare that over the past 3 years, JC has received compensation from Bristol Myers Squibb, Xintria Pharmaceutical Corporation, Aldrich Chemical Corporation, and Cambridge-Major Laboratories, Inc. Seth C. Hopkins is an employee of Sepracor Inc. This work was supported in part by NIAAA (AA016179).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Vinkers, C.H., Klanker, M., Groenink, L. et al. Dissociating anxiolytic and sedative effects of GABAAergic drugs using temperature and locomotor responses to acute stress. Psychopharmacology 204, 299–311 (2009). https://doi.org/10.1007/s00213-009-1460-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-009-1460-4