Abstract
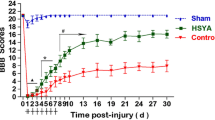
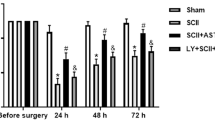
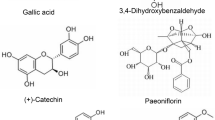
Spinal cord edema is a quick-onset phenomenon with long-term effects. This complication is associated with inflammatory responses, as well as poor motor function. No effective treatment has been developed against spinal edema, which urges the need to provide novel therapies. Astaxanthin (AST) is a fat-soluble carotenoid with anti-inflammatory effects and a promising candidate for treating neurological disorders. This study aimed to investigate the underlying mechanism of AST on the inhibition of spinal cord edema, astrocyte activation, and reduction of inflammatory responsesin a rat compression spinal cord injury (SCI) model. Male rats underwent laminectomy at thoracic 8–9, and the SCI model was induced using an aneurysm clip. After SCI, rats received dimethyl sulfoxide or AST via intrathecal injection. The effects of AST were examined on the motor function, spinal cord edema, integrity of blood-spinal cord barrier (BSCB), and expression of high mobility group box 1 (HMGB1), toll-like receptor 4 (TLR4), nuclear factor-kappa B (NF-κB), glial fibrillary acidic protein (GFAP), and aquaporin-4 (AQP4), and matrix metallopeptidase- 9 (MMP-9) post-SCI. We showed that AST potentially improved the recovery of motor function and inhibited the spinal cord edema via maintaining the integrity of BSCB, reducing the expression of HMGB1, TLR4, and NF-κB, MMP-9 as well as downregulation of astrocyte activation (GFAP) and AQP4 expression. AST improves motor function and reduces edema and inflammatory responses in the spinal tissue. These effects are mediated by suppression of the HMGB1/TLR4/NF-κB signaling pathway, suppressing post-SCI astrocyte activation, and decreasing AQP4 and MMP-9 expression.
Graphical abstract






Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AQP4:
-
Aquapurin-4
- AST:
-
Astaxanthin
- BBB:
-
Basso, Beattie and Bresnahan
- BSA:
-
Bovine serum albumin
- BSCB:
-
Blood-spinal cord barrier
- CAM:
-
Calmodulin
- DMSO:
-
Dimethyl sulfoxide
- EB:
-
Evans blue
- FSA:
-
Foot-stepping angle
- GFAP:
-
Glial fibrillary acidic protein
- HMGB1:
-
High mobility group box-1
- MMP-9:
-
Matrix metalloproteinase-9
- MRI:
-
Magnetic Resonance Imaging
- NF-Κb:
-
Nuclear factor-kappa B
- PBS:
-
Phosphate-buffered saline
- PKA:
-
Protein kinase A
- PVDF:
-
Polyvinylidene difluoride
- RAGE:
-
Receptor of advanced glycation end product
- RHI:
-
Rump height index
- RI:
-
Recovery index
- SAH:
-
Subarachnoid hemorrhage
- SCI:
-
Spinal cord injury
- TBI:
-
Traumatic brain injury
- TLR4:
-
Toll-like receptor-4
- TRPV4:
-
Transient receptor potential vanilloid-type 4
- TNF:
-
Tumor necrosis factor
References
Agalave NM, Svensson CI (2014) Extracellular high-mobility group box 1 protein (HMGB1) as a mediator of persistent pain. Mol Med 20:569–578
Anwar MA, Al Shehabi TS, Eid AH (2016) Inflammogenesis of secondary spinal cord injury. Front Cell Neurosci 10:98
Cabrera-Aldana EE, Ruelas F, Aranda C, Rincon-Heredia R, Martínez-Cruz A, Reyes-Sánchez A, Guizar-Sahagún G, Tovar-y-Romo LB (2017) Methylprednisolone administration following spinal cord injury reduces aquaporin 4 expression and exacerbates edema. Mediators Inflamm 2017: 4792932
Cho N, Hachem LD, Fehlings MG (2017) Spinal cord edema after spinal cord injury: from pathogenesis to management. Brain Edema. Elsevier, pp 261–275
Fakhri S, Abbaszadeh F, Dargahi L, Jorjani M (2018a) Astaxanthin: A mechanistic review on its biological activities and health benefits. Pharmacol Res 136:1–20
Fakhri S, Dargahi L, Abbaszadeh F, Jorjani M (2018b) Astaxanthin attenuates neuroinflammation contributed to the neuropathic pain and motor dysfunction following compression spinal cord injury. Brain Res Bull 143:217–224
Fakhri S, Dargahi L, Abbaszadeh F, Jorjani M (2019) Effects of astaxanthin on sensory-motor function in a compression model of spinal cord injury: involvement of ERK and AKT signalling pathway. Eur J Pain 23:750–764
Figley SA, Khosravi R, Legasto JM, Tseng Y-F, Fehlings MG (2014) Characterization of vascular disruption and blood–spinal cord barrier permeability following traumatic spinal cord injury. J Neurotrauma 31:541–552
Huang Y, Li S-n, Zhou X-y, Zhang L-x, Chen G-x, Wang T-h, Xia Q-j, Liang N, Zhang X (2019) The dual role of AQP4 in cytotoxic and vasogenic edema following spinal cord contusion and its possible association with energy metabolism via COX5A. Front Neurosci 13:584
Huang S, Jiang H, Hu H, Lv D (2021) Targeting AQP4 localization as a novel therapeutic target in CNS edema. Acta Biochim Biophys Sin 53:269–272
Ieong C, Sun H, Wang Q, Ma J (2018) Glycyrrhizin suppresses the expressions of HMGB1 and ameliorates inflammative effect after acute subarachnoid hemorrhage in rat model. J Clin Neurosci 47:278–284
Illarionova N, Gunnarson E, Li Y, Brismar H, Bondar A, Zelenin S, Aperia A (2010) Functional and molecular interactions between aquaporins and Na, K-ATPase. Neuroscience 168:915–925
Jin L-Y, Li J, Wang K-F, Xia W-W, Zhu Z-Q, Wang C-R, Li X-F, Liu H-Y (2021) Blood–spinal cord barrier in spinal cord injury: a review. J Neurotrauma 38:1203–1224
Kitchen P, Day RE, Taylor LH, Salman MM, Bill RM, Conner MT, Conner AC (2015) Identification and molecular mechanisms of the rapid tonicity-induced relocalization of the aquaporin 4 channel. J Biol Chem 290:16873–16881
Kumar H, Ropper AE, Lee S-H, Han I (2017) Propitious therapeutic modulators to prevent blood-spinal cord barrier disruption in spinal cord injury. Mol Neurobiol 54:3578–3590
Laird MD, Shields JS, Sukumari-Ramesh S, Kimbler DE, Fessler RD, Shakir B, Youssef P, Yanasak N, Vender JR, Dhandapani KM (2014) High mobility group box protein-1 promotes cerebral edema after traumatic brain injury via activation of toll-like receptor 4. Glia 62:26–38
Lee JY, Kim HS, Choi HY, Oh TH, Yune TY (2012) Fluoxetine inhibits matrix metalloprotease activation and prevents disruption of blood–spinal cord barrier after spinal cord injury. Brain 135:2375–2389
Liu X, Wang Y, Yang J, Liu Y, Zhou D, Hou M, Xiang L (2015) Anti-edema effect of melatonin on spinal cord injury in rats. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 159:220–226
Liu S, Mao J, Wang T, Fu X (2017) Downregulation of aquaporin-4 protects brain against hypoxia ischemia via anti-inflammatory mechanism. Mol Neurobiol 54:6426–6435
Masoudi A, Dargahi L, Abbaszadeh F, Pourgholami MH, Asgari A, Manoochehri M, Jorjani M (2017) Neuroprotective effects of astaxanthin in a rat model of spinal cord injury. Behav Brain Res 329:104–110
Nishibori M, Wang D, Ousaka D, Wake H (2020) High mobility group box-1 and blood–brain barrier disruption. Cells 9:2650
Noble LJ, Donovan F, Igarashi T, Goussev S, Werb Z (2002) Matrix metalloproteinases limit functional recovery after spinal cord injury by modulation of early vascular events. J Neurosci Res 22:7526–7535
Ohnishi M, Monda A, Takemoto R, Fujimoto Y, Sugitani M, Iwamura T, Hiroyasu T, Inoue A (2014) High-mobility group box 1 up-regulates aquaporin 4 expression via microglia–astrocyte interaction. Neurochem Int 75:32–38
Oklinski MK, Skowronski MT, Skowronska A, Rützler M, Nørgaard K, Nieland JD, Kwon T-H, Nielsen S (2016) Aquaporins in the spinal cord. Int J Mol Sci 17:2050
Oshio K, Binder D, Yang B, Schecter S, Verkman A, Manley G (2004) Expression of aquaporin water channels in mouse spinal cord. Neuroscience 127:685–693
Pan YI, Guo Y, Ma Y, Wang L, Sy Z, Mm L, Gc H (2019) Aquaporin-4 expression dynamically varies after acute spinal cord injury-induced disruption of blood spinal cord barrier in rats. Neuropathology 39:181–186
Pan Q-L, Lin F-X, Liu N, Chen R-C (2022) The role of aquaporin 4 (AQP4) in spinal cord injury. Biomed Pharmacother 145:112384
Papadopoulos MC, Verkman AS (2013) Aquaporin water channels in the nervous system. Nat Rev Neurosci 14:265–277
Park CS, Lee JY, Choi HY, Lee K, Heo Y, Ju BG, Choo H-YP, Yune TY (2020) Gallic acid attenuates blood-spinal cord barrier disruption by inhibiting Jmjd3 expression and activation after spinal cord injury. Neurobiol Dis 145:105077
Poon PC, Gupta D, Shoichet MS, Tator CH (2007) Clip compression model is useful for thoracic spinal cord injuries: histologic and functional correlates. Spine 32:2853–2859
Saini V, Lutz D, Kataria H, Kaur G, Schachner M, Loers G (2016) The polysialic acid mimetics 5-nonyloxytryptamine and vinorelbine facilitate nervous system repair. Sci Rep 6:1–12
Sandner B, Pillai DR, Heidemann RM, Schuierer G, Mueller MF, Bogdahn U, Schlachetzki F, Weidner N (2009) In vivo high-resolution imaging of the injured rat spinal cord using a 3.0 T clinical MR scanner. J Magn Reson Imaging Magn Reson Med 29:725–730
Sharma HS, Badgaiyan RD, Alm P, Mohanty S, Wiklund L (2005) Neuroprotective effects of nitric oxide synthase inhibitors in spinal cord injury-induced pathophysiology and motor functions: an experimental study in the rat. Ann N Y Acad Sci 1053:422–434
Sun L, Li M, Ma X, Feng H, Song J, Lv C, He Y (2017) Inhibition of HMGB1 reduces rat spinal cord astrocytic swelling and AQP4 expression after oxygen-glucose deprivation and reoxygenation via TLR4 and NF-κB signaling in an IL-6-dependent manner. J Neuroinflammation 14:1–18
Sun L, Li M, Ma X, Zhang L, Song J, Lv C, He Y (2019) Inhibiting high mobility group box-1 reduces early spinal cord edema and attenuates astrocyte activation and aquaporin-4 expression after spinal cord injury in rats. J Neurotrauma 36:421–435
Teng Z, Guo Z, Zhong J, Cheng C, Huang Z, Wu Y, Tang S, Luo C, Peng X, Wu H (2017) ApoE influences the blood-brain barrier through the NF-κB/MMP-9 pathway after traumatic brain injury. Sci Rep 7:1–8
Verkman A, Binder DK, Bloch O, Auguste K, Papadopoulos MC (2006) Three distinct roles of aquaporin-4 in brain function revealed by knockout mice. Biochim Biophys Acta Biomembr 1758:1085–1093
Wagner FC, Stewart WB (1981) Effect of trauma dose on spinal cord edema. J Neurosurg 54:802–806
Wang Z-R, Li Y-X, Lei H-Y, Yang D-Q, Wang L-Q, Luo M-Y (2016) Regulating effect of activated NF-κB on edema induced by traumatic brain injury of rats. Asian Pac J Trop Med 9:274–277
Zhang J, Takahashi HK, Liu K, Wake H, Liu R, Maruo T, Date I, Yoshino T, Ohtsuka A, Mori S (2011) Anti-high mobility group box-1 monoclonal antibody protects the blood–brain barrier from ischemia-induced disruption in rats. Stroke 42:1420–1428
Zhang XS, Zhang X, Zhang QR, Wu Q, Li W, Jiang TW, Hang CH (2015) Astaxanthin reduces matrix metalloproteinase-9 expression and activity in the brain after experimental subarachnoid hemorrhage in rats. Brain Res 1624:113–124
Zhang M, Cui Z, Cui H, Wang Y, Zhong C (2017) Astaxanthin protects astrocytes against trauma-induced apoptosis through inhibition of NKCC1 expression via the NF-κB signaling pathway. BMC Neurosci 18:1–12
Zhang X, Lu Y, Wu Q, Dai H, Li W, Lv S, Zhou X, Zhang X, Hang C, Wang J (2019) Astaxanthin mitigates subarachnoid hemorrhage injury primarily by increasing sirtuin 1 and inhibiting the Toll-like receptor 4 signaling pathway. FASEB J 33:722–737
Funding
This study was performed as a part of the Ph.D. thesis of Fatemeh Abbaszadeh. It was supported by a grant from the Department of Neuroscience of Iran University of Medical Science (Grant No. 18555) and the Neuroscience Research Center of Shahid Beheshti University of Medical Sciences (Grant No. 31278).
Author information
Authors and Affiliations
Contributions
F.A. was involved in the literature search, the data analysis, the conceptualization and design of the study, the graphic design and the drafting of the manuscript. S. R. was involved in performing MRI procedures and analyzing MRI data. M. J. (principal investigator), MT. J. and S. M. were involved in the conceptualization and design of the study, the critical revision of the manuscript for important intellectual content and the supervision of the study. The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All protocols for animal experiments were approved by the institutional animal Ethical Committee, the Iran University of Medical Sciences (IR.IUMS.REC.1399.1007).
Conflict of interest statement
The authors declared that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abbaszadeh, F., Jorjani, M., Joghataei, M.t. et al. Astaxanthin ameliorates spinal cord edema and astrocyte activation via suppression of HMGB1/TLR4/NF-κB signaling pathway in a rat model of spinal cord injury. Naunyn-Schmiedeberg's Arch Pharmacol 396, 3075–3086 (2023). https://doi.org/10.1007/s00210-023-02512-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-023-02512-7