Abstract
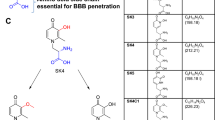
N,N’-bis(2-mercaptoethyl)isophthalamide (NBMI) is a novel lipophilic metal chelator and antioxidant used in mercury poisoning. Recent studies have suggested that NBMI may also bind to other metals such as lead and iron. Since NBMI can enter the brain, we evaluated if NBMI removes excess iron from the iron-loaded brain and ameliorates iron-induced oxidative stress. First, NBMI exhibited preferential binding to ferrous (Fe2+) iron with a negligible binding affinity to ferric (Fe3+) iron, indicating a selective chelation of labile iron. Second, NBMI protected SH-SY5Y human neuroblastoma cells from the cytotoxic effects of high iron. NBMI also decreased cellular labile iron and lessened the production of iron-induced reactive oxygen species in these cells. Deferiprone (DFP), a commonly used oral iron chelator, failed to prevent iron-induced cytotoxicity or labile iron accumulation. Next, we validated the efficacy of NBMI in Hfe H67D mutant mice, a mouse model of brain iron accumulation (BIA). Oral gavage of NBMI for 6 weeks decreased iron accumulation in the brain as well as liver, whereas DFP showed iron chelation only in the liver, but not in the brain. Notably, depletion of brain copper and anemia were observed in BIA mice treated with DFP, but not with NBMI, suggesting a superior safety profile of NBMI over DFP for long-term use. Collectively, our study demonstrates that NBMI provides a neuroprotective effect against BIA and has therapeutic potential for neurodegenerative diseases associated with BIA.





Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer’s disease
- ANOVA:
-
Analysis of variance
- BBB:
-
Blood–brain barrier
- BIA:
-
Brain iron accumulation
- CMC:
-
Carboxymethylcellulose
- DCF-DA:
-
2’,7’-Dichlorofluorescein diacetate
- DFO:
-
Deferoxamine
- DFP:
-
Deferiprone
- DMEM:
-
Dulbecco’s modified eagle’s medium
- DMPS:
-
Sodium 2,3-dimercaptopropanesulfonate monohydrate
- DMSO:
-
Dimethyl sulfoxide
- FAC:
-
Ferric ammonium citrate
- FBS:
-
Fetal bovine serum
- Fe2 + :
-
Ferrous iron
- Fe3 + :
-
Ferric iron
- FeCl3 :
-
Iron (III) chloride
- Hg:
-
Mercury
- MCH:
-
Mean corpuscular hemoglobin
- MCV:
-
Mean corpuscular volume
- MES:
-
2-(N-Morpholino) ethanesulfonic acid
- NBMI:
-
N,N’-Bis(2-mercaptoethyl)isophthalamide
- Pb:
-
Lead
- PD:
-
Parkinson’s disease
- RBC:
-
Red blood cell
- ROS:
-
Reactive oxygen species
- WBC:
-
White blood cell
- WT:
-
Wild type
References
Barnham KJ, Masters CL, Bush AI (2004) Neurodegenerative diseases and oxidative stress. Nat Rev Drug Discov, 3(3):205–214. https://doi.org/10.1038/nrd1330
Beard JL, Connor JR, Jones BC (1993) Iron in the brain. Nutr Rev, 51(6): 157–170. https://doi.org/10.1111/j.1753-4887.1993.tb03096.x
Chang J, Kueon C, Kim J (2014) Influence of lead on repetitive behavior and dopamine metabolism in a mouse model of iron overload. Toxicol Res, 30(4): 267–276. https://doi.org/10.5487/TR.2014.30.4.267
Clarke D, Buchanan R, Gupta N, Haley B (2012) Amelioration of acute mercury toxicity by a novel, non-toxic lipid soluble Chelator N, N’bis-(2-mercaptoethyl)isophthalamide: effect on animal survival, health, mercury excretion and organ accumulation. Toxicol Environ Chem 94(3):616–640. https://doi.org/10.1080/02772248.2012.657199
Cohen AR, Galanello R, Piga A, De Sanctis V, Tricta F (2003). Safety and effectiveness of long-term therapy with the oral iron chelator deferiprone. Blood, 102(5): 1583–1587. https://doi.org/10.1182/blood-2002-10-3280
Cui ZW, Xie ZX, Wang BF, Zhong ZH, Chen XY, Sun YH, Sun QF, Yang GY, Bian LG (2015) Carvacrol protects neuroblastoma SH-SY5Y cells against Fe(2+)-induced apoptosis by suppressing activation of MAPK/JNK-NF-κB signaling pathway. Acta Pharmacol Sin, 36(12): 1426–1436. https://doi.org/10.1038/aps.2015.90
Devos D, Moreau C, Devedjian JC, Kluza J, Petrault M, Laloux C, Jonneaux A, Ryckewaert G, Garcon G, Rouaix N, Duhamel A, Jissendi P, Dujardin K, Auger F, Ravasi L, Hopes L, Grolez G, Firdaus W, Sablonniere B, Strubi-Vuillaume I, Zahr N, Destee A, Corvol JC, Poltl D, Leist M, Rose C, Defebvre L, Marchetti P, Cabantchik ZI, Bordet R (2014). Targeting chelatable iron as a therapeutic modality in Parkinson's disease. Antioxid Redox Signal, 21(2): 195–210. https://doi.org/10.1089/ars.2013.5593
Diwakarla S, McQuade RM, Constable R, Artaiz O, Lei E, Barnham KJ, Adlard PA, Cherny RA, Di Natale MR, Wu H, Chai XY, Lawson VA, Finkelstein DI, Furness JB (2021). ATH434 Reverses colorectal dysfunction in the A53T Mouse Model of Parkinson's Disease. J Parkinsons Dis. https://doi.org/10.3233/JPD-212731
Dusek P, Schneider SA, Aaseth J (2016) Dec). Iron chelation in the treatment of neurodegenerative diseases. J Trace Elem Med Biol 38:81–92. https://doi.org/10.1016/j.jtemb.2016.03.010
Fawzi SF, Menze ET, Tadros MG (2020) Deferiprone ameliorates memory impairment in Scopolamine-treated rats: The impact of its iron-chelating effect on beta-amyloid disposition. Behav Brain Res, 378: 112314. https://doi.org/10.1016/j.bbr.2019.112314
Finkelstein DI, Billings JL, Adlard PA, Ayton S, Sedjahtera A, Masters CL, Wilkins S, Shackleford DM, Charman SA., Bal W, Zawisza IA, Kurowska E, Gundlach AL, Ma S, Bush AI, Hare DJ, Doble PA, Crawford S, Gautier EC, Parsons J, Huggins P, Barnham KJ, Cherny RA (2017) The novel compound PBT434 prevents iron mediated neurodegeneration and alpha-synuclein toxicity in multiple models of Parkinson's disease. Acta Neuropathol Commun, 5(1): 53. https://doi.org/10.1186/s40478-017-0456-2
Gadde R, Betharia S (2021) N,N'bis-(2-mercaptoethyl) isophthalamide (NBMI) exerts neuroprotection against lead-induced toxicity in U-87 MG cells. Arch Toxicol. https://doi.org/10.1007/s00204-021-03103-2
Gaeta A, Hider RC (2005) The crucial role of metal ions in neurodegeneration: the basis for a promising therapeutic strategy. Br J Pharmacol, 146(8): 1041–1059. https://doi.org/10.1038/sj.bjp.0706416
Galanello R, Campus S (2009) Deferiprone chelation therapy for thalassemia major. Acta Haematol 122(2–3):155–164. https://doi.org/10.1159/000243800
Grillo AS, SantaMaria AM, Kafina MD, Cioffi AG, Huston NC, Han M, Seo YA, Yien YY, Nardone C, Menon AV, Fan J, Svoboda DC, Anderson JB, Hong JD, Nicolau BG, Subedi K, Gewirth AA, Wessling-Resnick M, Kim J, Paw BH, Burke MD (2017) Restored iron transport by a small molecule promotes absorption and hemoglobinization in animals. Science, 356(6338): 608–616. https://doi.org/10.1126/science.aah3862
Guo C, Hao LJ, Yang ZH, Chai R, Zhang S, Gu Y, Gao HL, Zhong ML, Wang T, Li JY, Wang ZY (2016) Deferoxamine-mediated up-regulation of HIF-1alpha prevents dopaminergic neuronal death via the activation of MAPK family proteins in MPTP-treated mice. Exp Neurol 280:13–23. https://doi.org/10.1016/j.expneurol.2016.03.016
Halliwell B, Gutteridge JM (1988) Free radicals and antioxidant protection: mechanisms and significance in toxicology and disease. Hum Toxicol 7(1):7–13. https://doi.org/10.1177/096032718800700102
Hatcher HC, Singh RN, Torti FM, Torti SV (2009) Synthetic and natural iron chelators: therapeutic potential and clinical use. Future Med Chem 1(9):1643–1670. https://doi.org/10.4155/fmc.09.121
Heras-Garvin A, Refolo V, Schmidt C, Malfertheiner K, Wenning GK, Bradbury M, Stamler D, Stefanova N (2021) ATH434 Reduces α-Synuclein-Related Neurodegeneration in a Murine Model of Multiple System Atrophy. Mov Disord 36(11):2605–2614. https://doi.org/10.1002/mds.28714
Hoepken HH, Korten T, Robinson SR, Dringen R (2004) Iron accumulation, iron-mediated toxicity and altered levels of ferritin and transferrin receptor in cultured astrocytes during incubation with ferric ammonium citrate. J Neurochem 88(5):1194–1202. https://doi.org/10.1046/j.1471-4159.2003.02236.x
Ibrahim AS, Edwards JE Jr, Fu Y, Spellberg B (2006) Deferiprone iron chelation as a novel therapy for experimental mucormycosis. J Antimicrob Chemother 58(5):1070–1073. https://doi.org/10.1093/jac/dkl350
Jefferies WA, Brandon MR, Hunt SV, Williams AF, Gatter KC, Mason DY (1984) Transferrin receptor on endothelium of brain capillaries. Nature 312(5990):162–163. https://doi.org/10.1038/312162a0
Ke T, Bornhorst J, Schwerdtle T, Santamaria A, Soare FAA, Rocha JBT, Farina M, Bowman AB, Aschner M (2020) Therapeutic Efficacy of the N,N' Bis-(2-Mercaptoethyl) Isophthalamide Chelator for Methylmercury Intoxication in Caenorhabditis elegans. Neurotox Res, 38(1): 133–144. https://doi.org/10.1007/s12640-020-00194-0
Khodaverdian V, Tapadar S, MacDonald IA, Xu Y, Ho PY, Bridges A, Rajpurohit P, Sanghani BA, Fan Y, Thangaraju M, Hathaway NA, Oyelere AK (2019) Deferiprone: pan-selective histone lysine demethylase inhibition activity and structure activity relationship study. Sci Rep, 9(1): 4802. https://doi.org/10.1038/s41598-019-39214-1
Kolnagou A, Kontoghiorghe CN, Kontoghiorghes GJ (2014). Transition of Thalassaemia and Friedreich ataxia from fatal to chronic diseases. World J Methodol, 4(4): 197–218. https://doi.org/10.5662/wjm.v4.i4.197
Kontoghiorghes GJ, Kontoghiorghe CN (2020) Iron and chelation in biochemistry and medicine: new approaches to controlling iron metabolism and treating related diseases. Cells. https://doi.org/10.3390/cells9061456
Kruszewski M (2003) Labile iron pool: the main determinant of cellular response to oxidative stress. Mutat Res 531(1–2):81–92. https://doi.org/10.1016/j.mrfmmm.2003.08.004
Kuhn LC (2015) Iron regulatory proteins and their role in controlling iron metabolism. Metallomics 7(2):232–243. https://doi.org/10.1039/c4mt00164h
Li X, Jankovic J, Le W (2011) Iron chelation and neuroprotection in neurodegenerative diseases. J Neural Transm (Vienna) 118(3):473–477. https://doi.org/10.1007/s00702-010-0518-0
Mobarra N, Shanaki M, Ehteram H, Nasiri H, Sahmani M, Saeidi M, Goudarzi M, Pourkarim H, Azad M (2016) A review on iron chelators in treatment of iron overload syndromes. Int J Hematol Oncol Stem Cell Res 10(4):239–247
Molina-Holgado F, Gaeta A, Francis PT, Williams RJ, Hider RC (2008) Neuroprotective actions of deferiprone in cultured cortical neurones and SHSY-5Y cells. J Neurochem, 105(6): 2466–2476. https://doi.org/10.1111/j.1471-4159.2008.05332.x
Montuschi P, Barnes PJ, Roberts LJ, 2nd (2004) Isoprostanes: markers and mediators of oxidative stress. FASEB J, 18(15): 1791–1800. https://doi.org/10.1096/fj.04-2330rev
Nandar W, Connor JR (2011) HFE gene variants affect iron in the brain. J Nutr, 141(4): 729S-739S. https://doi.org/10.3945/jn.110.130351
Nandar W, Neely EB, Unger E, Connor JR (2013) A mutation in the HFE gene is associated with altered brain iron profiles and increased oxidative stress in mice. Biochim Biophys Acta, 1832(6): 729–741. https://doi.org/10.1016/j.bbadis.2013.02.009
Nunez MT, Chana-Cuevas P (2018) New Perspectives in Iron Chelation Therapy for the Treatment of Neurodegenerative Diseases. Pharmaceuticals (Basel), 11(4). https://doi.org/10.3390/ph11040109
Porter, J. B., Hoyes, K. P., Abeysinghe, R. D., Brooks, P. N., Huehns, E. R., & Hider, R. C. (1991, Nov 15). Comparison of the subacute toxicity and efficacy of 3-hydroxypyridin-4-one iron chelators in overloaded and nonoverloaded mice. Blood, 78(10), 2727–2734. https://www.ncbi.nlm.nih.gov/pubmed/1824264
Quintana C, Bellefqih S, Laval JY, Guerquin-Kern JL, Wu TD, Avila J, Ferrer I, Arranz R, Patino C (2006) Study of the localization of iron, ferritin, and hemosiderin in Alzheimer's disease hippocampus by analytical microscopy at the subcellular level. J Struct Biol, 153(1): 42–54. https://doi.org/10.1016/j.jsb.2005.11.001
Rakshit J, Mallick A, Roy S, Sarbajna A, Dutta M, Bandyopadhyay J (2020) Iron-induced apoptotic cell death and autophagy dysfunction in human neuroblastoma cell line SH-SY5Y. Biol Trace Elem Res, 193(1): 138–151. https://doi.org/10.1007/s12011-019-01679-6
Rao SS, Portbury SD, Lago L, Bush AI, Adlard PA (2020) The iron chelator deferiprone improves the phenotype in a mouse model of tauopathy. J Alzheimers Dis 78(4):1783. https://doi.org/10.3233/JAD-209009
Rogers JT, Venkataramani V, Washburn C, Liu Y, Tummala V, Jiang H, Smith A, Cahill CM (2016) A role for amyloid precursor protein translation to restore iron homeostasis and ameliorate lead (Pb) neurotoxicity. J Neurochem, 138(3), 479–494. https://doi.org/10.1111/jnc.13671
Salvador GA, Uranga RM, Giusto NM (2010). Iron and mechanisms of neurotoxicity. Int J Alzheimers Dis, 2011: 720658. https://doi.org/10.4061/2011/720658
Schutzmeier P, Focil Baquerizo A, Castillo-Tandazo W, Focil N, Bose-O'Reilly S (2018) Efficacy of N,N'bis-(2-mercaptoethyl) isophthalamide on mercury intoxication: a randomized controlled trial. Environ Health, 17(1):15. https://doi.org/10.1186/s12940-018-0358-1
Secor JD, Kotha SR, Gurney TO, Patel RB, Kefauver NR, Gupta N, Morris AJ, Haley BE, Parinandi NL (2011) Novel lipid-soluble thiol-redox antioxidant and heavy metal chelator, N,N'-bis(2-mercaptoethyl)isophthalamide (NBMI) and phospholipase D-specific inhibitor, 5-fluoro-2-indolyl des-chlorohalopemide (FIPI) attenuate mercury-induced lipid signaling leading to protection against cytotoxicity in aortic endothelial cells. Int J Toxicol, 30(6): 619–638. https://doi.org/10.1177/1091581811422413
Shi L, Huang C, Luo Q, Rogers E, Xia Y, Liu W, Ma W, Zeng W, Gong L, Fang J, Tang L, Cheng A, Shi R, Chen Z (2019) The association of iron and the pathologies of parkinson’s diseases in MPTP/MPP(+)-induced neuronal degeneration in non-human primates and in cell culture. Front Aging Neurosci 11:215. https://doi.org/10.3389/fnagi.2019.00215
Sripetchwandee J, Khamseekaew J, Svasti S, Srichairatanakool S, Fucharoen S, Chattipakorn N, Chattipakorn SC (2019) Deferiprone and efonidipine mitigated iron-overload induced neurotoxicity in wild-type and thalassemic mice. Life Sci, 239: 116878. https://doi.org/10.1016/j.lfs.2019.116878
Tenopoulou M, Kurz T, Doulias PT, Galaris D, Brunk UT (2007) Does the calcein-AM method assay the total cellular 'labile iron pool' or only a fraction of it? Biochem J, 403(2): 261–266. https://doi.org/10.1042/BJ20061840
Torrance JD, Bothwell TH (1968) A simple technique for measuring storage iron concentrations in formalinised liver samples. S Afr J Med Sci, 33(1), 9–11. https://www.ncbi.nlm.nih.gov/pubmed/5676884
Ye Q, Kim J (2016) Mutation in HFE gene decreases manganese accumulation and oxidative stress in the brain after olfactory manganese exposure. Metallomics, 8(6): 618–627. https://doi.org/10.1039/c6mt00080k
Ye Q, Trivedi M, Zhang Y, Bohlke M, Alsulimani H, Chang J, Maher T, Deth R, Kim J (2019) Brain iron loading impairs DNA methylation and alters GABAergic function in mice. FASEB J, 33(2): 2460–2471. https://doi.org/10.1096/fj.201801116RR
Zaman KM, Blue LY, Huggins FE, Atwood DA (2007) Cd, Hg, and Pb Compounds of Benzene-1,3-diamidoethanethiol (BDETH(2)). Inorg Chem, 46(6): 1975–1980. https://doi.org/10.1021/ic0607639
Zecca L, Youdim MB, Riederer P, Connor JR, Crichton RR (2004) Iron, brain ageing and neurodegenerative disorders. Nat Rev Neurosci, 5(11): 863–873. https://doi.org/10.1038/nrn1537
Zecca L, Berg D, Arzberger T, Ruprecht P, Rausch WD, Musicco M, Tampellini D, Riederer P, Gerlach M, Becker G (2005) In vivo detection of iron and neuromelanin by transcranial sonography: a new approach for early detection of substantia nigra damage. Mov Disord, 20(10), 1278–1285. https://doi.org/10.1002/mds.20550
Acknowledgements
The authors are grateful to EmeraMed (Nicholasville, KY) for providing NBMI and reagents, to Dr. Haley Boyd and Dr. Kuljeet Gugnani for helpful discussions, to Ms. Lingxue Zeng and Mr. Sonny Farfan for help during animal experiments, and to Ms. Analucia Gonzales Urday and Mr. Shrey Shah for quantification of calcein-AM images.
Funding
This work was supported in part by EmeraMed.
Author information
Authors and Affiliations
Contributions
RC, RG, YF, SB, and JK designed research; RC, RG, YF, NK, NS, and KB performed research; RC, RG, YF, SB, and JK analyzed data; RC prepared the original draft; RG, SB, and JK reviewed and edited the manuscript; HSC, SB, and JK provided necessary lab space and reagents for research.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheng, R., Gadde, R., Fan, Y. et al. Reversal of genetic brain iron accumulation by N,N′-bis(2-mercaptoethyl)isophthalamide, a lipophilic metal chelator, in mice. Arch Toxicol 96, 1951–1962 (2022). https://doi.org/10.1007/s00204-022-03287-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-022-03287-1