Abstract
Pseudomonas and Burkholderia pose a significant health threat to people with chronic respiratory conditions; the resistance inherent in these bacteria indicates that new antimicrobial strategies are required. Susceptibility of 56 strains of P. aeruginosa and 55 strains of Burkholderia to manuka honey, tobramycin and colistin using microbroth dilution and E strip was determined. MICs of antibiotics with honey were determined to search for synergistic combinations against two representative strains of each genus. All strains exhibited susceptibility to honey ≤10 % (w/v); mean susceptibility of Burkholderia (4.6 % w/v) was lower than P. aeruginosa (7.3 % w/v). Synergistic or additive combinations were found with all four strains tested. Combinations of manuka honey with antibiotics can be used to lower the MIC need to successfully inhibit both P. aeruginosa and B. cepacia. The use of honey as a combination agent may be possible for the management of P. aeruginosa and B. cepacia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pseudomonas aeruginosa and Burkholderia spp. are important opportunist bacteria that can cause serious and chronic respiratory infections in vulnerable patients, especially those with underlying conditions such as cystic fibrosis or chronic granulomatous disease (Lyczak et al. 2000; Vanlaere et al. 2009). They have also been implicated in wound infections (Alvarez-Lerma et al. 2008; Bassett et al. 1970). The switch from non-mucoid to mucoid variants accompanies complex changes in motility and biofilm formation that have been shown to facilitate the persistence of each of these bacteria in lungs. Chronic colonisation of the lungs of cystic fibrosis patients by mucoid strains of P. aeruginosa and Burkholderia is associated with deteriorating lung function which results in a poor prognosis (Hancock 1998; Nicas and Hancock 1983).
Increasingly, the tendency of pathogenic bacteria to acquire resistance to conventional antibiotics is limiting treatment plans, and new strategies of antimicrobial treatment are being sought. In comparison with other bacteria, the low permeability of the outer membrane of P. aeruginosa restricts penetration of antibiotics into the bacterium (Hancock 1998); this membrane is 12–100 times less permeable than that of E. coli (Nicas and Hancock 1983). As a result of this intrinsic mechanism, P. aeruginosa can exhibit high baseline decreased susceptibility to many antibiotics. Increasingly, gene mutation and gene acquisition confer resistance to a range of antibiotics that includes β-lactams, aminoglycosides and fluoroquinolones, making these strains more difficult to inhibit.
Burkholderia strains are also inherently resistant to many available antibiotics (Mahenthiralingam et al. 2005). It has been demonstrated that some strains utilise penicillin as a sole carbon source (Vermis et al. 2003) and that others survive in solutions of the hospital disinfectant, chlorhexidine (Heo et al. 2008). Some of this recalcitrance may be due to their wide distribution throughout the environment; they have been isolated from soil, water, insects and plants, as well as from humans, where they will have been exposed to many antimicrobial compounds (Compant et al. 2008).
Both of these notoriously resistant bacteria are prolific biofilm formers, especially in cystic fibrosis patients where up to 1000 times the concentration of antibiotic is needed than to kill the equivalent planktonic cell (Mah and O’Toole 2001). Added to the natural resistance of these bacteria, this makes these tenacious bacteria a real therapeutic challenge. New strategies are needed to treat for cystic fibrosis pulmonary infection (McCaughey et al. 2013).
Susceptibility to manuka honey of 22 strains of B. cepacia (Cooper et al. 2000) and of 17 strains of P. aeruginosa isolated from burns (Cooper et al. 2002) has been demonstrated using raw non-medical-grade (non-sterilised) honey samples. Gamma-irradiated sterile medical-grade honey is now available, and it is this which is now utilised for both medical research and in licensed wound dressings applied within wound care. Recently, manuka honey has been shown to enhance the activity of antibiotics (Jenkins and Cooper 2010, 2012; Muller et al. 2013). Currently, the susceptibility to manuka honey of clinical strains of P. aeruginosa and B. cepacia isolated from cystic fibrosis patients and the potential for synergistic activity in combinations of antibiotics and honey against these strains is unknown. This study, therefore, was designed to determine the susceptibility of clinical isolates to medical-grade honey and also to look at the potential for honey in combination with antibiotics used in this field.
Materials and methods
Test bacteria and honey
Clinical isolates of P. aeruginosa and B. cepacia collected from a range of infections were submitted to the Specialist Antimicrobial Chemotherapy Unit, Cardiff in the UK. Of the isolates tested here, 56 were identified as P. aeruginosa and 55 as Burkholderia species by standard bacteriological techniques (Table 1). These cultures were stored in −80 °C on beads and cultured on Columbia agar containing horse blood before testing.
The sterile medical-grade manuka honey used here was Comvita manukacare 18+ ; it was a gift from Comvita UK.
Microbroth dilution
The minimum inhibitory concentration for manuka honey, colistin and tobramycin was determined by using the standard CLSI broth microdilution method with Mueller–Hinton broth (MHB). A serial doubling dilution was used for the antibiotics, but the MIC of the sample of honey was used at 1 % (w/v) increments from 0 to 10 % (w/v). Inocula were prepared from direct colony suspension, and microtitre plates were inoculated with 105 CFU/ml. Plates were incubated in air at 37 °C for 18 h. The MIC was defined as the lowest concentration of the antimicrobial that prevents visible growth of a microorganism in a broth dilution susceptibility test.
Synergy
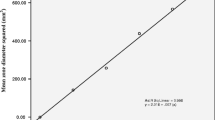
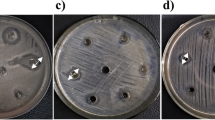
Experiments were undertaken to determine the potential of honey in combination with currently used antibiotics to exhibit synergistic activity. Two representative isolates of each of P. aeruginosa and B. cepacia were chosen for this further investigation, and interactions between manuka honey and each of two antibiotics (colistin and tobramycin) were tested. Microbroth dilution was conducted as above using honey at 1 % (w/v) below the MIC with a range of antibiotic concentrations. These combinations were also tested by E strips by the inclusion of honey at 1 % (w/v) below the MIC into Muller Hinton agar (MHA) or MHA alone.
Fractional inhibition concentration (FIC) was calculated for each combination using the following formula:
The FIC values have been interpreted to indicate synergism (≤0.5), additivity (>0.5 to ≤4) or antagonism (>4) according to published recommendations (Carmeli et al. 1999; Odds 2003).
Results
Susceptibility of respiratory isolates to manuka honey
Using the standard CLSI microbroth dilution method, susceptibility to manuka honey was determined for 111 clinical isolates of P. aeruginosa and B. cepacia obtained from cystic fibrosis patients. The 56 isolates of P. aeruginosa exhibited an MIC of ≤10 % (w/v), and the 55 Burkholderia isolates exhibited an MIC of ≤7 % (w/v) (Table 1); mean MICs were 7.3 and 4.7 % (w/v) for P. aeruginosa and B. cepacia, respectively. Hence, B. cepacia demonstrated a higher susceptibility to manuka honey than P. aeruginosa; conversely, B. cepacia has been shown to be more resistant to antibiotics than P. aeruginosa (Wilkinson and Pitt 1995).
Synergy between manuka honey and antibiotics
Using two representative strains of each of P. aeruginosa and B. cepacia, synergistic combinations of honey and either colistin or tobramycin were investigated using broth dilution and E strips. No antagonism was seen with any of the combinations tested. Synergy was established between colistin and honey for both P. aeruginosa isolates (Tables 2) and one of the B. cepacia isolates (Table 3). Synergy was also observed for tobramycin and honey against one of the P. aeruginosa species. All other combinations showed additivity with values ≤1. Despite some variation between MICs derived by different methods, FIC values were largely consistent (Tables 2, 3) .
Discussion
Tobramycin and colistin were chosen for the synergy studies here because they are licensed for use as inhaled antibiotics in treating chronic respiratory infections in cystic fibrosis. The use of inhaled drugs for treatment of respiratory infections is relatively new. Within the last 30 years, drugs that were originally designed for oral and intravenous application have been reformulated for inhalation; novel inhaled compounds such as gallium are also in development (Hofmann 2012). It is possible that honey combined with selected antibiotics could be developed into an inhalation compound for use in patients with respiratory infections. Combinations of antibiotics with non-antibiotic substances can enhance the efficacy of a number of currently used antibiotics forming syncretic combinations (Ejim et al. 2011; Garo et al. 2007). Additionally, combination therapy has been promoted as a strategy for reducing the emergence of antibiotic resistant bacteria and decreasing the likelihood that organisms exposed to them will survive. Already, manuka honey has been shown not to select for resistance (Cooper et al. 2010).
The findings above are consistent with data obtained in previous studies with raw manuka honey (Cooper et al. 2000, 2002), and it is important that the susceptibility of respiratory isolates to honey did not differ markedly from that of wound isolates. As discussed above, P. aeruginosa and B. cepacia are both potentially pathogenic bacteria with innate resistance to antibiotics. Incidence of multidrug resistance in these species other than respiratory conditions such as cystic fibrosis is not common, and in some cases, these infections can be cleared effectively. However, in complex and chronic infections, such as those seen in respiratory disorders, these bacteria can become highly tolerant to antibiotics and progressively more difficult to treat. As a consequence of this decreased susceptibility to individual antibiotics and to combinations of antibiotics, it has become ever more important to find new or complementary antibacterial agents to augment currently available drug regimes.
Compounding the problem of innate antibiotic resistance in these bacteria is their ability to establish microcolonies embedded in mucoid extracellular polymeric substances, otherwise known as biofilm. This is a particular problem in cases of cystic fibrosis. Such structures require the utilisation of high concentrations of antibiotic for inhibitory concentrations to be reached throughout the biofilm. Antibiotics delivered to cells within the biofilm at levels below the MIC due to inefficient diffusion through biofilms have been shown to induce growth of biofilm, specifically with tobramycin and P. aeruginosa (Linares et al. 2006). Use of sub-inhibitory antibiotics can also lead to increased resistance (Wu et al. 2009).
P. aeruginosa and B. cepacia are frequently associated with cystic fibrosis and hospital-acquired pneumonias which are associated with high morbidity and mortality. Poor control of these bacteria impacts on treatment times, increases risk of cross-infection and increases risk of long-term carriage in patients (Aloush et al. 2006; Chou 2006). Previously, studies have suggested that natural compounds combined with antibiotics could be a new strategy for combating infections and here it is apparent that honey could be a compound worthy of further investigation. Laboratory studies have also begun to report the susceptibility of biofilms of P. aeruginosa to manuka honey (Maddocks et al. 2013; Cooper et al. 2014), and the next logical step would be to evaluate the efficacy of combinations of honey and antibiotics on biofilms.
Conclusions
The data presented here indicate that manuka honey at relatively low concentrations inhibits the growth of clinical cystic fibrosis isolates of both P. aeruginosa and B. cepacia and acts synergistically with two pertinent antibiotics. We believe that manuka honey may have a role to play in the management of cystic fibrosis patients with chronic respiratory infections, and in the future, we intend to investigate the activity of honey with a much larger range of bacteria and antibiotic combinations and to determine the susceptibilities of biofilms, as well as suspension cultures. Clinical studies will also be needed to determine the potential and efficacy of antibiotic and honey combinations for cystic fibrosis patients.
References
Aloush V, Navon-Senezia S, Seigman-Igra Y, Cabili Y, Carmeli Y (2006) Multidrug-resistant Pseudomonas aeruginosa: risk factors and clinical impact. Antimicrob Agents Chemother 50:43–48. doi:10.1128/AAC.50.1.43-48.2006
Alvarez-Lerma F, Maull E, Terradas R, Sequra C, Planells I, Coll P et al (2008) Moisturizing body milk as a reservoir of Burkholderia cepacia: outbreak of nosocomial infection in a multidisciplinary intensive care unit. Crit Care 12:R10. doi:10.1186/cc6778
Bassett DC, Stokes KJ, Thomas WR (1970) Wound infection with Pseudomonas multivorans: a water-borne contaminant of disinfectant solutions. Lancet 1:1188–1191. doi:10.1016/S0140-6736(70)91783-6
Carmeli Y, Troillet N, Karchmer AW, Samore MH (1999) Health and economic outcomes of antibiotic resistance in Pseudomonas aeruginosa. Arch Intern Med 159:1127–1132. doi:10.1001/archinte.159.10.1127
Chou TC (2006) Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol Rev 58:621–681. doi:10.1124/pr.58.3.10
Compant S, Nowak J, Coenye T, Clement C, Barka EA (2008) Diversity and occurrence of Burkholderia spp. in the natural environment. FEMS Microbiol Rev 32:607–626. doi:10.1111/j.1574-6976.2008.00113.x
Cooper RA, Wigley P, Burton NF (2000) Susceptibility of multiresistant strains of Burkholderia cepacia to honey. Lett Appl Microbiol 31:20–24. doi:10.1046/j.1472-765x.2000.00756.x
Cooper RA, Halas E, Molan PC (2002) The efficacy of honey in inhibiting strains of Pseudomonas aeruginosa from infected burns. J Burn Care Rehabil 23:366–370. doi:10.1097/01.BCR.0000036453.98917.41
Cooper RA, Jenkins L, Henriques AF, Duggan RS, Burton NF (2010) Absence of bacterial resistance to medical-grade manuka honey. Eur J Clin Microbiol Infect Dis 29:1237–1241. doi:10.1007/s10096-010-0992-1
Cooper RA, Jenkins L, Hooper S (2014) Inhibition of biofilms of Pseudomonas aeruginosa by Medihoney in vitro. J Wound Care 23:93–104
Ejim L, Farha MA, Falconer SB, Wildenhain J, Coombes BK, Tyers M et al (2011) Combinations of antibiotics and nonantibiotic drugs enhance antimicrobial efficacy. Nat Chem Biol 7:248–350. doi:10.1038/nchembio.559
Garo E, Eldridge GR, Goering MG, DeLancey PE, Hamilton MA, Costerton JW et al (2007) Asiatic acid and corosolic acid enhance the susceptibility of Pseudomonas aeruginosa biofilms to tobramycin. Antimicrob Agents Chemother 51:1813–1817. doi:10.1128/AAC.01037-06
Hancock REW (1998) Resistance mechanisms in Pseudomonas aeruginosa and other nonfermentative gram-negative bacteria. Clin Infect Dis 27:S93–S99. doi:10.1086/514909
Heo ST, Kim SJ, Jeong YG, Bae I, Jin JS, Lee JC (2008) Hospital outbreak of Burkholderia stabilis bacteraemia related to contaminated chlorhexidine in haemotalogical malignancy patients with indwelling catheters. J Hosp Infect 7:241–245. doi:10.1016/j.jhin.2008.07.019
Hofmann H (2012) New developments in inhaled antibiotics for the treatment of Pseudomonas aeruginosa. Curr Pharm Des 18:683–695. doi:10.2174/138161212799315975
Jenkins R, Cooper R (2010) Synergy between oxacillin and manuka honey sensitises methicillin-resistant Staphylococcus aureus to oxacillin. J Antimicrob Chem 76:1405–1407. doi:10.1093/jac/dks071
Jenkins R, Cooper RA (2012) Improving antibiotic activity against wound pathogens with manuka honey in vitro. PLoS One 7:e45600. doi:10.1371/journal.pone.0045600
Linares JF, Gustaffsson I, Baquero F, Martinez J (2006) Antibiotics as intermicrobial signalling agents instead of weapons. Proc Natl Acad Sci USA 103:19484–19489
Lyczak JB, Cannon CL, Pier GB (2000) Establishment of Pseudomonas aeruginosa infection: lessons from a versatile opportunist. Microbes Infect 2:1051–1060. doi:10.1016/S1286-4579(00)01259-4
Maddocks SE, Jenkins RE, Rowlands RS, Purdy KJ, Cooper RA (2013) Manuka honey inhibits adhesion and invasion of medically important wound bacteria in vitro. Future Microbiol 8:1523–1536. doi:10.2217/fmb.13.126
Mah TF, O’Toole GA (2001) Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol 9:34–39. doi:10.1016/S0966-842X(00)01913-2
Mahenthiralingam E, Urban TA, Goldberg JB (2005) The multifarious, multireplicon Burkholderia cepacia complex. Nat Rev Microbiol 3:144–156. doi:10.1038/nrmicro1085
McCaughey G, Gilpin D, Elborn J, Tunney MM (2013) The future of antimicrobial therapy in the era of antibiotic resistance in cystic fibrosis pulmonary infection. Expert Rev Respir Med 7:385–396. doi:10.1586/17476348.2013.814411
Muller G, Alber DG, Turnbull L, Schlothauer RC, Carter DA, Whitchurch CB et al (2013) Synergism between Medihoney and rifampicin against methicillin-resistant Staphylococcus aureus (MRSA). PLoS One 8(2):e57679. doi:10.1371/journal.pone.0057679
Nicas TI, Hancock REW (1983) Pseudomonas aeruginosa outer membrane permeability: isolation of a porin protein F-deficient mutant. J Bacteriol 153:281–285
Odds F (2003) Synergy, antagonism, and what the chequerboard puts between them. J Antimicrob Chemother 52:1. doi:10.1093/jac/dkg301
Vanlaere E, Baldwin A, Gevers D, Henry D, De Brandt E, LiPuma JJ et al (2009) Taxon K, a complex within the Burkholderia cepacia complex, comprises at least two novel species, Burkholderia contaminans sp. nov. and Burkholderia lata sp. nov. Int J Syst Evol Microbiol 59:102–111. doi:10.1099/ijs.0.001123-0
Vermis K, Vandamme PAR, Nelis HJ (2003) Burkholderia cepacia complex genomovars: utilization of carbon sources, susceptibility to antimicrobial agents and growth on selective media. J Appl Microbiol 95:1191–1199. doi:10.1046/j.1365-2672.2003.02054.x
Wilkinson SG, Pitt TL (1995) Burkholderia (Pseudomonas) cepacia: pathogenicity and resistance. Rev Med Microbiol 6:10–17
Wu YL, Scott EM, Po ALW, Tariq N (2009) Development of resistance and cross-resistance in Pseudomonas aeruginosa exposed to subinhibitory antibiotic concentrations. APMIS 107:585–592. doi:10.1111/j.1699-0463.1999.tb01596.x
Acknowledgments
The work was funded by The Waterloo Foundation and The Sir Halley Stewart Trust.
Conflict of interest
The authors have no conflict of interests to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Erko Stackebrandt.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Jenkins, R., Wootton, M., Howe, R. et al. A demonstration of the susceptibility of clinical isolates obtained from cystic fibrosis patients to manuka honey. Arch Microbiol 197, 597–601 (2015). https://doi.org/10.1007/s00203-015-1091-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00203-015-1091-6