Abstract
Summary
Oslo in Norway has had the highest incidence of hip fractures in the world. The incidence in Oslo has been thoroughly described every decade since the late 1970s. The incidence in Oslo has previously been higher compared to the rest of Norway but has now decreased to a level below the country average.
Purpose
The purpose of this study was to report the incidence of hip fractures in Oslo in 2019 and compare it with the incidence rates from the previous four decades.
Methods
Patients residing in Oslo in 2019 with a new hip fracture identified by searching the Oslo hospital’s patient administrative systems and protocols from the operating theaters. The diagnosis was verified through medical records and/or radiographs. To compare with previous studies, the direct standardization method was used with the population of Oslo in 2019 as the standard.
Results
A total of 758 hip fractures, 70% women, were identified in 2019. The age-standardized incidence rates per 10,000 person-years in 2019 (95% CI) were 45 (41.1–48.8) for women and 30 (25.8–33.8) for men. In women, there has been a continuous decline in age-standardized rates the last three decades and in men the last two decades. The most pronounced decline was seen in the oldest age groups over 70 years. There has been a secular decline in both cervical and trochanteric fractures; however, the decrease in trochanteric fractures was most distinct for males, with more than two times higher risk in 1996/1997 compared to 2019.
Conclusion
Incidence rates for hip fractures in Oslo in 2019 were the lowest rate reported since 1978. The decrease was significant for both men and women. For the first time, the incidence rates are below the national rates of Norway. However, the rates are still among the highest worldwide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Scandinavian countries (Norway, Sweden, Denmark) have the highest registered incidence rates for hip fractures in the world [1,2,3]. Even though the incidence of hip fractures in general is high in Norway, particularly high rates have been registered in the capital of Norway, Oslo, over decades [3,4,5,6]. Hip fractures in Oslo have been reported to occur at rates up to one-third higher than in rural districts of Norway [7]. Although the incidence of hip fractures is decreasing in most Western countries, the total number of fractures is expected to increase due to an aging population in the years to come [2].
Each year approximately 9000 people suffer a hip fracture in Norway [8]. Hip fractures are considered the most severe osteoporotic fracture. The risk of hip fractures increases exponentially with age and may have major consequences for frail elderly persons [2, 9]. The 1-year mortality rate after hip fractures in Norway is 25% [10]. Half of all hip fracture patients will not return to their pre-fracture function [11]. There are two main types of hip fractures, in the cervical or the trochanteric region of the femur. Individuals sustaining a cervical hip fracture are typically healthier and younger and have a higher physical function prior to the fracture compared to individuals with a trochanteric fracture [12]. Patients with a trochanteric fracture are often frailer with lower body mass density and with an increased risk of falling, and require longer recovery compared to individuals with cervical fracture [12].
Hip fractures, along with stroke and myocardial infarction, serve as healthcare quality indicators in Norwegian hospitals due to their high incidence and elevated risk of death [13]. The societal costs following a hip fracture are substantial, with nearly half of the expenses attributed to rehabilitation and care within the first year post-fracture [14]. Hence, reporting secular trends in high-risk diagnosis, such as hip fractures, is crucial for the maintenance of an effective healthcare system [9, 15].
The incidence of hip fractures in Oslo has been reported with the same thorough method every decade since the late 1970s [3,4,5, 7]. In addition, the proportion of cervical and trochanteric hip fractures has been registered for all previous studies. In 1988/1989, the incidence rate was at the highest level, before a decline was seen in 2007 [3, 5]. However, compared with other geographical areas in Norway and other countries, the incidence rate in Oslo remains the highest [3, 5].
In this study, we aimed to investigate the current incidence of hip fractures in Oslo and compare it to the rates over the last four decades. In addition to the rates in other geographical areas.
Methods
Study population
To report the hip fracture incidence in Oslo in 2019, all patients residing in Oslo (around 680,000 inhabitants) with a new hip fracture were identified from the 1st of January to the 31st of December 2019. Fractures with ICD-10 codes S72.0 (cervical fracture) and S72.1 (trochanteric fracture) were identified using patient administrative systems/electronic diagnosis registers. In addition, lists from the operating theaters in all three hospitals in Oslo treating hip fractures were reviewed. Also, related diagnoses in other parts of the femur as well as unspecified diagnoses in the lower limb (S72.2, S72.7, S72.9, T02.3, T02.5, T02.6-T02.9, and T12) were used to identify patients with potential incorrect diagnosis. The hip fracture diagnosis was verified through medical records. If the diagnosis were not clarified by the records, the patients’ radiographs were examined for verification. Patients with a fracture in both hips in the period had each fracture registered separately.
Patients transferred between hospitals were only registered once, at the hospital where the surgery was performed. Patients residing in Oslo, but who had a hip fracture and surgery outside of Oslo, were captured either when they were transferred to their local hospital in Oslo postoperatively. Or if they were discharged directly to home, they were identified at the follow-up at their local hospital in Oslo, which is standard practice. Therefore, we most probably have included nearly all hip fracture cases in our area in the period.
Background information collected from the medical record included age, sex, weight, height, place of trauma, fracture site, type of fracture, and perioperative information, such as time to surgery and type of surgery, history of hip fractures, and use of anti-osteoporosis drugs (AOD) prior to and after a fracture. Previous hip fractures were found by examining radiographs and the patients’ medical records. If a previous hip fracture was not visible on radiographs or not documented in the medical records in the past 5 years, they were not recorded. AOD was defined as oral bisphosphonates, zoledronate, denosumab, or teriparatide which are the registered drugs for use in Norway.
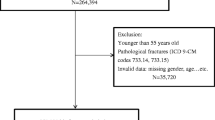
To be able to compare the incidence in 2019 with the previous years, patients with a subtrochanteric fracture (S72.2) were excluded, as in the previous studies. As in the previous studies, fractures due to cancer metastasis, periprosthetic fractures, and patients with registered home address outside of Oslo were also excluded. Patients who were registered with an incorrect hip fracture diagnosis were mostly due to secondary admissions for an already registered hip fracture (Fig supl).
Immigration status was received from Statistics Norway (SSB).
Historical and international comparison
The population of Oslo on the 1st of January 2019 was used as the standard population for the historical and national comparison and was provided by Statistics Norway (SSB) [16]. Age- and sex-specific incidence rates from the four previous studies were used to determine age-standardized incidence rates for hip fractures in Oslo in 2019, 2007 [5], 1996/1997 [3], 1988/1989 [7], and 1978/1979 [4]. Data from a study on hip fracture incidence in the total Norwegian population was used for the national comparison [8]. To compare the age- and sex-standardized incidence rate in Oslo with other geographical areas, we used the 2020 United Nations world population as the standard population [17]. As most other studies on hip fracture incidence included subtrochanteric hip fractures (S72.2), we included this group in our data (n = 37) for the analysis comparing the incidence rate in Oslo with other geographical areas.
Statistics
A two-sample Student t-test was used for comparisons of continuous outcomes. A chi-square test was used to compare categorical outcomes. The sex-specific age-standardized fracture rates were calculated by using the direct method of standardization to the population of Oslo on the 1st of January 2019. Age was divided into 10-year age groups up to 50 years, and 5-year age groups above 50. Incidence rate ratio (IRR) was calculated by Poisson regression. The level of statistical significance was set at 0.05. The results are given as mean (95% confidence interval (CI)). Age was given as median with interquartile range.
Analysis was conducted using Stata SE (Version 17, Stata Inc. College Station, TX, USA).
Ethics and approvals
The study was approved by the Regional Ethical Committee for Medical Research Ethics for South-Eastern Norway (reference number 2018/2235) and the Data Protection Officer at each of the hospitals. For this type of study, patient consent is not required. The study has adhered to the STROBE guidelines and has been performed in accordance with the Declaration of Helsinki.
Results
Patient characteristics
In 2019, a total number of 758 hip fractures were identified in 745 patients residing in Oslo (Fig supl) as 13 patients (12 women) had a fracture in both hips. Of the patients, 70% were women (n = 529). The median age was 84 years (IQR 75;89) in women, and 79 years (IQR 70;86) in men. There was an approximately equal number of fractures in the left and right hip, and 446 of the fractures were cervical (59%) and 312 trochanteric (41%), p < 0.001. According to the review of the medical records, 84 patients (11%) had sustained a contralateral hip fracture before 2019 (12.5% in women and 8% in men).
Incidence rates
The age-specific incidence rate for 2019 increased exponentially with age for both sexes and the incidence was higher for females compared with males in all age groups, except in the lowest age groups (Table 1). The number of cervical fractures was higher than trochanteric fractures in nearly all age groups and for both sexes, with a higher ratio in older males compared to older females.
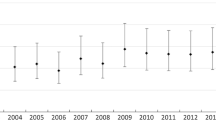
The age-standardized incidence rate for females and males above 50 years declined significantly between 2007 and 2019 (Table 2). There was a 28% and 52% higher risk of a hip fracture for females and males in 2007 compared to 2019. Compared to 2019, the incidence rate was 84% higher in 1988/1989 when the highest level was recorded for females (Table 2). The incidence rate ratio (IRR) was significantly higher in all previous years compared to 2019 for both sexes (Table 2). The age-specific incidence rate for 2019 compared to 2007 was most pronounced in the oldest age groups above 70 years for both females and males (Fig. 1).
The historical comparisons showed a secular decline in the incidence of both cervical and trochanteric fractures with the lowest in 2019 (Table 3). In women, there were somewhat similar changes over time for cervical and trochanteric fractures. However, in men, the changes were more pronounced for trochanteric compared to cervical fractures (Table 3). For example, in men, the IRR was 1.87 for trochanteric fracture and 1.34 for cervical fracture in 2007 compared to 2019.
In the comparison between Oslo and Norway as a whole, the age-standardized hip fracture incidence rate in 2019 (including both cervical, trochanteric, and subtrochanteric fracture) was 8% lower in Oslo compared to Norway for females (47.5 (43.4–51.4) versus 51.5 (52.2–52.8)), and 16% lower for males (30.3 (26.4–34.3) versus 36.2 (34.9–37.5)).
Other descriptives
Almost all hip fractures (95%) occurred due to low energy trauma. Seventy-three percent of the fractures happened indoors, of which 42.5% occurred at home, 23% in nursing homes or other care facilities, and 7.5% in other indoor areas. Twenty-four percent of the fractures were due to a fall outdoors and 3% had no registered site of trauma. Prior to the fracture, 53% of the patients were home dwelling without any assistance, 23% with assistance, 4.5% in short term care facilities, and 18% in permanent nursing homes. Patients with a trochanteric fracture were more likely to live in a permanent nursing home (22%) versus patients with a cervical fracture (14%). Most patients were operated at Diakonhjemmet Hospital (57%), 28% at Oslo University Hospital and 9% at Akershus University Hospital. Four percent were operated outside of Oslo. Prior to the fracture, 9.7% used or had used AOD. However, it was not specified when or for how long the patients had been using AOD. During the hospital stay, 48% of the patients started AOD after the hip fracture. Twenty-one percent did not receive AOD due to medical reasons. Patients were more likely to get AOD if they were operated at Oslo University Hospital (58% versus 39% at Akershus University Hospital and 44% at Diakonhjemmet Hospital). The majority of the patients (96%) received an infusion with zoledronate combined with 100,000 IE of vitamin D3 in the hospital. Twenty-four percent of the patients with a contralateral fracture had been treated with AOD prior to the subsequent fracture.
Influence of immigration
Only 7% of the patients sustaining a hip fracture had immigration background, while two percent were born in Norway with one or two parents with immigrant background. Almost all with immigration background were from a European country (5%), followed by Asia (1.6%). Ninety-three percent of the patients were born in Norway. In contrast, 20% of the females and 25% of the males in the total population of Oslo 50 years or older were immigrants or had one or two parents with immigrant background in 2019 [16].
Discussion
There has been a large reduction in the incidence of hip fractures in Oslo from 2007 to 2019. The incidence of hip fractures in Oslo, despite the large decline, remains higher than in most other populations. However, we found that hip fracture rates were lower than the Norwegian average. This contrasts with previous findings where the incidence in Oslo was higher than in the rest of the country [6, 8]. A systematic review found a higher incidence of hip fractures in urban areas, suggesting differences in lifestyle between cities and rural areas [18]. Furthermore, Norway’s elongated geography, characterized by its extensive coastline, seems to influence the incidence. Notably, regions near the coastline and in the northern districts exhibit the lowest incidence of hip fractures [6, 7]. A study on hip fracture incidence in Norway between 2002 and 2013 found that regional differences were smaller than earlier [6]. However, there was still a 17% higher incidence of hip fractures in Oslo compared to the district in Norway with the lowest registered rate [6]. This seems to have changed over the last decade. When comparing the results from 2019 in Oslo with Norway using Oslo as the standard population, the incidence of hip fractures was 8 and 16% lower in Oslo for females and males. However, reasons for the larger decline in Oslo in contrast to the rest of the country have not been investigated in this study.
The incidence of hip fractures has been higher in the Scandinavian countries compared to the rest of the world for several decades [2, 9]. The reason for this is not fully understood, but it is likely to be multifactorial, including genetics [19]. Even though the winter in Oslo is long, most hip fracture patients fell indoors, and Lofthus [3] did not find any seasonal changes in her study from 1996/1997. Other studies, however, saw a trend toward higher incidences in the winter [19,20,21]. The decreasing trend in hip fractures observed in the last decade has also been noted in other Western countries [9, 22, 23]. This decline has been evident across both genders and all age groups, with the biggest decrease observed in the population aged 70 and above [22]. To compare the incidence rates in Oslo to other geographical areas, we age- and sex-standardized our data to the United Nations World population of 2020, the same reference group used by Sing et al. in a global incidence study on hip fractures [9, 17]. We calculated the incidence rate per 100,000 person-years for men and women combined in Oslo to be 314 in 2019. Compared to the countries with the highest registered incidence rates from Sing et al. [9], Denmark and Singapore with age- and sex-standardized incidence rates of 258 and 260 in 2018, respectively, the incidence rate in Oslo is still remarkably high.
Possible explanations for the decrease in incidence
Use of anti-osteoporosis drugs
Bisphosphonates were not on the market in Norway before 1996, and patients with hip fractures before this period were not treated with AOD [24]. In the incidence study from 2007, the use of bisphosphonates may have explained some of the reduction, up to 13% for women between 60 and 69 years and 34% for women 70–79 years [5]. Since 2007, the use of oral bisphosphonates (alendronate) has gradually decreased in Oslo in coherence with other studies and might be due to concerns among general practitioners and patients regarding adverse events [9, 24, 25]. Zoledronate and denosumab became available in Norway in 2007 and 2011, respectively, and the use of both zoledronate and denosumab is increasing in Norway [24, 26]. After the Norwegian Capture the Fracture Initiative (NoFRACT) project started systematic secondary fracture prevention in Oslo in 2015, treatment with AOD increased [24, 27, 28]. However, it is difficult to quantify the number of patients who has received this treatment over the last 5 years as zoledronate is given mostly in hospitals and thereby not registered in the Norwegian prescription database. A study explaining the reduction of hip fracture incidence in Norway found that the use of AOD could explain 20% of the reduction in the incidence between 1999 and 2019 (11% for alendronate, 4% for zoledronate, and 6% for denosumab) [29]. In Denmark, the incidence of hip fractures decreased by 30% from 2005 to 2015, and they could in a best-case scenario conclude that AOD explained 20% of this decrease [23]. A study from Norway found a lower risk of hip fractures for women exposed to bisphosphonates and denosumab [30]. Measuring the effect of AOD could be challenging due to the residual effect after discontinuing the medication both for bisphosphonates and denosumab [31]. Furthermore, the effectiveness of alendronate is influenced by variations in users’ compliance, making it challenging to assess the impact [29]. Additionally, treatment with zoledronate usually starts after the patient has sustained a hip fracture. As a result, determining the impact on the declining incidence of hip fractures can be complex and inconclusive.
Proportion of cervical and trochanteric fractures
The decline in trochanteric fractures seems to be more pronounced than for cervical fractures. For both sexes, the risk of trochanteric fractures was approximately twice as high in 1996/1997 than in 2019 (Table 3). The cause of the substantial decrease in trochanteric fractures remains unknown, although there are disparities between individuals experiencing a trochanteric fracture versus a cervical hip fracture [32]. We found that patients sustaining a trochanteric fracture had a higher mean age than patients with a cervical fracture, 82 and 80, respectively. They were more likely to live in a permanent nursing home prior to the fracture, consistent with the results from Kujala [32] showing less patients with trochanteric fractures living independently at home. The ratio between cervical and trochanteric fractures changed with age, with a higher ratio of cervical fractures in older age groups for males (Table 1). For females, the ratio between cervical and trochanteric fractures was less in the highest age groups. The same results were seen in Tanner et al. [33], where the proportion of females sustaining a trochanteric fracture increases with age, while for males the proportion decreases. Additionally, a Swedish study reported that males with trochanteric fractures had a higher 1-year mortality despite a lower mean age than females [34]. The reduction in trochanteric fractures may be related to improved health among the elderly population, especially in men.
Healthier elderly population
While the elderly population is expected to increase, the age-standardized incidence of hip fractures is decreasing in Western countries [15]. The same trend is seen in two other high-risk diagnoses, stroke and myocardial infarction [35]. As for stroke and myocardial infarction, the decline may partly be explained by a healthier elderly population. Factors such as increased levels of body mass index (BMI), less smoking, and higher physical activity may be part of the explanation [22, 29].
Modifiable risk factors for hip fractures include low BMI and low body weight, which are associated with the highest risk [36]. Additionally, other modifiable risk factors include current smoking, inactivity, and high daily alcohol consumption [36]. In Norway, BMI has increased in all age groups from newborn to the oldest population throughout the twentieth century [37]. A study on hip fracture incidence in Norway in 2019 found that increased BMI could have explained 25% of the hip fracture reduction [29]. As for BMI levels in Oslo, a study conducted in the 1990s found that residents living in Oslo were taller and leaner compared to other areas in Europe [38]. Knowing that the BMI levels in Oslo have increased over the past 30 years, this might have contributed to the decline of hip fractures in Oslo.
Furthermore, current smoking is related to low BMI, and the risk of fractures is higher in persons with both low BMI and current smoking [37]. The Norwegian study from 2019 found an 11% reduction in hip fractures attributed to a decline in daily smokers [29]. The number of daily smokers in Norway in the age groups above 55 years has decreased from 20 to 13.5% for females and 24 to 12% for males between 2004 and 2019 [16]. The reduction appears to be even higher in Oslo compared to the rest of the country, with a six percent prevalence of daily smokers in the adult population in 2018 for Oslo, while the whole country had a nine percent smoking rate [16]. Additionally, both current and former smoking are associated with a higher risk of a trochanteric fracture than a cervical fracture [39]. The number of smokers among men has decreased in Norway, potentially contributing to the large reduction in trochanteric hip fractures over the past decades.
As for BMI, the level of physical activity seems to have increased in the Norwegian population over the last decades, also among elderlies [40]. Given that sedentary behavior increases the risk of hip fractures, increasing physical activity could have contributed to the reduced incidence hip fractures [29]. Most hip fractures occur due to a fall, and low physical activity is associated with risks of fall and subsequent hip fracture [41]. Besides, it has been observed that individuals who engage in excessive alcohol consumption are more disposed to falls [41]. While the overall consumption of alcohol among elderly individuals in Norway has seen a slight upward trend, the number of individuals categorized as excessive alcohol consumers has remained constant [42]. Søgaard et al. [41] found that the use of psychotropic and analgesic medications was a predictor for future hip fractures. The use of benzodiazepine has declined in Norway, and this decline was found to explain 13% of the hip fracture reduction in Norway [29]. Furthermore, as the population experiences improved health and longer lifespans, there has been an almost doubling in the number of individuals in need of total hip arthroplasty over the past decade [8]. Kjeldgaard et al. found that 17% of the hip fracture reduction could be explained due to hip arthroplasty [8]. Although the patient may sustain a periprosthetic fracture instead, however this was not investigated in the referred study [8].
Influence of immigration
In 2019, almost all individuals who experienced a hip fracture in Oslo were born in Norway. A Norwegian study that compared hip fracture rates among immigrant groups to those born in Norway found a lower incidence in all immigrant groups [43]. Similar results have been observed in Sweden [44]. Between 2007 and 2019, the percentage of Oslo residents over 50 years with immigrant background rose from 13 to 20% for females and from 17 to 25% for males [16]. For comparison, elderly with an immigrant background constituted 7% of the total population over 60 years in Norway in 2021 [45]. The proportion of the population with immigrant background has seen a greater increase in Oslo than in other parts of Norway. In fact, Oslo hosts over five times as many elderly immigrants as the municipality with the second-highest immigrant population [45]. As persons with ancestry from Africa and Asia probably are less disposed to suffer hip fractures, this effect may be more prominent in Oslo than in other parts of the country. However, the immigrant population remains relatively young, and the effect of immigration on hip fracture incidence may be more prominent in the years to come.
Strengths and limitations
This study had some limitations. We lacked information on immigration status on the individual level, preventing us from conducting sensitivity analysis on differences due to ethnicity.
To compare the 2019 incidence with previous years, we opted to exclude subtrochanteric fractures from the main analysis, consistent with previous studies. However, subtrochanteric fractures were included in supplementary analysis. Typically, subtrochanteric fractures are included in hip fracture incidence studies, and future incidence studies from Oslo should include these fractures.
The strength of this study was that all data was verified from patients' records from the hospitals’ database. This allowed for clarification of patients who were registered with an incorrect diagnosis. By using the same thorough fracture identification method as in the previous studies, we were able to accurately monitor changes in the incidence of cervical and trochanteric fractures in Oslo over five decades.
Conclusion
The incidence of hip fractures in Oslo has reached the lowest level measured since the late 1970s with a significant reduction in incidence rates for both females and males. The decline in hip fractures was most pronounced in the oldest age groups, particularly among females. The risk of trochanteric fractures has declined, especially throughout the last 20 years for males. The incidence in Oslo has previously been higher compared to the rest of Norway but has now decreased to a level below the country average. The incidence is still remarkably high, and Oslo is still registered with one of the highest hip fracture incidences worldwide. Further investigations of the hip fracture incidence in Oslo are of particular interest due to the remarkably higher decrease compared to the rest of the country of Norway. Factors such as the influence of immigration as well as the increasing number of elderly individuals in the years to come might interfere with the decreasing trend.
Data Availability
Data are available on reasonable request from the corresponding author.
References
Cauley JA, Chalhoub D, Kassem AM, Fuleihan GH (2014) Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol 10(6):338–351
Sugand K, Ali R, Goodall R, Salciccioli J, Marshall D, Schuster-Bruce J et al (2023) Trends in neck of femur fracture incidence in EU15+ Countries from 1990–2017. Injury 54(2):645–651
Lofthus CM, Osnes EK, Falch JA, Kaastad TS, Kristiansen IS, Nordsletten L et al (2001) Epidemiology of hip fractures in Oslo. Norway Bone 29(5):413–418
Falch JA, Ilebekk A, Slungaard U (1985) Epidemiology of hip fractures in Norway. Acta Orthop Scand 56(1):12–16
Støen RO, Nordsletten L, Meyer HE, Frihagen JF, Falch JA, Lofthus CM (2012) Hip fracture incidence is decreasing in the high incidence area of Oslo, Norway. Osteoporos Int 23(10):2527–2534
Forsén L, Søgaard AJ, Holvik K, Meyer HE, Omsland TK, Stigum H et al (2020) Geographic variations in hip fracture incidence in a high-risk country stretching into the Arctic: a NOREPOS study. Osteoporos Int 31(7):1323–1331
Falch JA, Kaastad TS, Bøhler G, Espeland J, Sundsvold OJ (1993) Secular increase and geographical differences in hip fracture incidence in Norway. Bone 14(4):643–645
Kjeldgaard HK, Meyer HE, O’Flaherty M, Apalset EM, Dahl C, Emaus N et al (2022) Impact of total hip replacements on the incidence of hip fractures in Norway during 1999–2019. A Norwegian Epidemiologic Osteoporosis Studies (NOREPOS) Study. J Bone Miner Res 37(10):1936–43
Sing CW, Lin TC, Bartholomew S, Bell JS, Bennett C, Beyene K et al (2023) Global epidemiology of hip fractures: secular trends in incidence rate, post-fracture treatment, and all-cause mortality. J Bone Miner Res 38(8):1064–1075
Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Kristensen TB, Gjertsen JE (2019) Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73 557 patients reported to the Norwegian hip fracture register. Bone Joint J. 101-b(9):1129–37
Tang VL, Sudore R, Cenzer IS, Boscardin WJ, Smith A, Ritchie C et al (2017) Rates of recovery to pre-fracture function in older persons with hip fracture: an observational study. J Gen Intern Med 32(2):153–158
Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashner TM (1999) Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci 54(12):M635–M640
Hassani S, Lindman AS, Kristoffersen DT, Tomic O, Helgeland J (2015) 30-day survival probabilities as a quality indicator for Norwegian hospitals: data management and analysis. PLoS One 10(9):e0136547
Hektoen LF, Saltvedt I, Sletvold O, Helbostad JL, Lurås H, Halsteinli V (2016) One-year health and care costs after hip fracture for home-dwelling elderly patients in Norway: results from the Trondheim Hip Fracture Trial. Scand J Public Health 44(8):791–798
Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP et al (2016) The world report on ageing and health: a policy framework for healthy ageing. Lancet 387(10033):2145–2154
Statistics Norway. Available from : www.ssb.no/en. Accessed 15 Jan 2024
United Nations. World population prospects 2022: department of economic and social affairs, population division 2022 (online ed.). Available from: https://population.un.org/wpp/Download/Standard/Population/. Accessed 15 Jan 2024
Brennan SL, Pasco JA, Urquhart DM, Oldenburg B, Hanna FS, Wluka AE (2010) The association between urban or rural locality and hip fracture in community-based adults: a systematic review. J Epidemiol Community Health 64(8):656–665
Odén A, Kanis JA, McCloskey EV, Johansson H (2014) The effect of latitude on the risk and seasonal variation in hip fracture in Sweden. J Bone Miner Res 29(10):2217–2223
Johansen A, Grose C, Havelock W (2020) Hip fractures in the winter - using the National Hip Fracture Database to examine seasonal variation in incidence and mortality. Injury 51(4):1011–1014
Solbakken SM, Magnus JH, Meyer HE, Emaus N, Tell GS, Holvik K et al (2014) Impact of comorbidity, age, and gender on seasonal variation in hip fracture incidence. A NOREPOS study. Arch Osteoporos 9:191
Meyer AC, Ek S, Drefahl S, Ahlbom A, Hedström M, Modig K (2021) Trends in hip fracture incidence, recurrence, and survival by education and comorbidity: a Swedish register-based study. Epidemiology 32(3):425–433
Abrahamsen B, Skjødt MK, Vestergaard P (2019) Hip fracture rates and time trends in use of anti-osteoporosis medications in Denmark for the period 2005 to 2015: missed opportunities in fracture prevention. Bone 120:476–481
Norwegian Prescription Database (NorPD). The norwegian institute of public health. Available from: https://www.norpd.no/default.aspx. Accessed 15 Jan 2024
Conley RB, Adib G, Adler RA, Åkesson KE, Alexander IM, Amenta KC et al (2020) Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res 35(1):36–52
Farmastat. Available from: https://www.farmastat.no/. Accessed 15 Jan 2024
Andreasen C, Solberg LB, Basso T, Borgen TT, Dahl C, Wisløff T et al (2018) Effect of a fracture liaison service on the rate of subsequent fracture among patients with a fragility fracture in the Norwegian Capture the Fracture Initiative (NoFRACT): a trial protocol. JAMA Netw Open 1(8):e185701
Solberg LB, Vesterhus EB, Hestnes I, Ahmed MV, Ommundsen N, Westberg M, Frihagen F (2023) Comparing two different orthogeriatric models of care for hip fracture patients: an observational prospective cross-sectional study. BMJ Open Qual 12(Suppl 2). https://doi.org/10.1136/bmjoq-2023-002302
Kjeldgaard HK, Holvik K, Abrahamsen B, Tell GS, Meyer HE, O’Flaherty M (2023) Explaining declining hip fracture rates in Norway: a population-based modelling study. Lancet Reg Health Eur 30:100643
Riska BSL, Gunnes N, Stigum H, Finnes TE, Meyer HE, Omsland TK et al (2023) Time-varying exposure to anti-osteoporosis drugs and risk of first-time hip fracture: a population wide study within the Norwegian Epidemiologic Osteoporosis Studies (NOREPOS). Osteoporos Int 34(8):1369–1379
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA et al (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296(24):2927–2938
Kujala MA, Hongisto MT, Luukkaala T, Stenholm S, Nuotio MS (2023) Pertrochanteric hip fracture is associated with mobility decline and poorer physical performance 4 to 6 months post-hip fracture. BMC Geriatr 23(1):722
Tanner DA, Kloseck M, Crilly RG, Chesworth B, Gilliland J (2010) Hip fracture types in men and women change differently with age. BMC Geriatr 10:12
Mattisson L, Bojan A, Enocson A (2018) Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord 19(1):369
Shah ASV, Lee KK, Pérez JAR, Campbell D, Astengo F, Logue J et al (2021) Clinical burden, risk factor impact and outcomes following myocardial infarction and stroke: a 25-year individual patient level linkage study. Lancet Reg Health Eur 7:100141
Mortensen SJ, Beeram I, Florance J, Momenzadeh K, Mohamadi A, Rodriguez EK et al (2021) Modifiable lifestyle factors associated with fragility hip fracture: a systematic review and meta-analysis. J Bone Miner Metab 39(5):893–902
Kvamme JM, Wilsgaard T, Florholmen J, Jacobsen BK (2010) Body mass index and disease burden in elderly men and women: the Tromsø Study. Eur J Epidemiol 25(3):183–193
Meyer HE, Falch JA, O’Neill T, Tverdal A, Varlow J (1995) Height and body mass index in Oslo, Norway, compared to other regions of Europe: do they explain differences in the incidence of hip fracture? European Vertebral Osteoporosis Study Group. Bone 17(4):347–350
Michaëlsson K, Weiderpass E, Farahmand BY, Baron JA, Persson PG, Zidén L et al (1999) Differences in risk factor patterns between cervical and trochanteric hip fractures. Swedish Hip Fracture Study Group. Osteoporos Int. 10(6):487–94
Vie TL, Hufthammer KO, Rangul V, Andersen JR, Meland E, Breidablik HJ (2023) Patterns of physical activity over 34 years in a large sample of adults: the hunt study, Norway. Scand J Public Health 14034948231174947. https://doi.org/10.1177/14034948231174947
Søgaard AJ, Aga R, Holvik K, Meyer HE (2022) Characteristics of fallers who later sustain a hip fracture: a NOREPOS study. Osteoporos Int 33(11):2315–2326
Tigerstedt C, Agahi N, Bye EK, Ekholm O, Härkönen J, Jensen HR et al (2020) Comparing older people’s drinking habits in four Nordic countries: summary of the thematic issue. Nordic Stud Alcohol Drugs 37(5):434–43
Aamodt G, Renolen R, Omsland TK, Meyer HE, Rabanal KS, Søgaard AJ (2020) Ethnic differences in risk of hip fracture in Norway: a NOREPOS study. Osteoporos Int 31(8):1587–1592
Johansson H, Odén A, Lorentzon M, McCloskey E, Kanis JA, Harvey NC et al (2015) Is the Swedish FRAX model appropriate for Swedish immigrants? Osteoporos Int 26(11):2617–2622
Statistics Norway. Elderly immigrants in Norway 2022. Available from: https://www.ssb.no/befolkning/innvandrere/artikler/eldre-innvandrere-i-norge.demografi-boforhold-inntekt-formue-og-helse/_/attachment/inline/cb7dac40-d211-4b7e-b435-9ac91ec37381:47310c1740eaf4b1a054f7a92073f79836883241/RAPP2022-02.pdf. Accessed 15 Jan 2024
Acknowledgements
Akershus University Hospital for contribution to the collection of data for the study.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital) Oslo University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hestnes, I., Solberg, L.B., Meyer, H.E. et al. The hip fracture incidence in the high-risk area Oslo continues to decline. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07156-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07156-8