Abstract
Summary
The role of recent fracture site in predicting the most detrimental subsequent fractures, hip and vertebral, is unclear. This study found that most recent fracture sites were associated with an increased risk of both hip and vertebral fracture, a finding that may impact the design of secondary prevention programs.
Background
Hip and vertebral fractures are the most serious in terms of associated morbidity, mortality, and societal costs. There is limited evidence as to which fracture types are associated with the highest risk for subsequent hip and vertebral fractures. This study aims to explore the dependency of imminent hip and vertebral fracture risk on the site of the recent index fracture.
Methods
Conducted as a nationwide retrospective cohort study, we utilized Swedish national registers to assess the risk of hip and vertebral fractures based on the site of the recent (≤ 2 years) index fracture and an old (> 2 years) prevalent fracture. This risk was compared to that observed in individuals without any prevalent fractures. This study encompassed all Swedes aged 50 years and older between 2007 and 2010. Patients with a recent fracture were categorized into specific groups based on the type of their previous fracture and were followed until December 2017, with censoring for death and migration. The study assessed the risk of hip and vertebral fractures during the follow-up period.
Results
The study included a total of 3,423,320 individuals, comprising 145,780 with a recent fracture, 293,051 with an old fracture, and 2,984,489 without a previous fracture. The median follow-up times for the three groups were 7.6 years (IQR 4.0–9.1), 7.9 years (5.8–9.2), and 8.5 years (7.4–9.7), respectively. Patients with a recent fracture at almost all sites exhibited a significantly increased risk of hip fracture and an elevated risk of vertebral fracture compared to controls.
Patients with recent fractures had an increased risk of subsequent hip and vertebral fractures, regardless of the index fracture site. These results strengthen the notion that all patients with a recent fracture, regardless of fracture site, should be included in secondary prevention programs, to improve the prevention of the clinically most serious fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures, particularly in the hip and spine, lead to considerable suffering, morbidity, and mortality, resulting in substantial societal and healthcare costs [1, 2]. Upon reaching the age of fifty, women face a 50% lifetime risk of experiencing a fragility fracture, while men face a 20% risk [3]. Patients sustaining an initial fracture encounter a pronounced and increased risk of recurrent fracture particularly during the first 2 years following the index fracture [4, 5]. The occurrence of a recent fracture, especially of the spine, significantly influences the 10-year probability of experiencing a new fracture [6].
There is recent evidence that a previous fracture regardless of site results in an elevated risk of any imminent fracture [7]. However, it has yet not been demonstrated how the index fracture site is associated with the two most detrimental incident clinical fracture types, hip and vertebral fracture. Hip fractures often lead to decreased mobility, reduced quality of life, increased morbidity and mortality [8,9,10], while vertebral fractures frequently result in chronic pain, reduced physical function, and increased mortality although the mortality increase occurs more gradually than what is observed for hip fracture [11, 12]. This is of great importance to investigate, since currently available osteoporosis medications, including bisphosphonates, denosumab, teriparatide, and romosozumab, increase bone mineral density (BMD) and are particularly effective in reducing the risk vertebral fractures, with relative risk reductions (RRR) of approximately 45–70% and hip fractures with RRR of about 40% [13].
To allow the prevention of clinically very serious fractures of the spine and hip, it is imperative to identify relevant prognostic markers, of which previous fracture constitutes one. If a recent fracture increases a risk factor for subsequent fracture of the spine or hip, regardless of fracture site, it would further emphasize the importance of including all fracture sites in secondary prevention programs such as Fracture Liaison Services (FLS) [14].
In a national, retrospective Swedish cohort study of all adults, 50 years and older, we recently demonstrated that the risk of any subsequent fracture, major osteoporotic fracture (MOF), and non-MOF was increased regardless of recent index fracture site [7]. The primary aim of the present study was to investigate, in the same population, if the risk of hip and vertebral fracture after a recent fracture is dependent on the index fracture site. We further aimed to determine if such associations were dependent on age and sex.
Methods
Study design
Using national registers in Sweden, we designed this nationwide retrospective cohort study to assess the risk of incident hip and vertebral fracture in patients with recent fractures (≤ 2 years) categorized by fracture site, in patients with old fractures (> 2 years), and in control patients without previous fractures (Fig. 1). As previously reported [7], all men and women in Sweden who were born in 1977 or earlier and were alive in 2005 were assigned a random baseline date between 2007 and 2010. Individuals aged 50 years or older and alive at baseline were included in the study. Patients who recently (≤ 2 years) suffered a fracture were categorized into groups using ICD-10 codes with four characters. Clinically similar fracture sites were grouped together to reach sufficient statistical power (≥ 80%) to detect an 82% increased risk, which was the overall risk increase in a large meta-analysis investigating the association between previous fracture and risk of subsequent fracture [15]. Due to differences in hip and vertebral fracture incidence, the smallest possible grouping of recent fracture sites differed in the two analyses. In the control group, the number of incident hip and vertebral fractures were 99,671 (3.3%) and 20,510 (0.69%), respectively. Therefore, to fulfill the same power assumptions, the minimum group size in the two analyses differed, 946 for the hip fracture analysis and 2581 for the vertebral fracture analysis, respectively. The two categorizations according to index fracture sites are specified in Supplemental Tables S1 and S2, respectively. The study was funded by the Swedish Research Council and the Sahlgrenska University Hospital Funds and received ethical approval from the Swedish Ethical Review Authority.
Data sources
Diagnoses for fractures and comorbidity were obtained from the National Patient Register, including both outpatient and inpatient hospital visits. Medication data was collected from the Swedish Prescribed Drug Register, which commenced on July 1, 2005, and includes all prescribed medications from both hospitals and primary care. The dates of deaths were acquired from Statistics Sweden. In Sweden, all residents receive a personal identification number at birth or upon immigration, allowing swift linkage between the registers.
Variables
Apart from pathological fracture diagnoses, all fracture diagnoses were included regardless of the trauma mechanism. Hip fracture and vertebral fracture were assessed as outcomes. Hip fracture included diagnoses of a fractured femoral head, neck, trochanter, or subtrochanteric part of the femur in combination with a code for surgical procedure. Vertebral fractures included both cervical, thoracic, and lumbar spine fractures. Covariates with a possible influence on fracture risk were selected; age, sex, inclusion year, and the most recent year’s osteoporosis medication, multiple recent fractures, and the Charlson comorbidity index, the latter quantifying comorbidity [16]. The osteoporosis medication data included hospitals and primary care prescriptions during the last 12 months as well as codes for medications administered via infusion (zoledronic acid) or injection (denosumab) at healthcare facilities. Detailed descriptions of vertebral and hip fracture outcomes are presented in Supplemental Table S3, and definitions of other study subject characteristics including Charlson comorbidity weights are presented in Supplemental Table S4.
Statistical analyses
Baseline characteristics for the three groups (recent fracture, old fracture, and no previous fracture) are presented as counts with percentages for categorical variables and averages with standard deviations (SD) for continuous variables. Event rates were computed as the number of events per 1000 person-years and presented with exact Poisson 95% confidence intervals (CI). To calculate hazard ratios for each group of recent fractures compared to patients with no previous fracture, we used Cox regression models. The hazard ratios were adjusted for age and sex (model 1) and multivariable adjustment (model 2). The follow-up was censored for emigration, death, and at the end of the study (December 31, 2017). The assumption of proportional hazards was tested using graphical methods. Forest plots were used to present the multivariable-adjusted hazard ratios per group of recent fracture. In the multivariable-adjusted Cox models, interaction terms for the categorical group variable (recent fracture group vs. no fracture) and age and sex, respectively, were added and tested. For the interaction terms, we considered p values less than 0.10 significant. We performed subgroup analyses per sex and age group and sensitivity analyses with censoring after 2 years. Due to the high and varying mortality in the cohort, the subdistribution hazard ratios for hip and vertebral fractures were analyzed using a Fine and Gray model to assess the potential impact of death as a competing risk [17]. All patients with recent femur/hip fracture were compared with a subset of 20,000 randomly selected persons from the control group without a previous fracture. Statistical analyses were performed using R 4.2.2 and R-Studio version 2023.03.0.
Results
Study population
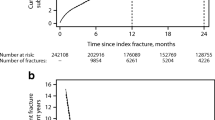
As previously reported, the study population included 3,423,320 persons [7]. At baseline, 145,780 had a recent fracture, 293,051 had experienced a fracture more than 2 years ago, and 2,984,489 persons had no previous fractures. The mean (standard deviation (SD)) age for the groups was 72.2 (12.7), 70.2 (12.3), and 65.5 (10.8), respectively. Osteoporosis medication use in the last year was more common among patients with a recent fracture (13.1%) than in patients with a fracture more than 2 years ago (10.4%) and in study subjects without previous fractures (4.5%). Charlson comorbidity index was highest among patients with a recent fracture, followed by patients with older fractures and by those without a previous fracture (Table 1). The median follow-up time for the three groups was 7.6 (IQR 4.0–9.1), 7.9 (5.8–9.2), and 8.5 years (7.4–9.7), respectively.
Risk of hip fractures
During follow-up, the 145,780 patients with a recent fracture suffered a total of 12,692 (8.7%) hip fractures while the patients with an old fracture at baseline sustained a total of 20,516 (7.0%) hip fractures, and persons with no previous fractures experienced 99,671 (3.3%) hip fractures. Compared to controls without a previous fracture, patients with a recent fracture had an increased risk of hip fracture in the Cox model adjusted for age and sex (model 1), with nearly all index fracture groups associated, with significant hazard ratios for 33 out of 36 investigated index fracture sites (Table 2). These hazard ratios were only slightly affected by multivariable adjustment (Table 2 and Fig. 2). Patients with a recent humerus fracture (HR 2.19 (95% CI 2.08–2.31)) and with a recent thoracic vertebral fracture (HR 2.18 (95% CI 1.88–2.52)) had among the highest risk of hip fracture. Except for index fractures at the femoral shaft, carpus, and lower end of the femur, all other index fracture sites exhibited a significantly increased risk of hip fracture in the model adjusted for age and sex (Table 2).
Risk of vertebral fractures
During follow-up, the 145,780 patients with a recent fracture suffered a total of 2596 (1.8%) vertebral fractures while patients with an old fracture at baseline sustained a total of 3925 (1.3%) vertebral fractures and persons with no previous fractures had 20,510 (0.69%) vertebral fractures. Compared to controls without previous fracture, patients with a recent fracture had a substantially increased risk of vertebral fracture in a Cox model adjusted for age and sex (model 1), regardless of fracture group investigated (Table 3). These hazard ratios were only slightly affected by multivariable adjustment (Table 3 and Fig. 3). Any recent vertebral fracture was associated with the greatest elevation of subsequent vertebral fracture risk (HR 8.33, 95% CI 7.45–9.31), while a recent distal radius fracture conferred the lowest risk increase (HR 1.64, 95% CI 1.46–1.85).
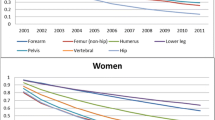
Risk of hip and vertebral fractures per sex
Sex interacted significantly (p value < 0.10) with 20 of 36 recent fracture sites for incident hip fracture and with 6 of 17 recent fracture sites for incident vertebral fracture (Supplemental Table S5A and S5B). For most fracture sites, the risk of hip and vertebral fracture was elevated in patients with recent fracture compared to controls with no previous fracture, regardless of sex (Supplemental Fig. 1–2, A-B). The relative risk increase was most pronounced among men, regardless of fracture site. For example, the risk of incident vertebral fracture was increased more than sevenfold for men with a recent vertebral fracture and almost sixfold for women, and the risk of incident hip fracture was more than tripled among men with a recent proximal humerus fracture and nearly doubled for women.
Risk of hip and vertebral fractures per age group
Age interacted significantly (p value < 0.10) with 33 of 36 recent fracture sites for incident hip fracture and 14 of 17 recent fracture sites for incident vertebral fracture (Supplemental Table S5A and S5B). For most fracture sites, compared to controls without previous fracture, the risk of both hip fracture and vertebral fracture was higher in patients with recent fracture regardless of age group (Supplemental Fig. 1–2, C-E). The relative risk increase was most pronounced among the youngest age group. For both the age group 50–64 and 65–79 years, most index fracture sites exhibited a significantly elevated risk of subsequent hip and vertebral fracture than what was observed for the most common index fracture site, i.e., the distal radius (S525). For instance, among those 50–64 years of age with a recent subtrochanteric, pertrochanteric, and femoral neck index fractures, the risk of incident hip fracture was increased more than sevenfold compared to controls with no previous fracture.
Risk of fractures with follow-up censored after 2 years
With a shortened follow-up time, the risk of hip and vertebral fracture was consistently higher in those with a recent fracture (Supplemental Figure S1F, S2F), regardless of the recent index fracture site, though with broader CIs.
Mortality and competing risk of death
During follow-up, there were 593,369 (19.9%) deaths in the patients with no previous fracture, 101,759 (34.7%) among the patients with old fractures, and 66,380 (44.2%) among the patients with recent a fracture. In particular, patients with recent femoral fractures, the number of deaths was 9296 (74.9%, neck), 6937 (82%, pertrochanteric), 1398 (75.1%, subtrochanteric), 714 (64.3%, shaft), and 683 (64.6%, lower end). When performing competing risk of death analyses with Fine and Gray comparing patients with different recent femoral fractures with patients with no previous fracture, the subhazard ratios for incident hip fracture differed slightly from the corresponding Cox hazard ratios (Supplemental Table S6). Three hazard ratios in Cox adjustment model 1 were non-significant whereas nine subhazard ratios (both models 1 and 2) were non-significant (recently fractured cervical vertebral, upper end of radius, carpus, lower end of femur, shaft and lower end of tibia, fibula, and toes). The equivalent subhazard ratios for incident vertebral fracture in patients were all significant and highly similar to the corresponding Cox hazard ratios regardless of recent fracture group (Supplemental Table S7).
Discussion
This nationwide cohort study followed 3,423,320 men and women, all 50 years or older in Sweden, for over 7 years. Patients with almost all different types of recent fractures at baseline had a higher risk of both hip and vertebral fractures. These risk increments were most pronounced in analysis with short follow-up time (2 years) and in the youngest age group. These results show that the risk of both hip and vertebral fracture is consistently elevated and to a large extent independent of the index fracture site, indicating that secondary fracture prevention programs should target all patients with recent fractures, which will likely enable the prevention of the clinically most serious fractures, those of the spine and hip.
There were some noteworthy dissimilarities in risk between the patients with different index fracture sites. The risk of incident hip fracture appeared to be close to neutral in patients with recent femur fractures in the analysis with all included study subjects. However, the age-stratified analysis demonstrated that the risk of subsequent hip fracture was very high in those with previous hip fractures in the youngest age group, an association not found in older patients, in which the risk tended to be reduced, compared to controls. This discrepancy could be due to a considerably higher competing risk of death in the oldest age group, in which patients with hip fracture are more likely to die before having another hip fracture. When considering the competing risk of death, the subhazard ratios were indeed higher than the corresponding hazard ratios. An additional reason for the lack of association between previous femur fracture and subsequent hip fracture could be due to the protective effect of surgery on the fractured hip, putting only one hip at risk for subsequent hip fracture. Another intriguing finding was that a recent carpus fracture exhibited no association with incident hip fracture, but a recent fracture in carpus/metacarpus was strongly associated with incident vertebral fracture, with a significant hazard ratio above 2. Some of the recently fractured groups (cervical vertebral, upper end of radius, carpus, lower end of femur, shaft and lower end of tibia, fibula, and toes) lacked significance when analyzing subhazard ratios for incident hip fracture. However, the equivalent recent fracture groups showed strong associations for incident vertebral fracture, both hazard and subhazard ratios.
We recently found that recent MOF and non-MOF as well as most recent fractures, regardless of index fracture site, were associated with an increased risk of any fracture in the herein investigated population [7]. However, for several reasons, the clinical utility of identifying which recent index fracture sites confer the highest risk for vertebral and hip fractures specifically is large. Both clinical spine fractures and hip fractures frequently lead to severe consequences in terms of disability, increased morbidity, and mortality, for the affected patients and for society and the healthcare system, in terms of substantial costs for surgical intervention, hospital care, rehabilitation, and nursing home care [18, 19]. Thus, prevention of these very serious fractures is key to combating adverse health outcomes and fracture-associated costs. The results from this study demonstrate that almost all recent fractures result in an increased risk of subsequent clinical spine fracture or hip fracture, indicating that selecting only patients with the most frequent osteoporotic fractures (usually spine, hip, proximal humerus, and distal radius) in FLSs will result in a missed opportunity to prevent spine and hip fractures in many high-risk patients with other types of recent fractures [20, 21].
The National Osteoporosis Guideline Group in the UK includes recommendations of an intervention threshold for pharmacological therapy equivalent to the 10-year fracture probability of a postmenopausal woman with a previous fracture [22, 23]. This treatment threshold definition and the observed elevated risk for hip and spine fracture observed for most index fracture sites in this study suggests that a large proportion of patients with recent fractures in this study would qualify for pharmacological intervention. Commonly available osteoporosis medications such as zoledronic acid and denosumab are particularly effective at reducing the risk of both vertebral and hip fractures, with relative risk reductions of approximately 70% and 40%, respectively [24, 25]. Furthermore, head-to-head trials using osteoanabolic medications, such as romosozumab and teriparatide, have demonstrated superior prevention of vertebral fractures and for romosozumab also for hip fractures, compared to oral bisphosphonates [26, 27]. Thus, effective medications are available to treat fracture patients highly vulnerable to suffering subsequent vertebral and hip fractures, and the results from the present study indicate that almost all fracture patients should be screened and offered osteoporosis medications if suitable.
The results herein indicate that almost all patients with a recent fracture have an elevated risk of incident hip and vertebral fracture. However, it should be noted that, since the study does not take BMD into account, the increased risk for some index fracture types could be due to more severe trauma or other factors than low BMD. However, a previous study found that almost all types of fractures are associated with low BMD [28]. Furthermore, also patients with diagnosed osteopenia, in addition to osteoporosis, benefit, in terms of lower fracture rates, from the osteoporosis medication zoledronic acid [24, 29]. Still, some patients with certain index fracture types may have relatively normal BMD and will not benefit from osteoporosis medication, emphasizing the need for BMD testing before treatment decisions are made.
In the present analysis, we opted to adjust the analyses for a minimal number of potential confounders, since the aim was to investigate how hip and vertebral fracture risk is determined by the site of index fracture and not to attempt to explain underlying mechanisms. However, models adjusted for age, sex, osteoporosis medication, multiple recent fractures, and comorbidity did not dramatically change the found associations between recent fracture and the risk of subsequent hip or spine fractures.
Importantly, the risk of subsequent hip and vertebral fracture was also considerably elevated for patients with fractures that occurred more than 2 years prior to baseline. This suggests that in addition to implementing Fracture Liaison Services (FLSs) for recent fractures, strategies to identify patients with old fractures may be justified to facilitate the prevention of subsequent fractures.
The risk of both subsequent hip and vertebral fracture was higher in younger patients, than in older, and in men than in women, for those with a recent fracture, indicating that imminent fracture risk is complex and to some extent age and sex-dependent. We find it noteworthy that, in most fracture sites, the risk of subsequent hip and vertebral fracture was higher than that observed for wrist fracture, which is the most common fracture type.
Among the strengths of the study is its mere size. To our knowledge, it is the largest investigation of subsequent hip and vertebral fracture risk in patients with a recent fracture depending on fracture site. The large size allowed the investigation of different index fracture sites with adequate statistical power. Extensive adjustment for age, sex, inclusion year, repeated fractures, osteoporosis medications, and Charlson comorbidity index did not materially change the found associations, which suggests that there was limited bias in the analysis.
However, there are also limitations. It is important to note that due to the observational design, it is not possible to establish causality. Also, the baseline characteristics of patients with recent fracture, old fracture, and no previous fracture differed substantially in terms of sex, age, and comorbidity. However, the observed associations remained consistent after multiple adjustments and in sensitivity analyses performed by subgroups of age and sex. Furthermore, BMD data was not accessible, and both American and British guidelines consider fracture risk to be the key component in determining treatment indication [22, 30]. Thus, not having BMD in the risk evaluation is a limitation. However, an association between low BMD and fractures at almost all sites has been reported [28], implying that patients with all index fractures in this study may have low BMD, but due to the lack of BMD data, we could not test whether the associations between previous and incident fractures were BMD independent. Last, it is worth mentioning that register studies may have limitations in accurately capturing fracture events. However, the positive predictive value for capturing fractures in the inpatient register is high, ranging from 85 to 95% [31]. Specifically for humeral fractures, the National Patient Register has a high level of completeness (97%), though with lower accuracy (70%) a concern partially addressed by the herein used wash-out period of 5 months for fractures occurring at the same skeletal site [32].
To conclude, patients recently suffering from a fracture exhibited an increased risk of subsequent hip and vertebral fractures, regardless of the index fracture site. These results strengthen the notion that all patients with recent fractures, regardless of the fracture site, should be included in secondary prevention programs such as FLSs, to improve prevention of the clinically most serious fractures.
Data availability
Due to ethical and legal considerations, the data cannot be released publicly. National legislation in Sweden, particularly the Public Access to Information and Secrecy Act (SFS 2009:400), imposes legal constraints on the disclosure of personal information in research studies. While the data supporting the study results may be made available upon request, it is subjected to assessment of confidentiality. Interested parties can apply to access specific public documents held by the University of Gothenburg that after undergoing necessary evaluation manages the integrity of the documents containing research data. For inquiries related to such matters, please contact the head of the Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, at medicin@gu.se.
References
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767
Lorentzon M, Nilsson AG, Johansson H, Kanis JA, Mellström D, Sundh D (2019) Extensive undertreatment of osteoporosis in older Swedish women. Osteoporosis Int 30(6):1297–1305. (Epub 20190225)
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367(9527):2010–2018
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15(4):721–739
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E et al (2017) Imminent risk of fracture after fracture. Osteoporos Int 28(3):775–780. (Epub 2016/12/29)
Kanis JA, Johansson H, Harvey NC, Gudnason V, Sigurdsson G, Siggeirsdottir K et al (2020) Adjusting conventional FRAX estimates of fracture probability according to the recency of sentinel fractures. Osteoporos Int 31(10):1817–1828. (Epub 20200701)
Axelsson KF, Litsne H, Lorentzon M (2023) The importance of recent prevalent fracture site for imminent risk of fracture - a retrospective, nationwide cohort study of older Swedish men and women. J Bone Miner Res 38(6):851–859. (Epub 20230424)
Haleem S, Choudri MJ, Kainth GS, Parker MJ (2023) Mortality following hip fracture: trends and geographical variations over the last sixty years. Injury 54(2):620–629. (Epub 20221209)
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C et al (2004) Mortality after osteoporotic fractures. Osteoporosis Int 15(1):38–42. (Epub 20031030)
Sernbo I, Johnell O (1993) Consequences of a hip fracture: a prospective study over 1 year. Osteoporos Int 3(3):148–153. (Epub 1993/05/01)
Lau E, Ong K, Kurtz S, Schmier J, Edidin A (2008) Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am 90(7):1479–1486
Johansson L, Svensson HK, Karlsson J, Olsson LE, Mellström D, Lorentzon M et al (2019) Decreased physical health-related quality of life-a persisting state for older women with clinical vertebral fracture. Osteoporosis Int 30(10):1961–1971. (Epub 20190621)
Lorentzon M (2019) Treating osteoporosis to prevent fractures: current concepts and future developments. J Intern Med 285(4):381–394. (Epub 2019/01/19)
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD et al (2013) Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152. (Epub 2013/04/17)
Kanis JA, Johansson H, McCloskey EV, Liu E, Åkesson KE, Anderson FA et al (2023) Previous fracture and subsequent fracture risk: a meta-analysis to update FRAX. Osteoporosis Int 34(12):2027–2045
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. (Epub 1987/01/01)
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6(2):99–105
Lorentzon M, Johansson H, Harvey NC, Liu E, Vandenput L, McCloskey EV et al (2022) Osteoporosis and fractures in women: the burden of disease. Climacteric 25(1):4–10. (Epub 20210728)
Paccou J, Philippoteaux C, Cortet B, Fardellone P (2023) Effectiveness of fracture liaison services in osteoporosis. Joint Bone Spine 90(5):105574. (Epub 20230418)
Axelsson KF, Johansson H, Lundh D, Möller M, Lorentzon M (2020) Association between recurrent fracture risk and implementation of fracture liaison services in four Swedish hospitals: a cohort study. J Bone Miner Res 35(7):1216–1223. (Epub 20200323)
Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, Gittoes NJL et al (2022) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 17(1):58. (Epub 20220405)
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A (2008) Case finding for the management of osteoporosis with FRAX–assessment and intervention thresholds for the UK. Osteoporosis Int 19(10):1395–1408. (Epub 20080828)
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356(18):1809–1822
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361(8):756–765. (Epub 20090811)
Saag KG, Petersen J, Brandi ML, Karaplis AC, Lorentzon M, Thomas T et al (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377(15):1417–1427. (Epub 20170911)
Kendler DL, Marin F, Zerbini CAF, Russo LA, Greenspan SL, Zikan V et al (2018) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 391(10117):230–240. (Epub 20171109)
Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS et al (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res 18(11):1947–1954
Reid IR, Horne AM, Mihov B, Stewart A, Garratt E, Wong S et al (2018) Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med 379(25):2407–2416. (Epub 20181001)
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A et al (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis - 2020 update executive summary. Endocr Pract 26(5):564–570
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C et al (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450. (Epub 2011/06/11)
Bergdahl C, Nilsson F, Wennergren D, Ekholm C, Möller M (2021) Completeness in the Swedish Fracture Register and the Swedish National Patient Register: an assessment of humeral fracture registrations. Clin Epidemiol 13:325–333. (Epub 2021/05/29)
Funding
Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Lorentzon has received lecture fees from Amgen, Astellas, GE-Lunar, Lilly, Meda/Mylan, Parexel International, and UCB Pharma, outside the present work. Mr. Litsne has no conflicts of interest to report. Dr. Axelsson has received lecture fees from Amgen, Mylan/Meda, and Lilly, all outside the present work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lorentzon, M., Litsne, H. & Axelsson, K.F. The significance of recent fracture location for imminent risk of hip and vertebral fractures—a nationwide cohort study on older adults in Sweden. Osteoporos Int 35, 1077–1087 (2024). https://doi.org/10.1007/s00198-024-07072-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07072-x