Abstract
Summary
We developed a new tool to assess the severity of osteoporotic vertebral fracture using radiographs of the spine. Our technique can be used in patient care by helping to stratify patients with osteoporotic vertebral fractures into appropriate treatment pathways. It can also be used for research purposes.
Purpose
The aim of our study was to propose a semi-quantitative (SQ) grading scheme for osteoporotic vertebral fracture (OVF) on anteroposterior (AP) radiographs.
Methods
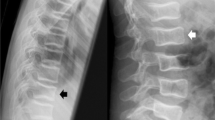
On AP radiographs, the vertebrae are divided into right and left halves, which are graded (A) vertical rectangle, (B) square, (C) traverse rectangle, and (D) trapezoid; whole vertebrae are graded (E) transverse band or (F) bow-tie. Type A and B were compared with normal and Genant SQ grade 1 OVF, Type C and D with grade 2 OVF, and Type E and F with grade 3 OVF. Spine AP radiographs and lateral radiographs of 50 females were assessed by AP radiographs SQ grading. After training, an experienced board-certified radiologist and a radiology trainee assessed the 50 AP radiographs.
Results
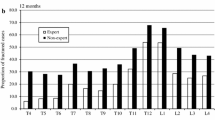
The height-to-width ratio of the half vertebrae varied 1.32–1.48. On lateral radiographs, 84 vertebrae of the 50 patients had OVFs (38 grade 1, 24 grade 2, and 22 grade 3). On AP radiographs, the radiologist correctly assigned 84.2%, 91.7%, and 77.2% and the trainee correctly assigned 68.4%, 79.2%, and 81.8% of grade 1, 2, and 3 OVFs, respectively. Compared with lateral radiographs, the radiologist had a weighted Kappa of 0.944 including normal vertebrae and 0.883 not including normal vertebrae, while the corresponding Kappa values for the trainee were 0.891 and 0.830, respectively.
Conclusion
We propose a new semi-quantitative grading system for vertebral fracture severity assessment on AP spine radiographs.






Similar content being viewed by others
Data Availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6:99–105. https://doi.org/10.1038/nrrheum.2009.260
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. https://doi.org/10.1007/s00198-006-0172-4
Li Y, Yan L, Cai S et al (2018) The prevalence and under-diagnosis of vertebral fractures on chest radiographs. BMC Musculoskelet Disord 19:235. https://doi.org/10.1186/s12891-018-2171-y
Kim DH, Vaccaro AR (2006) Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 6:479–487. https://doi.org/10.1016/j.spinee.2006.04.013
Weaver J, Sajjan S, Lewiecki EM et al (2017) Prevalence and cost of subsequent fractures among U.S. patients with an incident fracture. J Manag Care Spec Pharm 23:461–471. https://doi.org/10.18553/jmcp.2017.23.4.461
Delmas PD, Genant HK, Crans GG et al (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33:522–532. https://doi.org/10.1016/s8756-3282(03)00241-2
Sanchez-Rodriguez D, Bergmann P, Body JJ et al (2020) The Belgian Bone Club 2020 guidelines for the management of osteoporosis in postmenopausal women. Maturitas 139:69–89. https://doi.org/10.1016/j.maturitas.2020.05.006
Nuti R, Brandi ML, Checchia G et al (2019) Guidelines for the management of osteoporosis and fragility fractures. Intern Emerg Med 14:85–102. https://doi.org/10.1007/s11739-018-1874-2
Wang YXJ, Che-Nordin N, Deng M et al (2019) Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int 30:897–905. https://doi.org/10.1007/s00198-019-04856-4
Viswanathan M, Reddy S, Berkman N et al (2018) Screening to prevent osteoporotic fractures: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 319:2532–2551. https://doi.org/10.1001/jama.2018.6537
Crandall CJ, Newberry SJ, Diamant A et al (2014) Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med 161:711–723. https://doi.org/10.7326/M14-0317
Levis S, Theodore G (2012) Summary of AHRQ’s comparative effectiveness review of treatment to prevent fractures in men and women with low bone density or osteoporosis: update of the 2007 report. J Manag Care Pharm 18:S1–S15; discussion S13. https://doi.org/10.18553/jmcp.2012.18.s4-b.1
Howe TE, Shea B, Dawson LJ et al (2011) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev 6:CD000333. https://doi.org/10.1002/14651858.CD000333.pub2
Conley RB, Adib G, Adler RA et al (2020) Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res 35:36–52. https://doi.org/10.1002/jbmr.3877
Kwok TCY, Law SW, Leung EMF et al (2020) Hip fractures are preventable: a proposal for osteoporosis screening and fall prevention in older people. Hong Kong Med J 26:227–235. https://doi.org/10.12809/hkmj198337
Force USPST, Curry SJ, Krist AH et al (2018) Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA 319:2521–2531. https://doi.org/10.1001/jama.2018.7498
Camacho PM, Petak SM, Binkley N et al (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocr Pract 26:1–46. https://doi.org/10.4158/GL-2020-0524SUPPL
Wang YXJ, Du MM, Che-Nordin N et al (2020) Recognizing osteoporotic vertebral deformity on frontal view radiograph: a cohort analysis and a pictorial review. Arch Osteoporos 15:41. https://doi.org/10.1007/s11657-020-00716-5
Wang YXJ, Du EZ, Gong J, Cheng X (2021) Interpretation of osteoporotic vertebral deformity on frontal view radiographs of the chest and abdomen: a pictorial review. Quant Imaging Med Surg 11:423–442. https://doi.org/10.21037/qims-2020-28
Du EZ, Liu WH, Wang YXJ (2021) Improving osteoporotic vertebral deformity detection on chest frontal view radiograph by adjusted X-ray beam positioning. J Orthop Translat 28:169–178. https://doi.org/10.1016/j.jot.2021.04.001
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Wang YXJ, Santiago FR, Deng M, Nogueira-Barbosa MH (2017) Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 7:555–591. https://doi.org/10.21037/qims.2017.10.05
Wang YXJ, Diacinti D, Yu W et al (2020) Semi-quantitative grading and extended semi-quantitative grading for osteoporotic vertebral deformity: a radiographic image database for education and calibration. Ann Transl Med 8:398. https://doi.org/10.21037/atm.2020.02.23
Fleiss JL (1981) Statistical methods for rates and proportions, 2nd edn. John Wiley and Sons, New York
Jensen GF, McNair P, Boesen J, Hegedus V (1984) Validity in diagnosing osteoporosis. Observer variation in interpreting spinal radiographs. Eur J Radiol 4:1–3
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 15:887–896. https://doi.org/10.1007/s00198-004-1626-1
Yu W, Lin Q, Zhou X et al (2014) Reconsideration of the relevance of mild wedge or short vertebral height deformities across a broad age distribution. Osteoporos Int 25:2609–2615. https://doi.org/10.1007/s00198-014-2801-7
Wu CY, Li J, Jergas M, Genant HK (1995) Comparison of semiquantitative and quantitative techniques for the assessment of prevalent and incident vertebral fractures. Osteoporos Int 5:354–370. https://doi.org/10.1007/BF01622258
Ferrar L, Jiang G, Cawthon PM et al (2007) Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 22:1434–1441. https://doi.org/10.1359/jbmr.070608
Kleerekoper M, Neson DA, Peterson EL, Tilley BC (1992) Outcome variables in osteoporosis trials. Bone 13:S29–S34. https://doi.org/10.1016/s8756-3282(09)80007-0
Guglielmi G, Diacinti D, van Kuijk C et al (2008) Vertebral morphometry: current methods and recent advances. Eur Radiol 18:1484–1496. https://doi.org/10.1007/s00330-008-0899-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Ali Guermazi is the President of Boston Imaging Core Lab (BICL), LLC, and a consultant to Merck Serono, AstraZeneca, Pfizer, Galapagos, Roche, and Tissue Gene. Daichi Hayashi received publication royalties from Wolters Kluwer. Wei Yu, Wen-Min Guan, Qiang Lin, Mei-Mei Du, Wei-Bo Xia, and Yi-Xiang J Wang declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, W., Guan, WM., Hayashi, D. et al. Vertebral fracture severity assessment on anteroposterior radiographs with a new semi-quantitative technique. Osteoporos Int 35, 831–839 (2024). https://doi.org/10.1007/s00198-024-07024-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07024-5