Abstract
Summary
The evolution of pain and quality of life after a symptomatic vertebral fracture differs according to patient gender, with a worse evolution in women independently of the treatment received.
Purpose
In a previous randomized clinical study comparing the effect of vertebroplasty (VP) vs. conservative therapy (CT) on pain evolution and quality of life (QoL) of patients with symptomatic vertebral fractures (VF), we observed the development of chronic back pain in 23% of subjects, independently of the therapy received. This study analyses the effect of gender on the evolution of pain and QoL in these subjects.
Methods
118/125 randomized patients (27 males/91 females) with recent symptomatic VFs were evaluated. All received a standardized analgesic and antiosteoporotic format of treatment. Pain and QoL were evaluated by VAS and Qualeffo-41, respectively, at baseline, at 2 weeks and 2 and 6 months. We compared pain evolution and QoL after treatment (CT vs. VP) according to gender, and analysed factors including age, time of evolution, treatment received, baseline VAS, previous VFs (total and recent), incidental VFs, lumbar and femoral T-scores, and analgesic and antiosteoporotic treatment.
Results
At baseline, there were no differences in age (males 74.8 ± 11.2 vs. females:73.2 ± 8.7 years), time of evolution, number of VFs (males:3.8 ± 2.4 vs. females: 3.1 ± 2.4), treatment received (VP, males:59%, females:45%), lumbar or femoral T-score, baseline VAS (males:6.8 ± 2.1 vs. females:6.8 ± 2.2) or Qualeffo score (males:52.2 ± 24.4 vs. females:59.7 ± 20.6). Pain and QoL evolution differed according to gender, being better in males. These differences were significant after two months independently of the treatment and the development of incidental VF during follow-up.
Conclusions
Pain and QoL evolution after a symptomatic VF differs according to gender, with a worse evolution in women independently of the treatment received.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures (VFs) are the most common type of osteoporotic fracture. Although this type of fracture is frequently overlooked, they can cause chronic back pain and significant impairment in the quality of life [1,2,3]. Indeed, in a previous randomized controlled trial (RCT) comparing the effects of percutaneous vertebroplasty (VP) versus conservative treatment on the quality of life and pain relief in patients with painful osteoporotic VFs, we observed the development of chronic back pain in nearly one quarter of the patients (23%), independently of the treatment received (i.e., VP or conservative treatment) [4]. On evaluating the factors related to the development of chronic back pain, having a longer symptom onset time, multiple acute VFs and higher baseline scores for pain (evaluated by the visual analogue scale [VAS]) were related to chronic back pain, as was female gender [4]. Previous reports have also indicated female predominance related to the development of chronic back pain in patients with fragility fractures [5, 6]. However, whether this finding reflects a more severe disease in women [1, 2, 7,8,9,10] or differential pain response/evolution related to sex, is not known at present.
Therefore, the aim of this study was to analyse the effect of sex on the evolution of pain and quality of life in patients with symptomatic fragility VFs included in a previous RCT comparing the effect of vertebroplasty versus conservative treatment. To do this, we compared the evolution of pain and quality of life according to sex along the first 6 months of the study, controlling for possible factors that could be related to chronic back pain development in both genders as well as the type of treatment received for VsF (conservative vs. VP).
Materials and Methods
The detailed study design has been previously published [11]. Briefly, we performed a RCT comparing VP with conservative treatment for improving pain and quality of life in individuals with recent painful osteoporotic VFs over a 1-year follow-up period.
The study was conducted at the Neurointerventional Radiology Department of the Imaging Diagnostic Centre, in conjunction with the Rheumatology Department of the hospital. All patients were referred to the Rheumatology Department and those with clinical symptoms compatible with acute VF were screened. Inclusion criteria were: acute, painful osteoporotic VF from T4-L5 with clinical onset < 12 months, confirmed by spine radiography and the presence of oedema on magnetic resonance (MR) images or activity on bone scan and with a VAS score ≥ 4. Exclusion criteria were: untreatable coagulopathy, active local or systemic infection, current malignancy, vertebral canal occupation by a fragment of the vertebral body or non-osteoporotic VF, active associated disorders (i.e., fibromyalgia or spondyloarthropathies) or other disorders (i.e., dementia) that may interfere with correct assessment of quality of life and pain. Ethical approval was obtained from our hospital Ethics Committee (Project number 2907; Clinical Trials number ID NCT00994032) and all participants provided written informed consent.
Spinal X-rays and MR were performed in all subjects at baseline. Patients were clinically assessed at baseline and thereafter at 2 weeks, and at 2, 6 and 12 months. Medication details, including antiosteoporotic and analgesic therapy were recorded throughout the study. Treatment included calcitonin during the first month [12] and analgesics when necessary (with a standardized format that included tramadol up to 200 mg/day, ibuprofen 600 mg every 8 h, and acetaminophen 1 g every 8 h if needed and 25 mg of percutaneous fentanyl when necessary, according to the evolution of pain) in both groups of patients (with additional VP depending on randomization [the VP procedure was undertaken in symptomatic VF with associated oedema in MR]). After one month of treatment, patients began/or continued treatment with bisphosphonates (oral or intravenous), or teriparatide according to the attending physician. Analgesic treatment was categorized into minor analgesics (acetaminophen and/nonsteroidal anti-inflammatory drugs) and minor and major opiate derivatives. Pain assessment was based on the VAS (from 0 to 10: in which 0 indicates no pain and 10 indicates the maximum level of pain). For quality of life measurements, the Qualeffo-41 test was used. This questionnaire consists of 41 items and includes five domains: pain, physical function, social function, general health perception and mental function. Domain scores range from 0 to 5 and total Qualeffo-41 from 0 to 100, being 100 the worst status [13]. Pain and quality of life were assessed at baseline and at all the follow-up time points.
Bone densitometry was performed in all patients before randomization and at 12 months and standard radiographs of the thoracic and lumbar spine were obtained to analyse VFs at baseline, and at 6 and 12 months. According to the Genant criteria, the severity of the deformity was graded as mild (20–25% height reduction), moderate (25–40%) and severe (> 40%) [14].
Statistical Analysis
Quantitative variables were described using means and standard deviations whereas frequencies and percentages were reported for qualitative variables. Associations between gender and qualitative variables were assessed by the chi-square and Fisher’s exact tests, whereas t-tests were used for quantitative variables.
The evolution of pain measures over time was fitted using B-splines regression [15]. A random intercept at the subject level was included in the model to account for subject baseline variability and the cluster structure of data. Longitudinal correlation was taken into account by including an autoregressive residual in the model.
The means of pain measures by treatment group were compared at each visit time using a t-test. To avoid multiplicity of type-I error the p-values were adjusted using the Hochberg approach [16]. The present study compared the evolution of pain and quality of life between sexes during the first 6-month period of the study, since the number of subjects decreased at 12 months, and therefore the statistical analysis was not sufficiently powered.
The overall type-I error rate was set at 5%. Statistical analyses were carried out using nlme, splines and compareGroups packages [17] of R v4.1.3 software [18].
Results
Of the initial 125 (97 females/28 males) patients randomized, 118 (91 females/27 males) received the allocated intervention, and these were the subjects evaluated with a follow-up of 6 months.
As shown in Table 1, there were no statistically significant differences between the two groups of patients (males and females) with respect to the principal clinical characteristics at baseline. Thus, age (males: 74.8 ± 11.2 vs. females: 73.2 ± 8.7 years), time since symptom onset, number of VFs (males: 3.8 ± 2.4 vs. females: 3.1 ± 2.4), treatment received for VF (VP or conservative treatment), lumbar or femoral T-scores, baseline VAS values (males: 6.8 ± 2.1 vs. females: 6.8 ± 2.2) and total Qualeffo-41 score (males: 52.2 ± 24.4 vs. females: 59.7 ± 20.6) were similar in both groups of patients as were the number of recent VFs (with oedema) identified by MR (males: 2 ± 1.24 vs. females: 2 ± 1.32), the number of severe VFs and the number of VPs preformed per patient in each group ( Table 1).
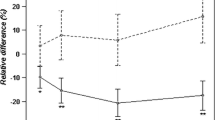
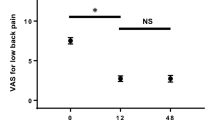
VAS scores significantly decreased in both groups of patients at all time points during the 6-month follow-up period (Figure 1A) However, the improvement in pain was greater in males after two months of evolution achieving a significant mean difference in VAS ≥ 2 (males vs. females: -2.0586 ± 0.737, p = 0.0247) at 6 months of follow-up, with similar results when evaluating the quality of life. Thus, the Qualeffo-41 total score showed a greater improvement in males (Figure 1B and Table 2) after two months, which was maintained at 6 months and with similar results in the Qualeffo subdomain of pain, again showing a more marked decrease in males (Figure 1C). This different evolution in pain and quality of life did not seem to be related to the initial treatment received for the VF, since both genders received similar therapeutic approaches (VP in 59% of males vs. 45% of females, p= n.s,) and showed a similar clinical response to VP and conservative treatment (interaction analysis of gender-treatment for VAS p=0.4 and for Qualeffo-41 p=0.4) and a similar use of analgesics (72.2% of males vs. 65.3% of women, p=n.s.). In addition, the development of incidental VFs during follow-up was similar in both genders (males: 18.5% vs. females 12.1%, p= n.s.).
When analysing the antiosteoporotic treatment, a slight but significantly lower number of males followed antiosteoporotic treatment at 6 months (74.1% males vs. 93.4% females, p=0.01), being oral bisphosphonates the most frequent type of antiosteoporotic treatment in both genders (66.7% in males vs. 69.2% in females); teriparatide and zoledronic acid were slightly more frequently used in females (teriparatide in males 3.7% vs. 12.1% in females; zoledronic acid in males 3.7% vs. 12.1% in females).
Discussion
Our results show that the evolution of pain and quality of life after a symptomatic VF differs according to sex, with a worse evolution in women compared to males.
Thus, the evolution of pain, evaluated by the VAS, and the Qualeffo-41 score clearly varied between genders, particularly two months after initiating treatment for the symptomatic VFs, showing a more marked relief in pain and improvement in the quality of life in males compared to females for up to 6 months of follow-up.
Several studies have shown gender differences in the development of chronic pain, with women being more frequently affected, particularly in relation to musculoskeletal disorders [19,20,21]. This finding has been related not only to the presence of more prevalent chronic pain conditions in women but also to higher acute pain sensitivity in this gender [19,20,21]. In fact, when comparing disease-associated pain scores in men and women with the same diagnosis, women had higher average pain scores than men for several disorders, including osteomuscular diseases and back pain [22].
Vertebral fractures are one of the most common manifestations of osteoporosis. This type of fracture may be associated with the development of chronic back pain and impaired quality of life [1,2,3]. Although the factors related to these complications are not fully clarified, some studies report that the severity of bone disease, particularly the number and the severity of the vertebral deformities, are factors that can be related to the development of chronic pain in these subjects [1, 2, 7,8,9,10]. In a previous RCT performed by our group in the same cohort of patients aimed at comparing the effects of VP versus the conservative approach on the quality of life and pain relief, no significant differences were observed after two months of treatment [11]. In addition, independently of the treatment received, nearly one quarter of patients developed chronic back pain [4]. When we analysed the factors related to the development/maintenance of back pain, subjects with a longer time since symptom onset, particularly greater than four months, having higher VAS values at baseline, having multiple acute VF and female gender were related to the development of chronic back pain [4], with similar findings also reported by Firanescu et al. in a recent randomized study that also addressed the treatment of recent symptomatic VFs [6]. To our knowledge, there are no data comparing the evolution of pain and quality of life in symptomatic VFs according to gender. Therefore, whether or not the clinical evolution of symptomatic VF differs according to gender due to differences in the severity of the disease and/or the therapeutic approach remains to be fully investigated.
In the present study, the differences observed between genders did not seem to be related to differences in disease severity, since besides having a similar age, the men and women studied presented a similar number of VFs at baseline with the same mean number of recent VFs, when evaluated by MR imaging, and similar lumbar and femoral T-scores. In addition, the therapeutic approach in the randomization procedure (i.e., conservative treatment vs. VP) was also similar in both genders, as was the time since symptom onset and the proportion of subjects with less than 4 months from symptom onset. Moreover, the baseline scores for pain (VAS) and Qualeffo-41 were similar in both genders, with all of the above indicating a similar grade of disease severity and disability when comparing the two genders.
It should be noted that the evolution of pain and the Qualeffo-41 score differed after two months of initiating treatment for the symptomatic VFs. Thus, whereas pain relief and quality of life improved by a similar magnitude in both genders at two weeks, after two months males showed a greater improvement in pain and, consequently, in quality of life. These findings could have been related to a differential therapeutic approach or a higher incidence of new VFs in the two genders. However, no differences were observed in the incidence of new VFs, observing a similar proportion in both genders at 6 months. Again, there were no differences in the use of analgesics, including major opiate derivatives; however, despite women having a worse evolution of pain, they tend to have a lower consumption of analgesics, possibly related to the more frequent adverse effects to opiates derivatives described in women [23]. Conversely, a lower percentage of males was receiving antiosteoporotic treatment at 6 months. Nevertheless, whether this finding was due to a lower compliance or persistence of the antiosteoporotic treatment in males was not analysed in the present study. This is a recurrent finding that has been reported in several epidemiological studies, describing not only a less frequent prescription of antiosteoporotic treatment in males after a fragility fracture but also a lower compliance and persistence with antiosteoporotic treatment [24,25,26,27].
All of this suggests the influence of gender in the susceptibility to develop chronic pain in the individuals included in our study. Indeed, recent studies have revealed significant sex differences in the physiological mechanisms underlying pain, including distinct interactions between hormones and the immune system that influence the transmission of signals of pain and sex-specific involvement of genes and proteins [19, 21]. In this sense, genetic variations in the opioid receptor mu 1 have been associated with differences in the evolution of low back pain according to gender, particularly in terms of pain sensitivity and recovery [28]. On the other hand, it has been proposed that gender differences in pain are influenced by the way that male and female brains process emotional and arousal/attentional aspects of pain [28]. There are also gender differences in the structure and function of the brain throughout life, with additional psychosocial factors contributing to these differences. However, it is not known whether gender differences in pain-related brain regions could contribute to differences in the prevalence and severity of chronic pain [19,20,21]. Whatever the mechanisms, it seems clear that gender influences the efficacy of the therapeutic approach in symptomatic VFs, with a worse evolution in women, thereby indicating the need to take gender into account when evaluating the clinical response of these subjects.
Some of the limitations of this study were the low number of patients included in the analysis, particularly of males, and the fact that the study was not addressed to evaluate the effect of gender on the evolution of pain and the quality of life, and particularly on a more individualized evaluation of the cause of vertebral pain (apart from that attributed to the VF/s). Nonetheless, one of the strengths of this study is the precise evaluation of these patients, all included in a RCT with extensive analysis of clinical and radiological factors related to the evolution of pain, quality of life and incidence of new VFs, as well as being the only RCT to date analysing and comparing the clinical evolution of pain and quality of life according to gender.
In conclusion, the evolution of pain and quality of life after a symptomatic VF differs according to patient gender, with a worse evolution in women independently of the type of treatment received. Thus, gender should be taken into account when evaluating the most adequate therapeutic approach in patients with symptomatic VF, as well as effect of gender on the compliance and persistence of treatment. Further research is needed to confirm these results and future studies should be addressed to determine the best therapeutic approach according to gender in these subjects.
Data availability
Data will be made available upon reasonable request to the author.
References
Francis RM, Aspray TJ, Hide G, Sutcliffe AM (2008) Back pain in osteoporotic vertebral fractures. Osteoporos Int 19:895–903
Ensrud KE, Schousboe JT (2011) Vertebral fractures. N Eng J Med 346:1634–1642
Klazen CA, Verhaar HJ, Lohle PN, Lampmann LE, Juttmann JR, Schoemaker MC et al (2010) Clinical course of pain in acute osteoporotic vertebral compression fractures. J Vasc Interv Radiol 21:1405–1409
Peris P, Blasco J, Carrasco JL, Martinez-Ferrer A, Macho J, San Román L et al (2015) Risk factors for the development of chronic back pain after percutaneous vertebroplasty versus conservative treatment. Calcif Tissue Int 96:89–96
Suzuki N, Ogikubo O, Hansson T (2009) The prognosis for pain, disability, activities of daily living and quality of life after an acute osteoporotic vertebral body fracture: its relation to fracture level, type of fracture and grade of fracture deformation. Eur Spine J 18:77–88
Firanescu CE, Venmans A, de Vries J, Lodder P, Schoemaker MC, Smeets AJ et al (2022) Predictive Factors for Sustained Pain after (sub)acute Osteoporotic Vertebral Fractures. Combined Results from the VERTOS II and VERTOS IV Trial. Cardiovasc Intervent Radiol 45:1314–1321
O’Neill TW, Cockerill W, Matthis C, Raspe HH, Lunt M, Cooper C et al (2004) Back pain, disability, and radiographic vertebral fracture in European women: a prospective study. Osteoporos Int 15:760–765
Rostom S, Allali F, Bennani L, Abouqal R, Hajjaj-Hassouni N (2012) The prevalence of vertebral fractures and health-related quality of life in postmenopausal women. Rheumatol Int 32:971–980
Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K et al (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR et al (1992) Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 7:449–456
Blasco J, Martínez-Ferrer A, Macho J, San Roman L, Pomés J, Carrasco J et al (2012) Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res 27:1159–1166
Knopp JA, Diner BM, Blitz M, Lyritis GP, Rowe BH (2005) Calcitonin for treating acute pain of osteoporotic vertebral compression fractures: a systematic review of randomized, controlled trials. Osteoporos Int 16:1281–1290
Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O et al (1999) Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporos Int 10:150–160
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Eilers PHCMB (1996) Flexible smoothing with B-splines and penalties. Stat Sci 11:89–121
Hochberg Y (1988) A sharper Bonferroni procedure for multiple significance testing. Biometrika 75:800–803
Subirana I, Sanz H, Vila J (2014) Building Bivariate Tables: The compareGroups Package for R. J Stat Softw 57:1–16
R Core Team (2022) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/
Osborne NR, Davis KD (2022) Sex and gender differences in pain. Int Rev Neurobiol 164:277–307
García-Esquinas E, Rodríguez-Sánchez I, Ortolá R, Lopez-Garcia E, Caballero FF, Rodríguez-Mañas L et al (2019) Gender Differences in Pain Risk in Old Age: Magnitude and Contributors. Mayo Clin Proc 94:1707–1717
Overstreet DS, Strath LJ, Jordan M, Jordan IA, Hobson JM, Owens MA et al (2023) A Brief Overview: Sex Differences in revalent Chronic Musculoskeletal Conditions. Int J Environ Res Public Health 20:4521
Ruau D, Liu LY, Clark JD, Angst MS, Butte AJ (2012) Sex differences in reported pain across 11,000 patients captured in electronic medical records. J Pain 13:228–234
Lopes GS, Bielinski S, Moyer AM, Jacobson DJ, Wang L, Jiang R et al (2021) Sex differences in type and occurrence of adverse reactions to opioid analgesics: a retrospective cohort study. BMJ Open 11:e044157
Antonelli M, Einstadter D, Magrey M (2014) Screening and treatment of osteoporosis after hip fracture: comparison of sex and race. J Clin Densitom 17:479–483
Hadji P, Jacob L, Kostev K (2016) Gender- and age-related treatment compliance in patients with osteoporosis in Germany. Patient Prefer Adherence 10:2379–2385
Nakatoh S, Fujimori K, Tamaki J, Okimoto N, Ogawa S, Iki M (2021) Insufficient persistence of and adherence to osteoporosis pharmacotherapy in Japan. J Bone Miner Metab 39:501–509
Pedersen AB, Risbo N, Kafatos G, Neasham D, O’Kelly J, Ehrenstein V (2023) Utilization patterns and factors associated with persistence of new users of anti-osteoporosis treatment in Denmark: a population-based cohort study. Arch Osteoporos 18:19
Olsen MB, Jacobsen LM, Schistad EI, Pedersen LM, Rygh LJ, Røe C et al (2012) Pain intensity the first year after lumbar disc herniation is associated with the A118G polymorphism in the opioid receptor mu 1 gene: evidence of a sex and genotype interaction. J Neurosci 32:9831–9834
Acknowledgements
Study funded by Fundació La Marató de TV3, Spanish Society of Radiology and Catalan Society of Rheumatology.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. Funded by a grant of Fundació La Marató de TV3, the Spanish Society of Medical Radiology and the Catalan Society of Rheumatology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure statement
Pilar Peris, Jordi Blasco, Ana Monegal, Helena Florez, Nuria Guañabens, and Josep Lluis Carrasco declare that they have no conflict of interest related to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authors’ roles
Study design: PP, JLC. Study conduct: PP, JB, JLC. Data collection: PP, JB, AM, HF, NG, JLC. Data interpretation: PP, JLC. Drafting manuscript: PP, JLC. Revising manuscript content: PP, JB, AM, HF, NG, JLC. Approval of the final version of the manuscript: all authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Peris, P., Blasco, J., Monegal, A. et al. Effect of gender on the evolution of pain and quality of life after treatment of symptomatic vertebral fragility fractures. Osteoporos Int 35, 515–521 (2024). https://doi.org/10.1007/s00198-023-06960-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06960-y