Abstract
Summary
This registry-based study of 3068 patients with osteoporosis compared the anti-fracture effectiveness of denosumab versus bisphosphonates. Denosumab was associated with significantly greater risk reduction than alendronate or ibandronate for vertebral and any fractures. No difference in fracture risk reduction was found between zoledronate and denosumab.
Purpose
To analyse the fracture risk of patients with osteoporosis receiving bisphosphonates or denosumab in a real-world setting.
Methods
This registry-based cohort study evaluated patients taking denosumab, bisphosphonates or both sequentially. Fractures were analysed using rates, rate ratios and hazard ratios (HR), including both therapies as time-varying co-variates. Fracture risk hazards were adjusted (aHR) for baseline T-Scores and trabecular bone score (TBS) and were additionally analysed with inverse probability treatment weighting.
Results
A total of 3068 patients (89% female; median age at treatment onset, 69 years [63 to 76]) received denosumab (median duration 2.8 years, [2.2 to 4.7]), bisphosphonates (3.4 years, [2.1 to 5.7]) or both sequentially. Thus, 11,078 subject-years were assessed for bisphosphonates (41% alendronate, 36% ibandronate, 23% zoledronate) and 4216 for denosumab. Moreover, 48,375 subject-years were observed before treatment onset, in addition to 2593 years of drug holidays. A total of 1481 vertebral fractures (435 under therapy), 1508 non-vertebral fractures (499 under therapy) and 202 hip fractures (67 under therapy) occurred after age 50. The risks of vertebral, non-vertebral and hip fractures were significantly lower under all bisphosphonates, denosumab and drug holidays than before treatment onset (all p < 0.001). After adjusting for age, baseline T-scores and TBS, denosumab was associated with lower risk than alendronate or ibandronate for vertebral fractures (aHR 0.47 (0.35 to 0.64) and 0.70 [0.53 to 0.91], p < 0.001 and p = 0.009, respectively) and any fractures (aHR 0.62 [0.51 to 0.76] and 0.77 [0.64 to 0.92], p < 0.001 and p = 0.004). With propensity weighting, denosumab was associated with a lower hip fracture risk compared to alendronate (HR 0.54 [0.29 to 0.98], p = 0.044). No difference in fracture risk reduction (vertebral, non-vertebral or hip) was found between zoledronate and denosumab.
Conclusions
When adjusting for disease severity, denosumab was associated with significantly greater risk reduction than alendronate and ibandronate for vertebral fractures. No difference in fracture risk reduction was found between zoledronate and denosumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and fracture risk [1]. Antiresorptive therapies such as bisphosphonates and denosumab increase bone mineral density (BMD) and reduce the risk of fractures, which are major causes of disability and high healthcare costs [2]. Both agents inhibit osteoclast function, albeit with different mechanisms of action. When internalized from the bone surface, bisphosphonates bind to bone mineral and inhibit osteoclast function or promote osteoclast apoptosis [3]. These effects are long-lasting, extending for several months or years beyond treatment discontinuation. Denosumab, a fully humanized monoclonal IgG2 antibody, binds to the receptor activator of nuclear factor-κB ligand (RANKL) and thereby impairs the formation, activation and survival of osteoclasts [4]. This effect is quickly reversed upon denosumab discontinuation, which usually necessitates an alternative antiresorptive subsequent therapy [5]. Since osteoporosis is a chronic disease, most patients receive sequential therapies with both bisphosphonates and denosumab over the course of several decades, with or without temporary discontinuations (“drug holidays”) after bisphosphonate therapy. Thus far it remains unclear which antiresorptive agent is most effective regarding fracture risk reduction. In randomised controlled trials, denosumab was superior to alendronate in increasing BMD [6,7,8,9,10], and the transition from a bisphosphonate to denosumab was more effective in improving BMD than continuing with a bisphosphonate [11]. BMD is an important surrogate marker for fracture risk, and larger increases in BMD are associated with greater reductions in fracture risk, as observed across randomised controlled trials of osteoporosis therapies with different mechanisms of action [12, 13]. Still, head-to-head studies designed to compare the anti-fracture efficacy of denosumab with bisphosphonates are lacking. Most real-world studies have shown no significant difference in this regard, but they have often been limited by the use of indirect comparisons, short observational periods or missing information on BMD [14,15,16]. Thus, selection bias (different indication due to variable disease severity) might confound these findings.
We evaluated the anti-fracture effectiveness of bisphosphonates (zoledronate, ibandronate and alendronate) and denosumab in our patients in the osteoporosis registry of the Swiss Society of Rheumatology. This registry records not only fractures, including the time of their occurrence and their location, but also T-scores at different locations and trabecular bone scores (TBS) at the beginning of treatment and during follow-up. Hence, fracture risk can be adjusted for baseline BMD levels.
Methods
Study population
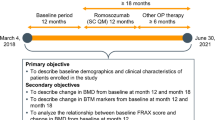
This study was conducted at a single non-academic outpatient centre in Switzerland, named OsteoRheuma Bern. Patients reviewed in this cohort study derive from a national register for osteoporosis maintained by the Swiss Society of Rheumatology [17, 18]. Subjects who were referred for a dual-energy X-ray absorptiometry (DXA) scan were consecutively enrolled in this registry. Eligible cohort members were patients followed from January 1, 2015, to September 30, 2019 who received denosumab, bisphosphonates or both sequentially. Retrospective data about past fractures and anti-osteoporotic therapies were collected in detailed face-to-face interviews, and like prospective data obtained after cohort entry, they were verified against referral information provided by each patient’s general practitioner. Patients were usually followed up by DXA scans every 1 to 3 years depending on their individual fracture risk and therapeutic strategy. Anti-osteoporotic drug therapy was administered in cases of fragility fracture or high fracture risk. The choice of medication was at the discretion of the treating physician, but there are certain constraints stipulated by the health authorities: In Switzerland, denosumab, zoledronate and ibandronic acid/ibandronate sodium can only be administered to patients with a fragility fracture and/or a T-score below -2.5 SD. In addition, denosumab can be prescribed to patients receiving hormone ablative therapy, regardless of fracture state or bone density. Alendronate has no restrictions and can be used in patients with osteopenia and no fractures.
The study was approved by the Ethics Committee of the Canton of Bern, Switzerland (KEKBE 2019–01037), and all subjects provided written informed consent.
Fracture assessment
Prior fracture history after the age of 50 years and new fractures during the follow-up period were recorded during structured face-to-face interviews, in addition to treatment modalities before and after cohort entry. Patients were seen at least every 1–3 years for a DXA scan that always included a vertebral fracture assessment. All clinical fractures after the age of 50 years were considered to be osteoporotic fractures; fractures of the fingers, toes and skull, as well as those associated with high-energy trauma, were excluded. Morphometric vertebral fractures were identified by vertebral fracture assessment using the semiquantitative method of Genant on lateral scans of the spine (Th6 to L4) [19]. Grade 2 and 3 vertebral fractures (≥ 25% loss of vertebral height) were recorded as morphometric vertebral fractures at baseline and during follow-up.
BMD assessment
BMD was measured at the lumbar spine (L1-L4), total hip and femoral neck. If patients could not be evaluated at one of these regions, additional measurement at the forearm was performed, and the BMD of the distal 1/3 radius of the non-dominant arm was recorded in the register. This was necessary generally in subjects with spine degeneration, metal spinal implants or bilateral hip replacements. TBS was measured in all patients after January 1, 2014 (the date that software evaluation of this score became possible). Hologic Delphi S/N 70197 C or GE Lunar Prodigy Pro “Full” JBO/557-C devices were used for all measurements (BMD, TBS and vertebral fracture analyses). In most cases (> 90%), each patient’s measurements were performed using the same device. A few patients underwent their baseline DXA scan outside our centre, and in these situations, we recorded these externally measured baseline T-scores in the registry.
Statistical analyses
We analysed the association of bisphosphonates (zoledronate, ibandronate and alendronate) and denosumab therapy with osteoporotic fractures at different sites (hip, vertebra, non-vertebra and other) in a time-to-event manner. This analysis included treatments as time-varying covariates in a Cox regression model, accounting for multiple events per patient. We modelled individuals with multiple fractures by indicating clusters of standard errors by patient in the regression model to account for the treatment at the time of fracture. Patients aged ≥ 50 years were considered at risk. We distinguished four different settings, specifically ‘before treatment onset’, ‘bisphosphonate therapy’, ‘denosumab therapy’ and ‘drug holidays’, and calculated hazard ratios (HRs) with 95% confidence intervals (CIs) using ‘before treatment’ as the reference and with standard errors to allow for intra-patient correlation. The time ‘before treatment onset’ refers to the specific period beginning at age 50 and before receiving therapy. In separate analyses, we compared bisphosphonates and denosumab in a similar way. As a sensitivity analysis, we stratified patient age into two 15-year ranges, specifically from 50 to < 65 years and from 65 to < 80 years, to check for different patterns over long-term follow-up. Proportional hazard assumptions were checked using Schoenfeld residuals. We further adjusted for age, gender, TBS, T-scores at different sites (lumbar spine, total hip, femoral neck and distal 1/3 radius) and use of glucocorticoids or aromatase inhibitors. Since BMD was not assessed at every site in all patients, we created 25 imputed datasets based on chained equations and conducted multiple imputations using T-scores at the lumbar spine, total hip, femoral neck, distal 1/3 radius, TBS and age. After multiple imputation, we calculated pooled chi-squared statistics based on Rubin’s rules to assess proportional hazard assumptions of the adjusted time-to-fracture analysis.
As an additional analysis, we used propensity modelling to construct two balanced treatment groups, namely ‘initial denosumab’ versus ‘initial zoledronate’, ‘initial ibandronate’ or ‘initial alendronate’. This model considered only the initial treatment, not subsequent therapies and/or drug holidays. Further, this model accounted for the time to first fracture only. The covariates included in the model were age, gender, use of glucocorticoids or aromatase inhibitors, prior vertebral or non-vertebral fractures and BMD (lumbar spine, total hip, femoral neck and distal 1/3 radius). We derived the balanced inverse probability of treatment weights by replacing weights that exceeded 10 with 10. For baseline characteristics, we calculated standardised differences between treatment groups. We calculated HRs with 95% CIs for every distinct outcome using Cox regressions of the inverse probabilities of treatment weights considering multiple events. In contrast to the main analysis, the observation time started with the initiation of treatment rather than at patient age 50. For this part of the analysis, we applied simple mean imputation to derive the inverse probability of treatment weights in cases of missing values. We performed statistical analyses using Stata 16 (StataCorp, College Station, TX, USA).
Results
Study cohort
The study cohort included 3068 subjects who received bisphosphonates, denosumab or both sequentially. They were consecutively enrolled between January 1, 2015 (the implementation date of the osteoporosis register of the Swiss Society of Rheumatology), and September 30, 2019. Of these patients, 2384 were first treated with a bisphosphonate, compared to 684 with denosumab. We analysed 11,078 observed patient-years for bisphosphonate therapy (41% alendronate, 36% ibandronate [28% intravenous ibandronic acid and 8% oral ibandronate sodium], 23% zoledronate) and 4216 for denosumab therapy. The median treatment duration was 2.8 years [2.2 to 4.7] for denosumab, 4.7 [2.7 to 6.5] for alendronate, 3.4 [2.2 to 5.3] for ibandronate and 2.1 [1.0 to 3.1] for zoledronate. A total of 48,375 patient-years were analysed after age 50 and before therapy was begun (‘time before therapy’), compared to 2593 patient-years of drug holidays (defined as the time between two treatment cycles) that had a median duration of 1.7 years [0.54 to 3.1]. The characteristics of all patients are shown in Table 1 according to the initial therapy (bisphosphonates or denosumab).
Fracture rates
In all 3068 patients, 2989 fragility fractures occurred after age 50. These included 1481 vertebral fractures (435 under therapy), 1508 non-vertebral fractures (499 under therapy) and 202 hip fractures (67 under bisphosphonates or denosumab). The fracture rates under bisphosphonates or denosumab, and those occurring during a drug holiday, are indicated in Table 2.
Fracture risks
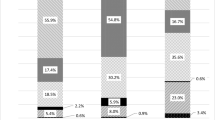
Crude hazard ratios for hip, vertebral, non-vertebral and any fractures, with hazards adjusted for age, gender, baseline T-scores (lumbar spine, femoral neck, total hip, distal 1/3 radius), TBS and use of glucocorticoids or aromatase inhibitors are shown in Table 3. These analyses indicate that all bisphosphonates and denosumab, in addition to drug holidays, were associated with a significantly decreased risk of any fractures (including vertebral, non-vertebral and hip fractures) compared to the fracture risk before treatment onset (after age 50). After adjusting for disease severity (namely age and baseline BMD) and/or differences between groups at baseline, denosumab was associated with lower risk than alendronate or ibandronate for vertebral fractures (aHR 0.47 (0.35 to 0.64) and 0.70 [0.53 to 0.91], p < 0.001 and p = 0.009, respectively) and any fractures (aHR 0.62 [0.51 to 0.76] and 0.77 [0.64 to 0.92], p < 0.001 and p = 0.004), but not for hip fractures. No difference in crude or adjusted fracture risk reduction was found between zoledronate and denosumab. (Fig. 1). In this multivariate regression model, patient age was significantly associated with the occurrence of any fractures. The baseline T-scores at the lumbar spine and distal 1/3 radius were significantly associated with the risk of vertebral, non-vertebral and any fractures, but not with hip fractures. In contrast, the baseline T-score at the femoral neck was associated with the hip fracture risk. TBS and male gender showed a significant association with the risk of vertebral fractures.
Fracture risk under denosumab versus bisphosphonates. This forest plot shows the fracture hazards (with 95% confidence intervals) under denosumab versus overall bisphosphonate therapy (A), ibandronate (B), alendronate (C) and zoledronate (D) with three statistical methods: Crude hazard ratios, adjusted hazard ratios (adjusted for age, BMD and TBS) and hazard ratios after inverse probability of treatment weighting. The crude and adjusted hazards considered all treatment sequences and all fractures, while the model using propensity weighting accounted for the first treatment sequence and time to first fracture. Abbreviations: BP: bisphosphonate, Dmab: denosumab, HR: hazard ratio, IPTW: inverse probability of treatment weighting
In the Cox regression models for crude or adjusted HRs, the proportional hazard assumption was violated for some fracture locations (mainly non-vertebral fractures). After adjusting for age, this violation was eliminated in most but not all cases. However, age might be one of the most important factors explaining the varying fracture risk observed across the wide range of ages in this study (age 50 to 80), apart from other factors like an increased imminent fracture risk after an index fracture or extraskeletal risk factors that change over time. We therefore analysed patterns after stratifying patient age into two 15-year ranges, namely from 50 to < 65 years and from 65 to < 80 years. Antiresorptive treatment was associated with significantly reduced fracture risk in older patients (> 65 years), but with a smaller reduction in younger ones (Table 4). In older individuals, bisphosphonates and denosumab both reduced hip fracture risk by about 60% and vertebral fracture risk by about 70–80%. Comparisons of fracture risk reduction in this older subgroup did not demonstrate a significant difference between bisphosphonate and denosumab treatment for any fracture location. This subanalysis, however, did not adjust for baseline BMD.
As an additional analysis, we used propensity modelling to compare the fracture risk under bisphosphonate versus denosumab (Suppl. Table 1). Of note, this model considered only the initial treatment, not subsequent therapies and/or drug holidays, and analyzed the time to first fracture only and not to subsequent fracture(s). After inverse weighting of treatment probabilities, denosumab was associated with a lower risk than alendronate and ibandronate in terms of vertebral fractures (HR 0.37 (0.28 to 0.49) and HR 0.55 (0.42 to 0.73), both p < 0.001) and any fractures (HR 0.38 (0.31 to 0.47) and HR 0.62 (0.50 to 0.76), both p < 0.001, respectively). Further, denosumab was associated with a lower risk of non-vertebral fractures compared with alendronate (HR 0.38 (0.29 to 0.50), p < 0.001) and ibandronate (HR 0.67 (0.50 to 0.89), p = 0.005). No difference in fracture risk reduction (vertebral, non-vertebral or hip) was found between zoledronate and denosumab. However, the hip fracture analysis showed a significant lower risk under denosumab compared to alendronate, HR 0.54 (0.29 to 0.98), p = 0.044) (Fig. 1). Thus, the findings in the propensity model are mostly consistent with the main analysis that used both therapies as time-varying covariates and adjusted the fracture hazards for baseline differences. The main differences were a significant risk reduction for non-vertebral fractures under denosumab compared to alendronate and ibandronate, and a significant hip fracture risk reduction under denosumab compared to alendronate, neither of which was found in the first analysis using time-varying co-variates.
Discussion
This registry-based cohort study of 3068 patients who received bisphosphonates (zoledronate, ibandronate and alendronate) or denosumab analysed the anti-fracture effectiveness of treatment after age 50. Overall, 67,169 observation-years were recorded, including 11,078 years of bisphosphonate therapy and 4128 years of denosumab therapy. A total of 2989 fragility fractures arose after age 50, and among them, 934 fractures occurred during antiresorptive therapies. The risks of vertebral, non-vertebral and hip fractures were significantly lower under any bisphosphonate, denosumab and drug holidays than before treatment onset. Crude and adjusted HRs, as well as HRs after propensity weighting, revealed a significant difference in vertebral fracture risk reduction between alendronate and denosumab as well as between ibandronate and denosumab. Further, denosumab was associated with a significantly lower hip fracture risk compared with alendronate (but not ibandronate or zoledronate) in the model that used propensity weighting. Hip fractures are associated with increased mortality, and therapies directed against further hip fractures improved survival [20]. Both alendronate and zoledronate are effective in preventing hip fractures [21,22,23]. Thus far, no real-world study or meta-analysis of clinical trials with fractures as a secondary outcome has shown that denosumab is superior to bisphosphonates regarding hip fracture reduction [9, 14,15,16, 24, 25]. Pedersen and colleagues identified no significant difference in hip fracture reduction between denosumab and alendronate within 3 years of follow-up in a Danish nationwide cohort study using healthcare data [15]. A real-life study of Adami and colleagues that retrieved clinical and densitometric data from a web-based fracture risk assessment tool also demonstrated no significant fracture risk reduction with denosumab compared with bisphosphonates [25]. Finally, a recent meta-analysis of randomised controlled trials found denosumab to be more effective than oral bisphosphonates in reducing the risk of vertebral but not hip fractures [26]. This is somewhat surprising as denosumab increases hip BMD to a greater degree than alendronate [10]. In addition, denosumab leads to continued increases in hip BMD for at least 10 years [27], which is not the case with bisphosphonates [28,29,30]. One reason why these studies did not show that denosumab was superior to bisphosphonates in preventing hip fractures might be the short treatment duration. The median duration of denosumab therapy in our study population was 2.9 years [2.2 to 4.7]. One might speculate that the superiority of denosumab in hip fracture risk reduction compared to bisphosphonates appears only after 3–5 years of therapy, as denosumab leads to continuous BMD increases at the total hip with a further reduction of non-vertebral fracture risk beyond 3 years of therapy [27, 31]. Further, hip fracture risk is also determined by extraskeletal factors (i.e., fall risk, co-medications and comorbidities, socioeconomic status and lifestyle factors), which might explain why the greater potency of denosumab with regard to improving BMD does not translate into higher effectiveness in reducing hip fracture risk.
The results of the three statistical models used to calculate fracture risk were generally consistent. However, while the correction for baseline fracture risk (in terms of age and baseline T-scores) changed the HR in the comparison between alendronate and denosumab, the difference was less pronounced for ibandronate versus denosumab and it was hardly present at all for the comparison of zoledronate versus denosumab. From a clinical point of view and in light of the reimbursement regulations in Switzerland, this is plausible, as zoledronate and denosumab are both preferred treatments in high-risk patients. Further, the model that used time-varying co-variates considered all treatment sequences (as well as drug holidays), while the model with inverse probability treatment weighting focused only on the first treatment sequence and the time to first fracture. The results of the two models were comparable, which might indicate that the therapy order (first bisphosphonate versus first denosumab) is not highly relevant in terms of fracture risk reduction. On the other hand, the baseline T-score at each location (lumbar spine, hip and radius) correlated with the fracture risk at the same site, which is a well-known association [32]. Our study also showed that fracture risk was lower during drug holidays compared to before treatment onset, supporting the rationale for a drug holiday after several years of bisphosphonate therapy [28, 29]. Of note, the vast majority of patients who discontinued denosumab in this study received subsequent bisphosphonate therapy [33]. Thus, only a small number of all vertebral fractures under bisphosphonate therapy occurred shortly after switching denosumab to bisphosphonates (< 3%). Administering bisphosphonates (usually zoledronate in this population) after denosumab seems to sufficiently prevent ‘rebound-associated’ vertebral fractures [34], although bisphosphonates do not fully prevent bone loss, particularly not after long-term denosumab [35]. This has to be taken into account when comparing the effectiveness of denosumab with bisphosphonates in the long-term management of patients with sequential treatments.
In previous studies with the same study population and observation time, we not only analysed treatment efficacy, but also the safety of bisphosphonates and denosumab. We found a higher risk of medication-related osteonecrosis of the jaw (MRONJ) in patients under denosumab (n = 12) versus bisphosphonates (n = 5), particularly in those receiving denosumab with prior bisphosphonate use (n = 9) [17]. On the other hand, there were only four cases of atypical femoral fracture (AFF) in the whole population, yielding no significant difference in patients treated with bisphosphonates versus denosumab [18]. When interpreting these safety outcomes in the context of the effectiveness of bisphosphonates and denosumab in this study, the treatment benefits of these antiresorptive agents outweigh the risks of MRONJ and AFF by far.
Limitations
Our observations have several limitations. First, residual confounding cannot be completely excluded, despite statistical corrections. We aimed to reduce bias with two different statistical approaches: utilising time-varying co-variates with adjustments for group differences and performing inverse weighting of treatment probabilities. Both models showed comparable results, which might suggest that there was no relevant confounding after adjusting. On the other hand, multiple testing increases the risk of type I errors, and our results need to be interpreted with caution. Second, the treatment durations may have been too short to analyse the effectiveness of both bisphosphonates and denosumab in terms of preventing hip fractures. Third, nearly half of the antiresorptive therapies and about 60% of the fractures were recorded retrospectively, and missing or false information cannot formally be excluded. However, these retrospective data were obtained directly from patients and from data provided by the patients’ general practitioners. Further, it can be assumed that it was more likely that previous fractures were forgotten than that additional fractures were erroneously reported. This means that the fracture rate in the period before inclusion or before the start of therapy would tend to be underestimated. However, our results show that the fracture risk during therapy was significantly lower than before treatment onset, so the risk of missed fractures was probably not very relevant and including these fractures would only increase the observed differences. Further, with respect to oral bisphosphonates (48% of all bisphosphonates), all information on treatment adherence was provided by patients. Thus, one reason for the higher efficacy of denosumab versus alendronate might be the better adherence to the parenterally administered denosumab [36]. This, however, would not explain the difference in terms of vertebral fracture risk reduction between denosumab and ibandronate, as ibandronate was mostly administered parenterally (78% intravenous, 22% oral). Finally, we did not use negative outcome control analyses to assess the comparability of the two treatment groups [37]. One important strength of this cohort study was the assessment of both fractures and BMD data. Most previous real-world studies relied on claim data and did not adjust for BMD, which is one of the most important surrogate marker of fracture risk. We also accounted for morphometric vertebral fractures (≥ 25% loss of vertebral height), which is important for managing patients with osteoporosis [38].
Conclusion
Among patients of age 50 years or older, the risks of vertebral, non-vertebral and hip fractures were lower under denosumab and/or bisphosphonate treatment than before treatment onset. Similarly, the risks of vertebral and non-vertebral fractures were lower during drug holidays than before treatment onset. Of note, the term ‘drug holiday’ is only relevant to bisphosphonate therapy, as denosumab should not be discontinued without subsequent treatment.
The anti-fracture effectiveness of both bisphosphonates and denosumab was particularly evident in older patients (> 65 years at treatment onset). After adjusting for baseline T-scores (lumbar spine, hip and distal 1/3 radius), age and other differences between groups, denosumab was associated with significant risk reduction compared to alendronate and ibandronate for vertebral fractures. Using propensity weighting, denosumab was associated with a lower hip fracture risk than alendronate. No difference in fracture risk reduction (vertebral, non-vertebral and hip fractures) was found between zoledronate and denosumab. Different statistical models showed comparable results, but nonetheless, residual confounding cannot formally be excluded and our findings need to be interpreted with caution.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
18 August 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00198-023-06887-4
References
Black DM, Rosen CJ (2016) Clinical Practice. Postmenopausal Osteoporosis. N Engl J Med 374(3):254–262. https://doi.org/10.1056/NEJMcp1513724
Shoback D, Rosen CJ, Black DM et al (2020) Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Guideline Update. J Clin Endocrinol Metabol 105(3):dgaa048. https://doi.org/10.1210/clinem/dgaa048
Drake MT, Clarke BL, Khosla S (2008) Bisphosphonates: Mechanism of action and role in clinical practice. Mayo Clin Proc 83(9):1032–1045. https://doi.org/10.4065/83.9.1032
Baron R, Ferrari S, Russell RGG (2011) Denosumab and bisphosphonates: Different mechanisms of action and effects. Bone 48(4):677–692. https://doi.org/10.1016/j.bone.2010.11.020
Tsourdi E, Langdahl B, Cohen-Sodal M et al (2017) Discontinuation of Denosumab therapy for osteoporosis: A systematic review and position statement by ECTS. Bone 105:11–17. https://doi.org/10.1016/j.bone.2017.08.003
Kendler DL, Roux C, Benhamou CL et al (2010) Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Min Res 25(1):72–81. https://doi.org/10.1359/jbmr.090716
Seeman E, Delmas PD, Hanley DA et al (2010) Microarchitectural deterioration of cortical and trabecular bone: differing effects of denosumab and alendronate. J Bone Miner Res 25(8):1886–1894. https://doi.org/10.1002/jbmr.81
Brown JP, Prince RL, Deal C et al (2009) Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: A randomized, blinded, phase 3 trial. J Bone Miner Res 24(1):153–161. https://doi.org/10.1359/jbmr.0809010
Lin T, Wang C, Cai X-Z et al (2012) Comparison of clinical efficacy and safety between denosumab and alendronate in postmenopausal women with osteoporosis: A meta-analysis. Int J Clin Pract 66(4):399–408. https://doi.org/10.1111/j.1742-1241.2011.02806.x
McClung MR, Lewiecki EM, Cohen SB et al (2006) Denosumab in Postmenopausal Women with Low Bone Mineral Density. New Engl J Med 354(8):821–31. https://doi.org/10.1056/NEJMoa044459
Miller PD, Pannacciulli N, Malouf-Sierra J et al (2020) Efficacy and safety of denosumab vs. bisphosphonates in postmenopausal women previously treated with oral bisphosphonates. Osteoporos Int 31(1):181–191. https://doi.org/10.1007/s00198-019-05233-x
Black DM, Bauer DC, Vittinghoff E et al (2020) Treatment-related changes in bone mineral density as a surrogate biomarker for fracture risk reduction: meta-regression analyses of individual patient data from multiple randomised controlled trials. Lancet Diabetes Endocrinol 8(8):672–682. https://doi.org/10.1016/S2213-8587(20)30159-5
Bouxsein ML, Eastell R, Lui LY et al (2019) Change in Bone Density and Reduction in Fracture Risk: A Meta-Regression of Published Trials. J Bone Miner Res 34(4):632–642. https://doi.org/10.1002/jbmr.3641
Zullo AR, Lee Y, Lary C et al (2021) Comparative effectiveness of denosumab, teriparatide, and zoledronic acid among frail older adults: a retrospective cohort study. Osteoporos Int 32(3):565–573. https://doi.org/10.1007/s00198-020-05732-2
Pedersen AB, Heide-Jørgensen U, Sørensen HT et al (2019) Comparison of Risk of Osteoporotic Fracture in Denosumab vs Alendronate Treatment within 3 Years of Initiation. JAMA Netw Open 2(4):e192416. https://doi.org/10.1001/jamanetworkopen.2019.2416
Choi NK, Solomon DH, Tsacogianis TN et al (2017) Comparative Safety and Effectiveness of Denosumab Versus Zoledronic Acid in Patients With Osteoporosis: A Cohort Study. J Bone Miner Res 32(3):611–617. https://doi.org/10.1002/jbmr.3019
Everts-Graber J, Lehmann D, Burkhard J-P et al (2022) Risk of Osteonecrosis of the Jaw Under Denosumab Compared to Bisphosphonates in Patients With Osteoporosis. J Bone Miner Res 37(2):340–348. https://doi.org/10.1002/jbmr.4472
Everts-Graber J, Bonel H, Lehmann D et al (2022) Incidence of Atypical Femoral Fractures in Patients on Osteoporosis Therapy – A Registry-Based Cohort Study. JBMR plus 6(10):e10681. https://doi.org/10.1002/jbm4.10681
Genant HK, Wu CY, van Kuijk C et al (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1148. https://doi.org/10.1002/jbmr.5650080915
Lyles KW, Colon-Emeric CS, Magaziner JS et al (2007) Zoledronic Acid and Clinical Fractures and Mortality after Hip Fracture. N Engl J Med 357(18):1799–1809. https://doi.org/10.1056/nejmoa074941
Black DM, Delmas PD, Eastell R et al (2007) Once-Yearly Zoledronic Acid for Treatment of Postmenopausal Osteoporosis. N Engl J Med 356(18):1809–1822. https://doi.org/10.1056/nejmoa067312
Black DM, Thompson DE, Bauer DC et al (2000) Fracture risk reduction with alendronate in women with osteoporosis: The fracture intervention trial. J Clin Endocrinol Metab 85(11):4118–4124. https://doi.org/10.1210/jcem.85.11.6953
Black DM, Cummings SR, Krapf DB et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348(9041):1535–41. https://doi.org/10.1016/s0140-6736(96)07088-2
Albert SG, Wood E (2021) Meta-Analysis of Clinical Fracture Risk Reduction of Antiosteoporosis Drugs: Direct and Indirect Comparisons and Meta-Regressions. Endocr Pract 27(11):1082–1092. https://doi.org/10.1016/j.eprac.2021.06.015
Adami G, Gavioli I, Rossini M et al (2022) Real-life short-term effectiveness of anti-osteoporotic treatments: a longitudinal cohort study. Ther Adv Musculoskeletal Dis 14:1759720X221105009. https://doi.org/10.1177/1759720X221105009
Händel MN, Cardoso I, von Bülow C et al (2023) Fracture risk reduction and safety by osteoporosis treatment compared with placebo or active comparator in postmenopausal women: systematic review, network meta-analysis, and meta-regression analysis of randomised clinical trials. BMJ. 381:e068033. https://doi.org/10.1136/bmj-2021-068033
Bone HG, Wagman RB, Brandi ML et al (2017) 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. https://doi.org/10.1016/S2213-8587(17)30138-9
Black DM, Schwartz A, Ensrud K et al (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial long-term extension (FLEX): A randomized tria 296(24):2927–38. https://doi.org/10.1001/jama.296.24.2927
Black DM, Reid I, Boonen S et al (2012) The effect of 3 versus 6 years of Zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Min Res 27(2):243–54. https://doi.org/10.1002/jbmr.1494
Bone HG, Hosking D, Devogelaer JP et al (2004) Ten years’ experience with alendronate for osteoporosis in postmenopausal women. New Engl J Med 18;350(12):1189–99. https://doi.org/10.1056/nejmoa030897
Ferrari S, Butler P, Kendler DL et al (2019) Further nonvertebral fracture reduction beyond 3 years for up to 10 years of denosumab treatment. J Clin Endocrinol Metabol 104(8):3450–3461. https://doi.org/10.1210/jc.2019-00271
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–9. https://doi.org/10.1136/bmj.312.7041.1254
Everts-Graber J, Reichenbach S, Gahl B et al (2021) Risk factors for vertebral fractures and bone loss after denosumab discontinuation: A real-world observational study. Bone 144:115830. https://doi.org/10.1016/j.bone.2020.115830
Burckhardt P, Faouzi M, Buclin T, Lamy O (2021) Fractures after denosumab discontinuation: a retrospective study of 797 Cases. J Bone Miner Res 36(9):1717–1728. https://doi.org/10.1002/jbmr.4335
Everts-Graber J, Reichenbach S, Gahl B et al (2022) Effects of zoledronate on bone mineral density and bone turnover after long-term denosumab therapy: observations in a real-world setting. Bone 163:116498. https://doi.org/10.1016/j.bone.2022.116498
Fatoye F, Smith P, Gebrye T, Yeowell G (2019) Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open 9(4):e027049. https://doi.org/10.1136/bmjopen-2018-027049>
McGrath LJ, Spangler L, Curtis JR et al (2020) Using negative control outcomes to assess the comparability of treatment groups among women with osteoporosis in the United States. Pharmacoepidemiol Drug Saf 29(8):854–863. https://doi.org/10.1002/pds.5037
Lems WF, Paccou J, Zhang J et al (2021) Vertebral fracture: epidemiology, impact and use of DXA vertebral fracture assessment in fracture liaison services. Osteoporosis Int 32(3):399–411. https://doi.org/10.1007/s00198-020-05804-3
Acknowledgements
We thank Dr René Zäch and Renate Bühler for their effort to maintain the osteoporosis register OP PF SGR, and Dr Mark Saadeh for proofreading the manuscript.
Funding
Open access funding provided by University of Bern OsteoRheuma Bern AG (intramural funding), with support from the Campus Stiftung Lindenhof Bern, Switzerland (Bonel_21-01_Netz_AFF).
Author information
Authors and Affiliations
Contributions
All authors were involved in data acquisition, analysis or interpretation, and in drafting the article or revising it critically for important intellectual content. All authors approved the final version to be submitted for publication. Study conception and design: JE, SR, TL. Acquisition of data: TL, JE, US, HRZ. Analysis and interpretation of data: JE, SR, DL, HB, HJH. BG and JE take responsibility for the integrity of the data analysis. The corresponding author attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Disclosures
JE, DL, BG, SR and TL have nothing to declare and no conflicts of interest. HB received consultancy fees from Novartis. HJH received occasional speaker’s fees from Amgen, Sandoz, Eli Lilly and Labatec. HRZ received consultancy fees from Abbvie, Celgene, Amgen and Mylan/Viatris. US received congress and travel expenses from Sandoz, Pfizer and Janssen Pharmaceutica, and consultancy fees from Novartis and Amgen.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These data were presented in part at the American Society of Bone and Mineral Research 2022 Annual Meeting in Austin, Texas, 9–12 September 2022.
The original online version of this article was revised: In this article the first reference in the Discussion section was incorrectly given as 19 but should have been 20. And all subsequent references (21 to 37) should have been one number higher.
The legend for Fig. 1 (B) and (C) were inadvertently swapped; the figure legend should have been “ibandronate (B), alendronate (C)”
The original article has been corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Everts-Graber, J., Bonel, H., Lehmann, D. et al. Comparison of anti-fracture effectiveness of zoledronate, ibandronate and alendronate versus denosumab in a registry-based cohort study. Osteoporos Int 34, 1961–1973 (2023). https://doi.org/10.1007/s00198-023-06863-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06863-y