Abstract
Summary
The role of integrating genomic scores (GSs) needs to be assessed. Adding a GS to recommended stratification tools does not improve the prediction of very low bone mineral density. However, we noticed that the GS performed equally or above individual risk factors in discrimination.
Purpose
We aimed to investigate whether adding a genomic score (GS) to recommended stratification tools improves the discrimination of participants with very low bone mineral density (BMD).
Methods
BMD was measured in three thoracic vertebrae using CT. All participants provided information on standard osteoporosis risk factors. GSs and FRAX scores were calculated. Participants were grouped according to mean BMD into very low (<80 mg/cm3), low (80–120 mg/cm3), and normal (>120 mg/cm3) and according to the Bone Health and Osteoporosis Foundation recommendations for BMD testing into an “indication for BMD testing” and “no indication for BMD testing” group. Different models were assessed using the area under the receiver operating characteristics curves (AUC) and reclassification analyses.
Results
In the total cohort (n=1421), the AUC for the GS was 0.57 (95% CI 0.52–0.61) corresponding to AUCs for osteoporosis risk factors. In participants without indication for BMD testing, the AUC was 0.60 (95% CI 0.52–0.69) above or equal to AUCs for osteoporosis risk factors. Adding the GS to a clinical risk factor (CRF) model resulted in AUCs not statistically significant from the CRF model. Using probability cutoff values of 6, 12, and 24%, we found no improved reclassification or risk discrimination using the CRF-GS model compared to the CRF model.
Conclusion
Our results suggest adding a GS to a CRF model does not improve prediction. However, we noticed that the GS performed equally or above individual risk factors in discrimination. Clinical risk factors combined showed superior discrimination to individual risk factors and the GS, underlining the value of combined CRFs in routine clinics as a stratification tool.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major health problem due to low diagnostic rates and disease-related consequences, such as osteoporotic fractures and increased mortality. Despite being a frequent and preventable disease, screening tests and referral to diagnostic tests have not increased diagnostic rates sufficiently [1, 2].
Quantitative computed tomography (CT) is a relatively new promising method for identifying high-risk individuals using CT scans to quantify bone mineral density (BMD). BMD is a well-known surrogate marker of osteoporosis [3]. Opportunistic screening using CT scans has the benefits of using pre-existing scans made for various clinical indications. We have recently demonstrated that spine BMD measured from routine cardiac CT scans is associated with fracture rate in a large group of individuals referred to cardiac CT [4]. Furthermore, we have documented that a substantial proportion of individuals (179/1487; 12%) referred to routine cardiac CT have very low BMD (thoracic spine BMD<80 mg/cm3) [5]. These findings suggest a feasibility using CT for opportunistic screening to increase diagnostic rates and identify high-risk osteoporotic individuals.
Current screening guidelines differ between countries and in lack of validated screening strategies, individual risk stratification is often based on identifying osteoporosis risk factors [6, 7]. The Fracture Risk Assessment tool (FRAX) can be used to assess an individual’s absolute 10-year fracture probability based on clinical risk factors with or without BMD measurements [8]. Recently, a randomized controlled trial has shown the benefits of using FRAX to screen women for further BMD assessment and pharmacological treatment by reducing hip fractures [9], underlining the clinical value of screening using FRAX.
However, the ability of FRAX to discriminate between men with fractures versus men without fractures is limited [10]. Screening using either a model including risk factors for osteoporosis or FRAX could possibly be improved by adding the individuals’ inherent risk of osteoporosis, especially in individuals otherwise not identified using standard screening tools.
Osteoporosis is a polygenic disease associated with a strong heritability (twin study-based H2-estimates range between 0.77 and 0.89 for lumbar and femoral neck BMD [11]); hence, family predisposition is a strong independent risk factor for osteoporosis [12, 13]. Genome-wide association studies (GWASs) have identified numerous genetic variants associated with BMD and/or osteoporotic fractures [14,15,16,17] from which a genomic score (GS) can be constructed [18]. The GS, also known as a polygenic score, is the sum of common alleles an individual carries weighted by the single nucleotide polymorphism (SNP) effect size estimated from GWAS. A GS could be a promising tool to identify patients with very low BMD otherwise invisible in the daily clinic. BMD measurements are accessible and relatively cheap; however, patients with osteoporosis often go undiagnosed. Research in genetic risk profiling and focus on personalized medicine have increased in recent years and could be a valuable tool for assessing the risk of very low BMD in the future. However, the clinical role of integrating GSs in medical clinics to improve the selection of individuals for BMD testing needs to be further assessed. We hypothesize that a GS adds value to the identification of patients with very low BMD based on a clinical risk factor model.
Therefore, the aim of this study was to investigate whether adding GS to recommended stratification tools improves the discrimination of participants with very low BMD.
Material and methods
Study design and study participants
This cross-sectional sub-study of the multicenter Danish Study of Non-Invasive Diagnostic Testing in Coronary Artery Disease (Dan-NICAD) included participants (n=1675) referred to a cardiac CT between September 2014 and March 2016 at two centers. All participants had an indication for a coronary CT angiography, a low to intermediate risk profile of coronary artery disease (CAD), and did not have a history of CAD. Inclusion and exclusion criteria have previously been reported [19]. All participants gave written, informed consent before enrolment.
The Central Denmark Regional Committee on Health Research Ethics (date: 2014-07-30, ref.: 1-10-72-190-14) and the Danish Data Protection Agency (ref.: 1-16-02-345-14) approved this study. The trial was registered at ClinicalTrials.gov (NCT02264717). The study followed the principles of the World Medical Association Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects.
Image acquisition and BMD analyses
All participants were referred for routine cardiac CT on the clinical indication of CAD. Using the non-enhanced cardiac CT, a mean BMD was analyzed by an experienced reader (Josephine Therkildsen (JT)) blinded to participant data for every participant based on three consecutive thoracic vertebrae beginning from the left main coronary artery. The selected thoracic vertebrae have previously been demonstrated to include Th6 (11%), Th7 (48%), Th8 (37%), and Th9 (4%) [20]. The Mindways QCT Pro software (Mindways Software Inc, TX) was used to measure BMD together with the calibration phantom, Mindways Solid 3 (Mindways Software Inc, TX) as previously described [5]. The mean BMD was grouped as very low (<80 mg/cm3), low (80–120 mg/cm3), and normal BMD (>120 mg/cm3) as described by the American College of Radiology (ACR) for lumbar spine QCT [21].
Osteoporosis risk factors
During interviews at the baseline visit and from electronic patient records, trained study nurses obtained information on self-reported osteoporosis risk factors including age, sex, smoking status, alcohol history, and family predisposition for osteoporosis (1-degree relatives having osteoporosis or a history of hip fractures). Anthropometric measurements, such as weight and height, were also obtained.
Danish Patient Registries were used to collect history of previous fractures, both any type of fracture and osteoporosis-related fractures (hip, spine, forearm, and proximal humerus fracture), use of glucocorticoids and anti-osteoporotic treatment, and known diseases to calculate Charlson comorbidity index as previously reported [4].
Using the Bone Health and Osteoporosis Foundation (BHOF), formerly known as the National Osteoporosis Foundation, recommendations for BMD testing, participants were divided into an “indication for BMD testing” and a “no indication for BMD testing” group. The categorization was based on [1] age + sex (age cutoff in women ≥ 65 years and men ≥ 70 years irrespective of osteoporosis risk factors) and [2] age + sex + clinical risk factors (postmenopausal women and men older than age 50 years with clinical risk factors which here includes body mass index<20 kg/m2, previous osteoporosis-related fracture, family history of osteoporosis, active smoking, glucocorticoid treatment within the previous 6 months, and secondary osteoporosis (here defined as diabetes mellitus type 1, early menopause < 45 years of age or Charlson comorbidity index ≥2)) [22].
FRAX calculation
The FRAX tool estimates the 10-year probability of fracture (hip and major osteoporotic fracture) (https://www.sheffield.ac.uk/FRAX/tool.aspx?country=29). A previous osteoporosis-related fracture was defined as a previous fracture at the hip, spine, proximal humerus, or forearm registered in the National Danish Patient registry using the 10th edition of the International Classification of Diseases [23] as previously reported [4]. Participants were asked if they were predisposed to osteoporosis, including 1-degree relatives having known osteoporosis or a history of hip fractures. Current systemic glucocorticoid use was defined as a redeemed prescription within 6 months prior to the baseline visit. All participants with self-reported or known rheumatoid arthritis, Crohn’s disease, colitis ulcerosa, osteogenesis imperfecta, severe scoliosis, Scheuermann’s disease, lymphoma, leukemia, or myelomatosis were excluded from BMD analyses; thus, these risk factors were considered as not present for the entire cohort. Secondary osteoporosis was defined as diseases strongly associated with osteoporosis (type 1 diabetes mellitus, early menopause (<45 years), or Charlson comorbidity index ≥ 2). Consumption of alcohol in units/day was not recorded; however, participants with chronic alcoholism were excluded from BMD analyses, and so the risk of alcohol consumption ≥ 3 units/day was considered as not present for the entire cohort. In general, there were a few missing values for osteoporosis risk factors (Table 1 legends). If a participant had a missing risk factor, the FRAX score was recorded as missing (n=32). Seven participants had a weight above 125 kg, and as FRAX only allow a maximum weight of 125 kg to be included, these participants were regarded as having a weight of 125 kg.
Genomic scores
All participants had blood samples collected (4 mL EDTA whole blood) at baseline for genotyping. DNA was extracted, and only high-quality DNA was used for genotyping using the Illumina Global Screening Array (Illumina, Inc., 5200 Illumina Way, San Diego, CA) at deCODE genetics (deCODE genetics, Inc., Reykjavik, Iceland). Quality control was performed with Plink 1.9 [24] removing samples and SNPs with missingness <0.02, sex discrepancy, minor allele frequency <0.01, and deviation from Hardy-Weinberg equilibrium (p<1 × 10−6), which resulted in a total of 310,531 autosomal SNPs. Furthermore, first and second-degree relatives were identified based on identity by descent (\(\hat{\pi}\)>0.2), and ancestral outliers were identified by multidimensional scaling, which in total removed 27 samples. Genotypes were imputed using the Michigan Imputation Server [25] (reference panel HRC: r1.1.2016 GRCh37). SNPs with a minor allele frequency below 0.01, missing genotype rate >5%, deviation from Hardy-Weinberg equilibrium (p<1 × 10−6), imputation quality below 0.9, and SNPs located within the major histocompatibility complex (MHC; 6p22.1–21.3: chr6:28,477,797-33,448,354, GRCh37) were removed, resulting in a total of 6,565,335 autosomal genetic variants, with positions annotated to genome build GRCh37.
The GS was computed based on a GWAS meta-analysis assessing total body (TB) BMD (GSTB_BMD) as measured by dual-energy X-ray absorptiometry (DXA) in 66,628 individuals compromising of 86 % European ancestry, 2% African American, and 14% from admixed background [17].
The GSTB_BMD was predefined as the primary GS based on an available full GWAS summary statistic.
Two other GSs (GSFN_BMD and GSHQ_SOS) were constructed and compared with the primary GSTB_BMD (Supplementary Table S1). The summary statistics for the GSFN_BMD were based on a GWAS meta-analysis assessing femoral neck (FN) BMD measured by DXA in 32,961 individuals with populations from both Europe, America, East Asia, and Australia [14]. Only 54 SNPs associated with BMD were publicly available. Finally, the GSHQ_SOS was based on 11,709 SNPs from a study assessing heel quantitative ultrasound speed of sound (HQ_SOS) in 341,449 individuals mainly of white British ancestry [15].
The GSs were computed based on genetic markers pruned for linkage disequilibrium (r2<0.9) as \(GS=\sum_{i=1}^m{X}_i{\hat{\beta}}_i\), where Xi is the ith genotype encoded as 0, 1, or 2 counting the number of the first allele in the bim-file, and \({\hat{\beta}}_i\) is the marker effects of the ith marker. Each GS was computed using different SNP P value thresholds (0.001, 0.01, 0.1, 0.5, 0.7, 0.9) to find the optimal GS performance. Processing of the genetic data and computing the GS were performed with the R package qgg [26, 27].
Participants were divided into three groups based on their GSTB_BMD; low (0–20% percentile), average (20–80% percentile), and high (80–100% percentile) comparable to previous reported results [28].
Statistical analysis
All GS scores were standardized to a mean of zero and a standard deviation (SD) of one. Demographics at baseline were compared by GS groups (low, average, and high) using a one-way analysis of variance, Kruskal-Wallis test, or Fischer’s exact test. Data are presented as a number with a percentage for categorical variables, as a mean with SD for normally distributed continuous variables, or as a median with an interquartile range for not normally distributed continuous variables.
The correlations between the GS and mean BMD, together with the GS and osteoporosis risk factors, were estimated using Pearson correlation, Spearman correlation, or logistic regression coefficients.
Four different logistic regression models were used to estimate odds ratio (OR) (and 95% confidence intervals) for having very low BMD (yBMD, defined as mean BMD <80 mg/cm3 as described by ACR [21]):
Model (2 and 3) was based on a combined model for clinical risk factors (CRF) which included: age, sex, BMI, active smoker, osteoporosis disposition, previous osteoporosis-related fracture, glucocorticoid treatment, and secondary osteoporosis. The GS and BMI were multiplied with −1, as an inverse association with mean BMD was present and statistical tests assume higher values indicating higher risk. The ORs presented in Table 2 are per 1 SD in GS standardized to the current dataset using z scores.
Using logistic regression, the CRF and CRF-GS models were compared using the likelihood ratio test. We evaluated each model’s ability to discriminate participants having very low BMD using area under the receiver operating characteristic curve (AUC). Furthermore, we evaluated the ability of reclassifying participants using the CRF model vs. the CRF+GS model using pre-test probability cutoff values of 6%, 12%, and 24% [29]. These cutoff values were based on the prevalence (p) of having very low BMD (12%) in the total cohort, by calculating p/2, p, and 2p, as recommended when clinical cutoff values do not exist [30]. The net reclassification index (NRI) and integrated discrimination improvement (IDI) were calculated. In order to internally validate the CRF and CRF+GS model, we compared AUCs with the FRAX and FRAX+GS model (not fitted to the current study [31]) and tested AUCs using 5-fold cross-validation [32]. A P value<0.05 was considered statistically significant and in multiple comparisons, P values were adjusted according to the Bonferroni adjustment (P value/ntests) when relevant. Sample size calculation has previously been published [19]. All analyses were performed using STATA/IC 17.0 (StataCorp, College Station, Tex).
Results
Study population
In total, 1421 participants (672 men, 749 women) had BMD measurements and GS available. The participant flowchart is displayed in Fig. 1. The mean age for the total population was 57 ± 9 years (range 40–79 years). Baseline characteristics stratified by GS groups are shown in Table 1. Baseline characteristics stratified by clinical indication for BMD testing are presented in Supplementary Table S2.
Study participant flowchart. In seven participants, the non-enhanced cardiac CT (used for BMD measurements) was not performed based on a pre-test individual clinical risk assessment. In 181 participants, BMD measurements were excluded due to technical or participant-related factors known to affect BMD measurements. In 66 participants, no GSs could be made, as genotyping from blood samples was not performed. The final study population consisted of 1421 individuals with both BMD and GS available. Abbr.: CT computed tomography, BMD bone mineral density, GS genomic score
Genomic score—the association with BMD
Participants having low GS (0–20%) were more likely to have a family history of osteoporosis (P<0.01), known osteoporosis (P<0.001), to take anti-osteoporotic medication (P<0.05), have very low BMD (P<0.01), and a higher median FRAXMOF score (P<0.05) compared to the average (20–80%) and high (80–100%) GS group (Table 1). Furthermore, subdividing GS showed that extremes affected mean BMD and prevalence of very low BMD (Supplementary Figure S1 and S2).
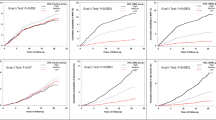
Assessing three different genomic scores, GSTB_BMD and GSHQ_SOS showed significant associations to mean BMD but the GSFN_BMD did not (Supplementary Table S1). Overall, a greater GSTB_BMD was associated with higher BMD in both men and women (Fig. 2) with a 3 % of the variance in the mean BMD explained by the GS. The GS was not statistically significantly correlated with osteoporosis risk factors, except for family predisposition in women likely capturing the inherited risk (Supplementary Table S3). GS and mean BMD were overall correlated across age and BMD groups, suggesting its predictive value irrespectively of age and BMD groups (Supplementary Table S4).
Scatter plot of the association between BMD and the GS. The association between mean BMD and GSTB_BMD (P<0.001) in men (blue crosses, fitted blue line) and women (red crosses, fitted red line). Pearson correlation coefficients for men and women were r = 0.17 (P<0.0001) and r = 0.18 (P<0.0001). Abbr.: BMD bone mineral density, GS genomic score
Genomic score—discrimination of participants with very low BMD
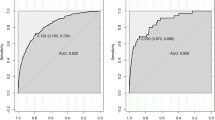
The GS showed a similar ability in identifying participants having very low BMD compared to standard clinical risk factors as displayed by the AUC in the total cohort and in participants with indication for BMD testing (Fig. 3A and Supplementary Figure S3). In the total cohort, the AUC for the GS was 0.57 (95% CI 0.52–0.61) not statistically different from the AUCs for individual risk factors (P=0.39). However, in participants without indication for BMD testing (n=841), the AUC for the GS alone (0.60 [95% CI 0.52–0.69]) performed above some individual clinical risk factors (sex, active smoking, and secondary osteoporosis, all P<0.0063) and equally for previous osteoporosis-related fracture, family predisposition, BMI, and glucocorticoid treatment (all P>0.0063); Bonferroni correction (0.05/8=P<0.0063) (Fig. 3B).
Discrimination of very low BMD stratified by indication for BMD testing. The area under receiver operating curves (AUC) using osteoporosis risk factors, the GS, and FRAX for discriminating participants having very low BMD stratified by indication for BMD testing as recommended by the Bone Health and Osteoporosis Foundation based on age, sex, and clinical risk factors [22]. In total, 580 participants indicated BMD testing (A) and 841 participants did not (B). AUC between the individual osteoporosis risk factors (including GS) was not statistically different in participants with indications for BMD testing (P=0.47). However, in participants without indication for BMD testing, the AUC for GS alone performed above some individual clinical risk factors (sex, active smoking, and secondary osteoporosis, all P<0.0063) and equally for previous osteoporosis-related fracture, family predisposition, BMI, and glucocorticoid treatment (all P>0.0063). Bonferroni correction (0.05/8=P<0.0063). Adding the GS to the FRAX and CRF model did improve the AUC, except for adding the GS to the FRAX in the group without indication for BMD testing; however, this was not statistically significant (all P>0.05). The GS and BMI were included as a continuous variable multiplied by −1, as higher values, thus indicating a higher risk. Abbr.: AUC area under receiver operating curves, BMD bone mineral density, BMI body mass index, CI confidence intervals, CRF clinical risk factors, FRAX (MOF) the 10-year probability of major osteoporotic fractures calculated by the Fracture Risk Assessment tool (without BMD), GS genomic score
Per one SD decrease in GS, the odds of having very low BMD were increased by 34% (Table 2). Subgroup analyses including women vs men showed similar results (Table 2). In participants without indication for BMD testing, OR for very low BMD per SD decrease was 1.56 (95% CI 1.18–2.07, P<0.01) compared to 1.24 (95% CI 1.02–1.50, P<0.05) in participants with an indication for BMD testing.
No improvements in net reclassification nor the integrated discrimination were detected when adding the GS to the CRF model using predefined probability cutoff values of 6%, 12%, and 24% in participants without an indication for BMD testing (Table 3). We observed a few individuals without very low BMD being misclassified using the CRF+GS model (n=3) (Table 3). Furthermore, no improvements were detected in participants with an indication for BMD testing or for the total cohort (Supplementary Table S5 and S6).
To assess the possible benefits of using GS for risk stratification, we assessed the effect of including the GS in the stratification algorithm as recommended by BHOF (Supplementary Figure S4). In total, 841 individuals did not have an indication for BMD testing based on standard stratification tools; however, 54 cases with very low BMD (6%) fell into this category. A number of cases that would be screened if incorporating the low GS in risk stratification are n=150, with a possibility to identify 17 more cases with very low BMD.
Prediction models—discrimination of very low BMD
The likelihood-ratio test showed a significant improvement of adding the GS to clinical risk factors (P<0.001). Subsequently, a CRF model including clinical risk factors (age, sex, BMI, active smoking, family history of osteoporosis, previous osteoporosis-related fracture, glucocorticoid treatment, and secondary osteoporosis) was developed to predict very low BMD using all available participants. Analysis of the model’s ability to discriminate very low BMD showed an AUC of 0.78 (95% CI 0.74–0.81). Next, a CRF+GS model was developed adding the GS to the clinical risk factor (CRF+GS) model resulting in an AUC of 0.78 (95% CI 0.75–0.81). Directly comparing AUCs did not show statistically significant improvement from the AUC for the CRF model alone (Supplementary Figure S3).
In participants without indication for BMD testing, adding GS to a clinical risk factor (CRF) model resulted in an AUC of 0.80 (95% CI 0.75–0.85) not statistically significant from the CRF model alone. AUCs stratified by indication for BMD testing are shown in Fig. 3.
Internal validation of the CRF and CRF+GS model is shown in Supplementary Figure S5. The models overall showed good calibration, although the CRF+GS model showed a tendency of better calibration at higher risks compared to the CRF model alone.
We computed the AUCs for the FRAXMOF and a FRAXMOF+GS model (0.73 [95% CI 0.69–0.77] and 0.72 [95% CI 0.68–0.76]), including the same risk factors as the CRF model, but without being fitted to the current study population (Supplementary Figure S3).
A five-fold cross-validation revealed AUCs for the CRF and CRF+GS model of 0.77 (95% CI 0.73–0.81) and 0.77 (95% CI 0.73–0.81), suggesting a small over-fitting but without affecting the difference in AUCs between the models.
Discussion
In the present study, the GS was weakly associated with mean BMD as measured from cardiac CT scans (Supplementary Table S1). Nonetheless, the GS showed equal or greater discrimination than standard clinical risk factors, especially in participants without an indication for BMD testing. In participants without an indication for BMD testing, odds for having very low BMD per SD decrease in GS was 1.56 (95% CI 1.18–2.07, P<0.01) compared to 1.24 (95% CI 1.02–1.50, P<0.05) in participants with an indication for BMD testing. However, when performing reclassification analyses, no significant improvements in prediction were detected adding the GS to the CRF model in the total cohort nor in subgroup analyses inconsistent with our stated hypothesis.
Despite not detecting any statistically significant improvement in the combined model’s AUCs, a new predictor may add valuable improved prediction, as AUC is not sufficient to fully assess model performance. Often, despite improving the performance of a model, the increase in AUC is likely very small [29]. Furthermore, despite not adding statistically significant value, the combination of several risk factors can add value to prediction [33]. Therefore, we performed a reclassification analysis to further assess the contribution of the GS as a novel variable in risk assessment for identifying participants with very low mean BMD. To our knowledge, no other studies have assessed the clinical utility of adding a GS in a stratification algorithm to identify participants having very low BMD as measured from CT.
There is a need to assess the clinical relevance of genetic profiling, as recent developments have resulted in low costs and fast routine assessment of genetic profiles being available, making personalized disease-preventive measures possible. If GS becomes a routine assessment, the genetic risk of very low BMD could be evaluated if indicated and requested by the clinician and the patient.
Our primary outcome was quantitative CT-measured BMD; however, GWASs have primarily focused on DXA- or ultrasound-measured BMD and fracture risk [14, 16, 17], and to our knowledge, no GWAS have been conducted on CT-measured BMD. As differences in BMD measurements exist regarding units and measurement sites, this could reduce the discriminative performance of the GS and GS-combined models in this study. BMD of the femoral neck by DXA is used to diagnose osteoporosis, but total body BMD and BMD measured by ultrasound are not recommended for diagnosis according to the World Health Organization [34]. However, we compared different genomic scores derived from these measurement sites (GSTB_BMD, GSFN_BMD, and GSHQ_SOS), including BMD femoral neck, in order to assess this in our study population and in a clinical context. We predefined the GSTB_BMD as our primary GS as it was based on a fully available GWAS summary statistic, and the GSTB_BMD (P<0.001) was selected for further analyses based on its strongest association to mean BMD in comparison to the other P value thresholds (Supplementary Table S1). There are numerous ways to calculate GSs [35], and our results are limited to this specific GS limiting generalizability to other GSs. The overall effect size of identified genetic variants is small, suggesting at present that GSs for prediction of fracture or low BMD alone have limited predictive power [36]. However, a GS may still be of clinical relevance combined with other clinically relevant predictors to fully capture the polygenic nature of osteoporosis. Furthermore, when GWASs for BMD further expand, the predictive power for discriminating disease likely increases.
It is important to assess both BMD-specific GSs (based on GWASs for BMD) and fracture-specific GSs (based on GWASs for fracture) to assess the relevance in a clinical context and for patient care. Individuals with BMD T score>-2.5 and no osteoporosis risk factors do not generally have an indication for specific anti-osteoporosis treatment, despite most fragility fractures occur in individuals without osteoporosis [37, 38]. This fact highlights the need to optimize the identification of individuals at high fracture risk, who are otherwise overlooked. A BMD-specific GS can potentially help identify inherited very low BMD, and thus, high fracture risk, in younger individuals without clinical risk factors. Despite limited research in the management of osteoporosis in younger adults, it seems likely that these individuals represent a patient group, where diagnosis and early treatment may impact positively the quality of life [39]. Furthermore, these young patients are likely to be missed using standard clinical stratification tools. Further research in screening, treatment, and prediction of fractures in younger adults is warranted.
Recent studies suggest adding a GS in osteoporosis screening could reduce the number of patients who need BMD testing and improve overall fracture risk prediction [15, 16, 40]. Due to differences in clinical outcomes and designs, it is challenging to directly compare our results with other studies. Ho-Le et al. (2017) assessed the predictive value of a BMD-associated genetic score for the incidence of radiographically verified fragility fractures. They documented that the genetic score improved the accuracy of fracture prediction above clinical risk factors [40]. Our primary outcome was CT-measured BMD, a surrogate marker of fracture risk, limiting direct comparison of outcomes. However, we have previously shown that CT-measured BMD in our cohort is associated with greater fracture rate, both incident osteoporosis-related fracture and any fracture, documenting the clinical feasibility of CT-measured BMD in predicting fractures across a broad age range [4]. Lu et al. (2021) assessed a genetic score for heel quantitative speed of sound, which they found to improve fracture risk prediction above traditional clinical risk factors when adding it to FRAX. The clinical cutoff was set at 20% and 3% for the prediction of major osteoporotic fractures and hip fractures, based on the indication for treatment as recommended by the BHOF [16]. Our primary GS was based on total body BMD as previously described and we assessed a CRF model vs CRF-GS model using cutoff values at 6%, 12%, and 24 %. As the reclassification analysis is highly dependent on the cutoff values used, this limits direct comparison. We used FRAX as a reference platform to identify individuals at risk, as this model is validated for fracture probability, included in clinical guidelines and not fitted to the current study data [41]. However, FRAX does not identify very low BMD, but asses fracture risk and so, our primary focus was a clinical risk factor model including known osteoporosis risk factors. Having differences in outcome and designs in mind, we could not confirm previous findings suggesting adding a GS to recommended stratification tools could be of use in osteoporosis screening for personalized risk assessment.
The aim of adding a GS is to identify patients, who will benefit from interventions including medical treatment that will reduce fracture risk. Preventive interventions are especially cost-effective in high-risk individuals [42]. Based on our data, we found no benefit of adding a GS to a CRF model. Although DXA will likely always be favorable in availability and costs, future GSs might increase awareness of many silent diseases by identifying high-risk individuals. We noticed that the GS model performed equally or above individual clinical risk factors in discriminating individuals with very low BMD. This suggests that if general genetic profiling of the population or subgroups of the population becomes more common, a GS might be of value in identifying individuals at risk otherwise overlooked. The combined clinical risk factor model (and FRAX) showed superior discrimination to individual risk factors and the GS, underlining the value of combined CRFs in routine clinics as a stratification tool.
Our results highlight the need to carefully evaluate the benefits of new predictors in different cohorts using different study designs before implementation.
Strengths and limitations
The strengths of this study include the consecutive inclusion of a homogenous study population of both men and women at two centers. Participants had free access to medical attention and were referred to cardiac CT by experienced cardiologists, limiting possible selection bias. All participants had relevant and extensive osteoporosis risk factors collected at their baseline visit and a trained reader (JT) performed BMD analyses and calculated FRAX for all participants. BHOF releases comprehensive recommendations to guide clinicians to prevent and treat osteoporosis worldwide, including guidelines for BMD testing [22], and despite country-specific guidelines, we used these recommendations for a stratification algorithm to assess the GS in a clinical setting.
Limitations include the following: [1] Only participants with European ancestry referred to cardiac CT were included; thus, the results from this study may not be extrapolated to other cohorts. [2] FRAX includes previous fractures (defined as spontaneous or low-energy fractures in adult life). However, we defined a previous osteoporosis-related fracture based on diagnostic codes from Danish registries recorded at Danish hospitals since 1995. These registries do not differentiate low- from high-energy fractures, nor could we include non-clinical fractures, such as vertebral fractures only detected on imaging or vertebral fractures without imaging. Participants were asked if they were predisposed to osteoporosis, including 1-degree relatives having osteoporosis or a history of hip fractures, and this was entered into the FRAX tool. Thus, a history alone describing parental hip fracture was not recorded despite being used in the FRAX tool. Current systemic glucocorticoid use was defined as a redeemed prescription recorded 6 months prior to the baseline visit; however, the FRAX tool defines use as either currently using or exposed for 3 months of minimum 5 mg daily. Secondary osteoporosis was here defined as type 1 diabetes mellitus, early menopause (<45 years), or a Charlson comorbidity index ≥ 2. Although the FRAX tool does not include a Charlson comorbidity index in its users’ guide, this was chosen to include diseases with a known increased fracture risk [41] comparable to the clinical risk factor model. [3] Lumbar and thoracic spine BMD values show high correlations [20], but currently, only lumbar QCT BMD is recommended [43]. CT-measured thoracic BMD is a surrogate marker of fracture risk, currently not included in clinical guidelines to diagnose osteoporosis [20, 43]. Despite BMD being the strongest individual predictor of fracture risk, the developed models’ ability to predict future fractures needs to be assessed. In the lack of validated thoracic BMD cutoff values, we chose ACR’s recommended lumbar spine BMD cutoff values for very low and low BMD. This likely underestimates the very low and low BMD group due to physiological differences in BMD values between the thoracic and lumbar spine [44]. [4] In the lack of relevant clinical cutoff values, predefined cutoff values of 6%, 12%, and 24% were chosen according to the calculated p/2, p, and 2p as described by Cook et al. (2011) [30]. The results of the reclassification analyses were dependent on these cutoff values.
We performed cross-validation, as model synthesis tested in the original dataset tends to optimistic estimate the predictive performance [45]. Our analysis showed a more realistic estimate with the tendency of a slight over-fitting, however not affecting the overall results. As our models were developed and assessed in the same study population, there is a need to externally validate the results of this study in an independent cohort to fully assess the generalizability of the results.
In conclusion, adding a GS to a clinical risk factor model did not improve the overall prediction of very low BMD. However, we noticed that the GS performed equally or above individual risk factors in discrimination. Clinical risk factors combined showed superior discrimination to individual risk factors and the GS, underlining the value of combined CRFs in routine clinics as a stratification tool.
Data availability
The data supporting the results of this study is not publicly available due to privacy or ethical restrictions.
Abbreviations
- ACR:
-
American College of Radiology
- AUC:
-
Area under the receiver operating characteristics curve
- BHOF:
-
Bone Health and Osteoporosis Foundation
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- CRF:
-
Clinical risk factors
- CT:
-
Computed tomography
- DXA:
-
Dual-energy X-ray absorptiometry
- FRAX:
-
Fracture Risk Assessment Tool
- GS:
-
Genomic score
- GWASs:
-
Genome-wide association studies
- IDI:
-
Integrated discrimination improvement
- MOF:
-
Major osteoporotic fractures
- NRI:
-
Net reclassification improvement
- SD:
-
Standard deviation
References
Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J et al (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137. https://doi.org/10.1007/s11657-013-0137-0
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M et al (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16(1):82. https://doi.org/10.1007/s11657-020-00871-9
Engelke K, Lang T, Khosla S, Qin L, Zysset P, Leslie WD et al (2015) Clinical use of quantitative computed tomography-based advanced techniques in the management of osteoporosis in adults: the 2015 ISCD official positions-part III. J Clin Densitom 18(3):393–407. https://doi.org/10.1016/j.jocd.2015.06.010
Therkildsen J, Nissen L, Jørgensen HS, Thygesen J, Ivarsen P, Frost L et al (2020) Thoracic bone mineral density derived from cardiac CT is associated with greater fracture rate. Radiology 296(3):499–508. https://doi.org/10.1148/radiol.2020192706
Therkildsen J, Winther S, Nissen L, Jorgensen HS, Thygesen J, Ivarsen P et al (2020) Feasibility of opportunistic screening for low thoracic bone mineral density in patients referred for routine cardiac CT. J Clin Densitom 23(1):117–127. https://doi.org/10.1016/j.jocd.2018.12.002
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359(9321):1929–1936. https://doi.org/10.1016/s0140-6736(02)08761-5
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43. https://doi.org/10.1007/s11657-017-0324-5
Kanis JA, Harvey NC, Johansson H, Oden A, Leslie WD, McCloskey EV (2017) FRAX Update. J Clin Densitom 20(3):360–367. https://doi.org/10.1016/j.jocd.2017.06.022
Shepstone L, Lenaghan E, Cooper C, Clarke S, Fong-Soe-Khioe R, Fordham R et al (2018) Screening in the community to reduce fractures in older women (SCOOP): a randomised controlled trial. Lancet 391(10122):741–747. https://doi.org/10.1016/S0140-6736(17)32640-5
Sandhu SK, Nguyen ND, Center JR, Pocock NA, Eisman JA, Nguyen TV (2010) Prognosis of fracture: evaluation of predictive accuracy of the FRAX algorithm and Garvan nomogram. Osteoporos Int: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 21(5):863–871. https://doi.org/10.1007/s00198-009-1026-7
Peacock M, Turner CH, Econs MJ, Foroud T (2002) Genetics of osteoporosis. Endocr Rev 23(3):303–326. https://doi.org/10.1210/edrv.23.3.0464
Yang TL, Shen H, Liu A, Dong SS, Zhang L, Deng FY et al (2020) A road map for understanding molecular and genetic determinants of osteoporosis. Nat Rev Endocrinol 16(2):91–103. https://doi.org/10.1038/s41574-019-0282-7
Kanis JA, Johansson H, Oden A, Johnell O, De Laet C, Eisman JA et al (2004) A family history of fracture and fracture risk: a meta-analysis. Bone 35(5):1029–1037. https://doi.org/10.1016/j.bone.2004.06.017
Estrada K, Styrkarsdottir U, Evangelou E, Hsu YH, Duncan EL, Ntzani EE et al (2012) Genome-wide meta-analysis identifies 56 bone mineral density loci and reveals 14 loci associated with risk of fracture. Nat Genet 44(5):491–501. https://doi.org/10.1038/ng.2249
Forgetta V, Keller-Baruch J, Forest M, Durand A, Bhatnagar S, Kemp JP et al (2020) Development of a polygenic risk score to improve screening for fracture risk: a genetic risk prediction study. PLoS Med 17(7):e1003152. https://doi.org/10.1371/journal.pmed.1003152
Lu T, Forgetta V, Keller-Baruch J, Nethander M, Bennett D, Forest M et al (2021) Improved prediction of fracture risk leveraging a genome-wide polygenic risk score. Genome Med 13(1):16. https://doi.org/10.1186/s13073-021-00838-6
Medina-Gomez C, Kemp JP, Trajanoska K, Luan J, Chesi A, Ahluwalia TS et al (2018) Life-course genome-wide association study meta-analysis of total body BMD and assessment of age-specific effects. Am J Hum Genet 102(1):88–102. https://doi.org/10.1016/j.ajhg.2017.12.005
Choi SW, Mak TS, O'Reilly PF (2020) Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc 15(9):2759–2772. https://doi.org/10.1038/s41596-020-0353-1
Nissen L, Winther S, Isaksen C, Ejlersen JA, Brix L, Urbonaviciene G et al (2016) Danish study of non-invasive testing in coronary artery disease (Dan-NICAD): study protocol for a randomised controlled trial. Trials 17(1):262. https://doi.org/10.1186/s13063-016-1388-z
Budoff MJ, Khairallah W, Li D, Gao YL, Ismaeel H, Flores F et al (2012) Trabecular bone mineral density measurement using thoracic and lumbar quantitative computed tomography. Acad Radiol 19(2):179–183. https://doi.org/10.1016/j.acra.2011.10.006
The guideline “Practice parameter for the performance of musculoskeletal quantitative computed tomography (QCT)" is available at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/QCT.pdf. Revised in 2018. Accessed 18 August 2022.
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 25(10):2359–2381
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/clep.s91125
Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ (2015) Second-generation PLINK: rising to the challenge of larger and richer datasets. GigaScie 4:7. https://doi.org/10.1186/s13742-015-0047-8
Das S, Forer L, Schönherr S, Sidore C, Locke AE, Kwong A et al (2016) Next-generation genotype imputation service and methods. Nat Genet 48(10):1284–1287. https://doi.org/10.1038/ng.3656
Rohde PD, Fourie Sørensen I, Sørensen P (2020) qgg: an R package for large-scale quantitative genetic analyses. Bioinformatics (Oxford, England) 36(8):2614–2615. https://doi.org/10.1093/bioinformatics/btz955
Rohde PD, Sørensen IF, Sørensen P (2022) Expanded utility of the R package qgg with applications within genomic medicine. bioRxiv:2022–2009. https://doi.org/10.1101/2022.09.03.506466
Christiansen MK, Winther S, Nissen L, Vilhjálmsson BJ, Frost L, Johansen JK et al (2021) Polygenic risk score-enhanced risk stratification of coronary artery disease in patients with stable chest pain. Circ Genom Precis Med 14(3):e003298. https://doi.org/10.1161/circgen.120.003298
Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27(2):157–172. https://doi.org/10.1002/sim.2929
Cook NR, Paynter NP (2011) Performance of reclassification statistics in comparing risk prediction models. Biom J Biometrische Zeitschrift 53(2):237–258. https://doi.org/10.1002/bimj.201000078
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 18(8):1033–1046. https://doi.org/10.1007/s00198-007-0343-y
Cook NR (2018) Quantifying the added value of new biomarkers: how and how not. Diagn Progn Res 2:14. https://doi.org/10.1186/s41512-018-0037-2
Lo A, Chernoff H, Zheng T, Lo SH (2015) Why significant variables aren't automatically good predictors. Proc Natl Acad Sci USA 112(45):13892–13897. https://doi.org/10.1073/pnas.1518285112
Anam AK, Insogna K (2021) Update on osteoporosis screening and management. Med Clin North Am 105(6):1117–1134. https://doi.org/10.1016/j.mcna.2021.05.016
Ma Y, Zhou X (2021) Genetic prediction of complex traits with polygenic scores: a statistical review. Trends Genet 37(11):995–1011. https://doi.org/10.1016/j.tig.2021.06.004
Richards JB, Zheng HF, Spector TD (2012) Genetics of osteoporosis from genome-wide association studies: advances and challenges. Nat Rev Genet 13(8):576–588. https://doi.org/10.1038/nrg3228
Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE et al (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164(10):1108–1112. https://doi.org/10.1001/archinte.164.10.1108
Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS et al (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res: the official journal of the American Society for Bone and Mineral Research. 18(11):1947–1954. https://doi.org/10.1359/jbmr.2003.18.11.1947
Herath M, Cohen A, Ebeling PR, Milat F (2022) Dilemmas in the management of osteoporosis in younger adults. JBMR Plus 6(1):e10594. https://doi.org/10.1002/jbm4.10594
Ho-Le TP, Center JR, Eisman JA, Nguyen HT, Nguyen TV (2017) Prediction of bone mineral density and fragility fracture by genetic profiling. journal of bone and mineral research : the official journal of the American Society for Bone and Mineral. Research 32(2):285–293. https://doi.org/10.1002/jbmr.2998
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N et al (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 22(9):2395–2411. https://doi.org/10.1007/s00198-011-1713-z
Tosteson AN, Burge RT, Marshall DA, Lindsay R (2008) Therapies for treatment of osteoporosis in US women: cost-effectiveness and budget impact considerations. Am J Manag Care 14(9):605–615
Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML et al (2008) Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom: the official journal of the International Society for Clinical Densitometry. 11(1):123–162. https://doi.org/10.1016/j.jocd.2007.12.010
Budoff MJ, Hamirani YS, Gao YL, Ismaeel H, Flores FR, Child J et al (2010) Measurement of thoracic bone mineral density with quantitative CT. Radiology 257(2):434–440. https://doi.org/10.1148/radiol.10100132
LeDell E, Petersen M, van der Laan M (2015) Computationally efficient confidence intervals for cross-validated area under the ROC curve estimates. Electron J Stat 9(1):1583–1607. https://doi.org/10.1214/15-ejs1035
Acknowledgements
The authors are grateful for all the priceless and valuable work done by the clinical staff involved in the Dan-NICAD trial. Furthermore, this research project would not have been possible without the financial support from the listed contributors, and finally, the authors would like to thank all study participants for their contribution.
Funding
Open access funding provided by Aarhus University Hospital. The Danish Heart Foundation (15-R99-A5837-22920), the Hede Nielsen Foundation, the Danish Council for Independent Research (DFF–7025–00103), the Health Research Fund of Central Denmark Region, the Danish Osteoporosis Foundation, and Acarix A/S (unrestricted grant) funded this research project. SW acknowledges support from the Novo Nordisk Foundation Clinical Emerging Investigator grant (NNF21OC0066981). The funding sources did not take any part in the design of this sub-study; in the collection, analysis, and interpretation of the data; in writing the report; or in the decision to submit this article to publication.
Author information
Authors and Affiliations
Contributions
Josephine Therkildsen: conceptualization and design, data acquisition, funding acquisition, data analysis and interpretation, writing original draft, review, and editing. Palle Duun Rohde: conceptualization and design, data acquisition, data analysis and interpretation, review, and editing. Louise Nissen: conceptualization and design, data acquisition, funding acquisition, data analysis and interpretation, review, and editing. Jesper Thygesen: data acquisition, data analysis and interpretation, review, and editing. Ellen-Margrethe Hauge: data analysis and interpretation, review, and editing. Bente L. Langdahl: data analysis and interpretation, review, and editing. Morten Boettcher: conceptualization and design, data acquisition, funding acquisition, data analysis and interpretation, review, and editing. Mette Nyegaard: conceptualization and design, data acquisition, data analysis and interpretation, review, and editing. Simon Winther: conceptualization and design, data acquisition, funding acquisition, data analysis and interpretation, review, and editing. All authors made substantial contributions to the conception and design, acquisition of the data, or analysis and interpretation of the data. All authors participated in drafting the manuscript and revised it critically. All authors approved the final version and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Statement of human rights
All individual participants gave written, informed consent before enrolment in the study. The Central Denmark Regional Committee on Health Research Ethics (date: 2014-07-30, ref.: 1-10-72-190-14) and the Danish Data Protection Agency (ref.: 1-16-02-345-14) approved this study. The trial was registered at ClinicalTrials.gov (NCT02264717). All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
Ellen-Margrethe Hauge has received honorariums and/or consulting fees from AbbVie, Sanofi, Sobi, and SynACT Pharma and research grants to Aarhus University Hospital from Danish Regions Medicine Grants, Danish Rheumatism Association, Roche, Novartis, and Novo Nordic Foundation. Bente L. Langdahl has received honorariums from Amgen, UCB, Gedeon-Richter, Astra-Zenica, and Astellas and worked as a consultant for Amgen, UCB, Gedeon-Richter, and Gilead. Furthermore, Bente L. Langdahl has received financial grants from Amgen and the Novo Nordic Foundation. Morten Boettcher disclosed advisory board participation for NOVO Nordisk, Astra-Zeneca, Pfizer, Boeringer Ingelheim, Bayer, Sanofi, Novartis, and Acarix. Josephine Therkildsen, Palle Duun Rohde, Louise Nissen, Jesper Thygesen, Mette Nyegaard, and Simon Winther declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Therkildsen, J., Rohde, P., Nissen, L. et al. A genome-wide genomic score added to standard recommended stratification tools does not improve the identification of patients with very low bone mineral density. Osteoporos Int 34, 1893–1906 (2023). https://doi.org/10.1007/s00198-023-06857-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06857-w