Abstract
Summary
We studied the characteristics of patients prescribed osteoporosis medication and patterns of use in European databases. Patients were mostly female, older, had hypertension. There was suboptimal persistence particularly for oral medications. Our findings would be useful to healthcare providers to focus their resources on improving persistence to specific osteoporosis treatments.
Purpose
To characterise the patients prescribed osteoporosis therapy and describe the drug utilization patterns.
Methods
We investigated the treatment patterns of bisphosphonates, denosumab, teriparatide, and selective estrogen receptor modulators (SERMs) in seven European databases in the United Kingdom, Italy, the Netherlands, Denmark, Spain, and Germany. In this cohort study, we included adults aged ≥ 18 years, with ≥ 1 year of registration in the respective databases, who were new users of the osteoporosis medications. The study period was between 01 January 2018 to 31 January 2022.
Results
Overall, patients were most commonly initiated on alendronate. Persistence decreased over time across all medications and databases, ranging from 52–73% at 6 months to 29–53% at 12 months for alendronate. For other oral bisphosphonates, the proportion of persistent users was 50–66% at 6 months and decreased to 30–44% at 12 months. For SERMs, the proportion of persistent users at 6 months was 40–73% and decreased to 25–59% at 12 months. For parenteral treatment groups, the proportions of persistence with denosumab were 50–85% (6 month), 30–63% (12 month) and with teriparatide 40–75% (6 month) decreasing to 21–54% (12 month). Switching occurred most frequently in the alendronate group (2.8–5.8%) and in the teriparatide group (7.1–14%). Switching typically occurred in the first 6 months and decreased over time. Patients in the alendronate group most often switched to other oral or intravenous bisphosphonates and denosumab.
Conclusion
Our results show suboptimal persistence to medications that varied across different databases and treatment switching was relatively rare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis medications, including bisphosphonates, denosumab, teriparatide, and selective estrogen receptor modulators (SERM) have well-established efficacy in reducing fracture risk [1, 2]. Clinical guidelines from the United Kingdom (UK) [3] and the European Union (EU) [1] recommend bisphosphonates as first-line therapy for primary and secondary prevention of fragility fractures. SERMs are indicated for treatment and prevention of osteoporosis in postmenopausal women. In patients with higher risk of fractures, denosumab or teriparatide may be initiated. Sequential therapy includes starting an anabolic agent and switching over to an anti-resorptive to potentiate skeletal benefit. Non-persistence is associated with 40% greater fracture risk [4]. Persistence to osteoporosis therapy can be measured using real world data which includes electronic healthcare records, claims data, and prescription databases. The use of these data sources reflects clinical practice and may be more reliable than self-reported persistence rates, which tend to be higher than pharmacy dispensation data [5]. Systematic reviews of persistence to osteoporosis medications using real world data showed declining rates at 1 year and 2 years after starting therapy [5, 6]. In the literature, studies were mostly limited to specific types of osteoporosis medications in a single population. Two recent systematic reviews only focused on oral bisphosphonates [6] and parenteral therapies [5] respectively and have limitations due to methodological heterogeneity used by the included studies, making it difficult to compare trends across different countries. Thus, the objective of our study was to describe the characteristics of patients initiated on various osteoporosis therapy, as well as the drug utilization patterns after starting treatment using standardised methodology across the adult population in six European countries.
Methods
Study design
This was a multi-national, multi-database cohort study conducted in 6 European countries. The study protocol (EUPAS35956) was registered on the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) [7].
The following data sources comprising primary care, secondary care, health registers, prescription/dispensation registers and claims were utilized.
-
1.
Clinical Practice Research Datalink (CPRD) GOLD [8] and AURUM [9] from the UK.
- 2.
-
3.
Integrated Primary Care Information Project (IPCI) 12 from the Netherlands.
-
4.
Data linked from the population-based administrative and health registries in Denmark (NDR) [13,14,15,16].
-
5.
Sistema d'Informació per al Desenvolupament de la Investigació en Atenció Primària (SIDIAP) [17] from Spain.
-
6.
German Pharmacoepidemiological Research Database (GePaRD) [18] from Germany.
The observation period for all databases started on 01 January 2018 and ended on 31 December 2019 for GePaRD; 31 December 2020 for NDR; 31 December 2021 for HSD, IPCI, and SIDIAP; and 31 January 2022 for CPRD GOLD and AURUM. The databases were accessed in a federated network. Standardized input files containing harmonised codes for drug exposure and comorbidities were processed via the Jerboa © software [19] for CPRD, HSD, IPCI, and SIDIAP; and using verified SAS 9.4 analytical codes for NDR and GePaRD, where only aggregated results were permitted to be shared. The output of de-identified results was deposited in a remote research environment with secure and restricted access provided to data partners and analysts.
We included patients aged 18 years or older, who had at least one year of data available in one of the contributing databases and were new users of one of the six osteoporosis treatment groups with the corresponding ATC codes: (i) alendronate [M05BA04], (ii) other oral bisphosphonates (ibandronate [M05BA06] or risedronate [M05BA07]), (iii) intravenous bisphosphonates (zoledronate [M05BA08]), (iv) SERM (raloxifene [G03XC01], bazedoxifene [G03XC02], and lasofoxifene [G03XC03]), (v) denosumab [M05BX04], (vi) teriparatide [H05AA02]. New users were defined as patients who did not have a prescription of an osteoporosis treatment from the same treatment group in the year prior to the start of osteoporosis therapy. The date of the first prescription for a given drug was used as the index date. The end of drug exposure was defined as the date of the last prescription or dispensation or claim for the study drug plus the calculated number of exposure days provided in the last prescription or dispensation based on the dispensed strength, package size and defined daily dose (DDD). For parenteral treatments, durations were defined according to the indicated dosing intervals: zoledronate (365 days), denosumab (182 days), teriparatide (quantity of 28-dose pen multiplied by 28 days). To define treatment episodes of continuous use of osteoporosis drugs, any two prescriptions of the same treatment cohort were concatenated. Treatment gaps of ≤ 90 days [20, 21] between drug utilization records for the study drug were allowed and stockpiling was dismissed. A refill gap exceeding 90 days was considered therapy discontinuation. Drug discontinuation was therefore defined as the last date of exposure to a study drug plus an additional 90 days (in line with the treatment gap). After study drug discontinuation, a patient could initiate another osteoporosis medication. All analyses were conducted at the treatment episode level. The same patient was therefore eligible to contribute to different drug cohorts if they switched treatments during the study period. Treatment switching was defined as initiation of another medication from a different osteoporosis treatment group as aforementioned. At the time of switching, patient was considered to have discontinued the first medication if the treatment gap was less than 90 days. For each medication, patients were followed from the index date until the earliest of the following dates: discontinuation of current treatment, switching to another osteoporosis medication, death, end of enrolment in database, or end of data collection.
Statistical analysis
We described the baseline characteristics, comorbidities, and medication history of the patients in each database. These variables were defined using diagnosis codes (Appendix 1), medication codes (Appendix 2), and measurement data (Appendix 3). The lookback period for comorbidities was any time prior to index date to account for chronic conditions, and one year prior to index date for medication history to indicate recency of use. Descriptive statistics were reported for treatment duration. The proportion of persistent users and the proportion of patients who switched medication were assessed for each treatment group and database at 6 months, 12 months, 18 months, and 24 months. Persistence was defined as the continuation of treatment with ≤ 90 days gap between prescriptions. Sankey diagrams were plotted to illustrate treatment patterns over time. Counts < 5 were supressed in line with database specific guidelines. Data analysis was performed using R version 4.0.3.
Results
Patient characteristics
We included the following number of patients from each database (CPRD GOLD: 7,665; CPRD AURUM: 175,557; HSD: 24,155; IPCI: 18,218; NDR: 95,601; SIDIAP: 72,457; GePaRD: 89,344) (Table 1). The median age (interquartile range [IQR]) of new users at initiation of osteoporosis therapy was similar across CPRD GOLD and AURUM (75 [66 – 82] years), HSD (72 [63–79] years), IPCI (72 [64–80] years), NDR (71 [63–78]), SIDIAP (72 [64–81] years), and GePaRD (75 [66–80] years). Most participants were females across all data sources (CPRD GOLD 80%, CPRD AURUM 79%, HSD 91%, IPCI 76%, NDR 78%, SIDIAP 88%, GePaRD 88%).
The most prevalent comorbidities were hypertension (CPRD GOLD 54%, CPRD AURUM 56%, HSD 54%, IPCI 45%, NDR 27%, SIDIAP 51%, GePaRD 67%), hypercholesterolemia (CPRD GOLD 34%, CPRD AURUM 36%, HSD 37%, IPCI 22%, NDR 31%, SIDIAP 40%, GePaRD 59%), and cancer (CPRD GOLD 23%, CPRD AURUM 25%, HSD 22%, IPCI 22%, NDR 32%, SIDIAP 44%, GePaRD 24%).
Prevalence of cardiovascular disease (angina, atherosclerosis, atrial fibrillation) were 37% (CPRD GOLD), 39% (CPRD AURUM), 29% (HSD), 37% (IPCI), 27% (NDR), 28% (SIDIAP) and 51% (GePaRD); of myocardial infarction (CPRD GOLD 6.8%, CPRD AURUM 7.1%, HSD 1.5%, IPCI 5.8%, NDR 3.9%, SIDIAP 2.6%, GePaRD 5.7%) and prior stroke (CPRD GOLD 6.8%, CPRD AURUM 7.2%, HSD 6.8%, IPCI 6.9%, NDR 7.5%, SIDIAP 5.4%, GePaRD 8.4%).
A total of 45-86% of patients had a formal diagnosis of osteoporosis at the time of therapy initiation (CPRD GOLD 46%, CPRD AURUM 50%, HSD 65%, IPCI 49%, NDR 45%, SIDIAP 64%, GePaRD 86%). A total of 32-54% of patients (CPRD GOLD 48%, CPRD AURUM 54%, HSD 36%, IPCI 40%, NDR 41%, SIDIAP 47%, GePaRD 32%) had a previous history of fracture.
The most prevalent medications were proton pump inhibitors (CPRD 49%, HSD 46%, IPCI 53%, NDR 35%, SIDIAP 27%, GePaRD 48%), antihypertensives (excluding beta blockers, ACE/angiotensin inhibitors) (CPRD GOLD 38%, CPRD AURUM 40%, HSD 26%, IPCI 32%, NDR 38%, SIDIAP 19%, GePaRD 35%), and lipid lowering agents (CPRD GOLD 39%, CPRD AURUM 40%, HSD 29%, IPCI 31%, NDR 31%, SIDIAP 14%, GePaRD 27%). Key co-medications and co-morbidities in the overall population for each database are presented in Table 1.
Treatment duration
Overall, alendronate was the most common osteoporosis treatment in all databases (Table 2). This was followed by other oral bisphosphonates (CPRD GOLD, CPRD AURUM, HSD, and IPCI), denosumab (SIDIAP and GePaRD), or intravenous bisphosphonates (NDR). Across all data sources, the type of osteoporosis treatment with the longest median duration of treatment was intravenous bisphosphonates in most databases – CPRD GOLD: 400 (interquartile range [IQR] [287 – 443]) days; CPRD AURUM: 455 [250 – 455]; HSD: 455 [227 – 455]; IPCI: 455 [294 – 671]; NDR: 455 [298 – 703]; GePaRD: 342 [168 – 455] (Table 3). There were no users of intravenous bisphosphonates in SIDIAP where the longest median duration of treatment was 407 [182 – 750] days in alendronate users. Duration of alendronate use was highest in SIDIAP and lowest in GePaRD (174 [118 – 322]).
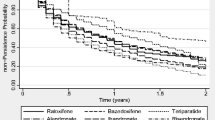
Treatment persistence
Across all data sources and treatment groups, the proportion of patients persistent to treatment decreased over time. For alendronate, persistence at 6 months ranged across databases between 44–75% and decreased to 21–55% at 12 months, 9–35% at 18 months, 0–26% at 24 months. For other oral bisphosphonates, persistence at 6 months was 46–69% and decreased to 22–46% at 12 months, 9–27% at 18 months, 0–19% at 24 months. For SERMs, persistence at 6 months was 44–78% and decreased to 22–54% at 12 months, 9–37% at 18 months, at 0–30% at 24 months. For parenteral treatment groups, the proportions of persistent users for zoledronic acid were: 73–84% (6 month), 47–68% (12 month), 4–39% (18 month), 0–23% (24 month); for denosumab: 72–87% (6 month), 37–52% (12 month), 16–34% (18 month), 0–23% (24 month); for teriparatide: 5–75% (6 month), 3–54% (12 month), 1–36% (18 month), 0–20% (24 month). To note, actual duration of treatment might have exceeded the end date of data extraction. The treatment persistence over time for each drug group and database is presented in Table 4.
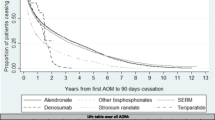
Treatment switching
Overall, switching occurred most frequently in the alendronate group (2.8 – 5.8%) in CPRD GOLD and IPCI; in the teriparatide group (7.1–14%) across HSD, NDR, and SIDIAP, and GePaRD; and in the SERM group (4.9%) in CPRD AURUM. Switching occurred most frequently in the first 6 months and decreased over time (Table 5). The Sankey diagrams of switching patterns are presented in Fig. 1. Patients in alendronate group most often switched to other oral bisphosphonates in CPRD GOLD, CPRD AURUM, HSD, IPCI; to denosumab in SIDIAP; to denosumab and IV bisphosphonates in NDR, and to denosumab and other oral bisphosphonates in GePaRD.
A Sankey diagram of treatment switching pattern (CPRD GOLD). B Sankey diagram of treatment switching pattern (CPRD AURUM). C Sankey diagram of treatment switching pattern (HSD). D Sankey diagram of treatment switching pattern (IPCI). E Sankey diagram of treatment switching pattern (NDR). F Sankey diagram of treatment switching pattern (SIDIAP). G Sankey diagram of treatment switching pattern (GePaRD). ALN: alendronate; DENO: denosumab; IVBP: intravenous bisphosphonates; OBP: other oral bisphosphonates; SERM: selective estrogen receptor modulators; TERI: teriparatide. The colour coded paths depict the proportion of users continuing/switching treatment at time points 6 months, 12 months, 18 months, and 24 months. The red paths depict the proportion of users who discontinued treatment (STOP). The grey paths depict the proportion of users censored (CEN) (end of follow-up) before the respective time points
Discussion
The trends observed in our drug utilization study are in line with previous studies and with current European guidelines and treatment algorithms [22], with a predominance of older women amongst patients receiving osteoporosis treatment. The baseline characteristics of the participants indicated a high proportion of women in their 70s, and a high prevalence of osteoporosis and/or previous fracture. Cardiovascular history and risk factors for cardiovascular disease such as hypertension and hypercholesterolemia were common in this population, probably due to ageing and the known association between osteoporosis and cardiovascular disease [23].
The treatment persistence to oral bisphosphonates was similar to that reported in a systematic review, which ranged from 35–71% at 6 months, 18–75% at 1 year and 13–72% at 2 years [6]. Persistence to SERMs in our study was similar to that by Li et al. [24], which found persistence to raloxifene was 45% at 6 months and 33% at 1 year in the General Practitioner Research Database. Persistence to parenteral osteoporosis therapy in our study was lower than that reported in a systematic review, which ranged from 34–73% for zoledronic acid, 61–100% for denosumab, 10–87% for teriparatide at 1 year respectively [5]. The observed persistence with osteoporosis treatments was well below the recommended treatment duration of at least 18 months with teriparatide [1] and three to five years with all other treatments [1, 25]. Unfortunately, this is a known issue in the field, which hampers the effort to treat patients at high risk of fracture due to suboptimal compliance [26]. Conversely, prescription of teriparatide beyond 24 months shows possible off-label usage as teriparatide is clinically limited to 24 months [25]. In primary care in Italy, teriparatide cannot be prescribed by general practitioners, but only by specialists. It is possible that the off-label use is the result of a lag in the registration of prescriptions by the general practitioner into the electronic health record.
Treatment switching patterns varied across the databases. Switching from oral bisphosphonates are most likely motivated by gastric intolerance or perceived lack of efficacy [27]. In contrast, switching from teriparatide is most likely related to planned sequential therapy, which has been shown to provide further benefits when a bone forming agent (teriparatide) is immediately followed by an anti-resorptive (a bisphosphonate or denosumab) [1]. In a study where general practitioners recruited postmenopausal women across 5 European countries [28], the percentage of switching among new users was 9%, which was comparable to the range observed in our study (3 to 14%).
The strength of our study is that we performed a multinational database analysis of prescription and dispensation records and included a variety of osteoporosis medications using standardized methodology, which allowed us to compare the recent trends of treatment patterns and pathways in different countries. Our study is the largest to date on the characteristics and treatment patterns of patients on osteoporosis therapy, with more than 450,000 patients from seven data sources in six European countries. Our results provide a timely update to the literature, as the latest time frame of data collection in recent systematic reviews were until 2011 for oral bisphosphonates [6] and 2016 for parenteral treatments [5] respectively in European studies. Moreover, we provided information about treatment duration and switching patterns in addition to treatment persistence. Our findings would be useful to healthcare providers to focus their resources on improving persistence to specific osteoporosis treatments with suboptimal compliance.
Our study has limitations. Firstly, misclassification of persistence to the osteoporosis medications is possible. This is particularly relevant to primary care databases such as IPCI, HSD, and CPRD, since they are not necessarily equivalent to the actual consumption or use of the prescribed therapies. However, sensitivity analyses in a previous study [29] conducted in Spain suggested little impact of such misclassification in these data. This study was based on index exposure and dismissing compliance and showed similar findings to those seen in the ‘on treatment’ analyses. Second, no bisphosphonates in fixed combination with calcium/vitamin D were included for the definition of exposure drug classes. While potentially some prescriptions including drugs defining exposure could have been missed, these preparations are typically prescribed rarely compared to plain bisphosphonate preparations. Third, no distinction could be made between ibandronate as oral versus parenteral use because there is no difference in the ATC code, hence the intravenous bisphosphonate group did not include the ATC code for ibandronate in this study. Fourth, due to the nature of the databases (CPRD, HSD, IPCI, SIDIAP), the use of intravenous bisphosphonates, which is more commonly prescribed in secondary care settings, may be underreported. However, these dispensations would be captured in GePaRD and NDR. Lastly, the observational nature of this study makes it vulnerable to confounding by indication due to differential use of medicines according to baseline fracture risk. For example, in all databases, diagnosis of osteoporosis and history of fracture was higher in denosumab versus alendronate users. Such differences in perceived or estimated risk can lead to differences in persistence not attributable to the drug itself but to imbalances in patient characteristics. Patients with higher fracture risk may be more likely to persist with osteoporosis therapy, but the difference in persistence at 12 months between denosumab and alendronate of more than 5% was only observed in some databases (HSD, IPCI, GePaRD) and not others (CPRD GOLD, CPRD AURUM, NDR, SIDIAP).
In conclusion, we have described the duration, persistence and switching of patients who initiated osteoporosis medications in six European countries. Switching was found to be relatively rare and could be for planned sequential therapy as recommended by healthcare professionals. Persistence was generally low and varied between databases. While treatment use varied by country, alendronate was the most common osteoporosis treatment across all databases.
Data availability
Direct data sharing is not allowed by European law. The data are not publicly available due to privacy or ethical restrictions. Data holders included as co-authors can be contacted to learn more on data access conditions.
References
Kanis JA, Cooper C, Rizzoli R, Reginster JY (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30(1):3–44
Crandall CJ, Newberry SJ, Diamant A, Lim YW, Gellad WF, Booth MJ et al (2014) Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med 161(10):711–723
Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, Gittoes NJL et al (2022) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 17(1):58
Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E, Siris E (2011) A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health 14(4):571–581
Koller G, Goetz V, Vandermeer B, Homik J, McAlister FA, Kendler D et al (2020) Persistence and adherence to parenteral osteoporosis therapies: a systematic review. Osteoporos Int 31(11):2093–2102
Fatoye F, Smith P, Gebrye T, Yeowell G (2019) Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open 9(4):e027049
The European Union electronic Register of Post-Authorisation Studies. European Non-interventional Post-authorization Safety Study Related to Adherence to the Risk Minimization Measures for Romosozumab by the EU-ADR Alliance (EUPAS35956) Registered 25 June 2020 [updated 29 Oct 2020. Available from: http://www.encepp.eu/encepp/viewResource.htm?id=37813, Accessed 11 Jan 2023
Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T et al (2015) Data Resource Profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 44(3):827–836
Wolf A, Dedman D, Campbell J, Booth H, Lunn D, Chapman J et al (2019) Data resource profile: Clinical Practice Research Datalink (CPRD) Aurum. Int J Epidemiol. 48(6):1740-g
Cazzola M, Puxeddu E, Bettoncelli G, Novelli L, Segreti A, Cricelli C et al (2011) The prevalence of asthma and COPD in Italy: a practice-based study. Respir Med 105(3):386–391
Filippi A, Vanuzzo D, Bignamini A, Mazzaglia G, Cricelli C, Catapano A (2005) The database of Italian general practitioners allows a reliable determination of the prevalence of myocardial infarction. Ital Heart J 6(4):311–314
de Ridder MAJ, de Wilde M, de Ben C, Leyba AR, Mosseveld BMT, Verhamme KMC et al (2022) Data Resource Profile: The Integrated Primary Care Information (IPCI) database. The Netherlands. Int J Epidemiol 51(6):e314–e323
Pottegard A, Schmidt SAJ, Wallach-Kildemoes H, Sorensen HT, Hallas J, Schmidt M (2017) Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol. 46(3):798-f
Schmidt M, Pedersen L, Sorensen HT (2014) The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 29(8):541–549
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490
Schmidt M, Schmidt SAJ, Adelborg K, Sundboll J, Laugesen K, Ehrenstein V et al (2019) The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol 11:563–591
Recalde M, Rodríguez C, Burn E, Far M, García D, Carrere-Molina J et al (2022) Data Resource Profile: The Information System for Research in Primary Care (SIDIAP). Int J Epidemiol 51(6):e324–e336
Haug U, Schink T (2021) German Pharmacoepidemiological Research Database (GePaRD). In: Sturkenboom M, Schink T (eds) Databases for Pharmacoepidemiological Research. Springer International Publishing, Cham, pp 119–124
Lovestone S (2020) The European medical information framework: A novel ecosystem for sharing healthcare data across Europe. Learn Health Syst 4(2):e10214
Gallagher AM, Rietbrock S, Olson M, van Staa TP (2008) Fracture Outcomes Related to Persistence and Compliance With Oral Bisphosphonates. J Bone Miner Res 23(10):1569–1575
Yun H, Curtis JR, Guo L, Kilgore M, Muntner P, Saag K et al (2014) Patterns and predictors of osteoporosis medication discontinuation and switching among Medicare beneficiaries. BMC Musculoskelet Disord 15(1):112
Kanis JA, Harvey NC, McCloskey E, Bruyère O, Veronese N, Lorentzon M et al (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31(1):1–12
Lello S, Capozzi A, Scambia G (2015) Osteoporosis and cardiovascular disease: an update. Gynecol Endocrinol 31(8):590–594
Li L, Roddam A, Gitlin M, Taylor A, Shepherd S, Shearer A et al (2012) Persistence with osteoporosis medications among postmenopausal women in the UK General Practice Research Database. Menopause 19(1):33–40
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43
Reyes C, Tebe C, Martinez-Laguna D, Ali MS, Soria-Castro A, Carbonell C et al (2017) One and two-year persistence with different anti-osteoporosis medications: a retrospective cohort study. Osteoporos Int 28(10):2997–3004
Paskins Z, Crawford-Manning F, Cottrell E, Corp N, Wright J, Jinks C et al (2020) Acceptability of bisphosphonates among patients, clinicians and managers: a systematic review and framework synthesis. BMJ Open 10(11):e040634
Roux C, Martinez L, Horne R, Diez-Perez A, Guillemin F, Ortolani S et al (2011) Switching patterns over 12months in European postmenopausal women initiating or receiving bone loss medications: The POSSIBLE EU® Study. Bone 48:S215
Prieto-Alhambra D, Elorza-Ricart JM, Hermosilla E, Rodriguez-Ruiz J, Mendez-Boo LMMP (2014) Primary Care Prescriptions and Subsequent Pharmacy Dispensing: A Population-Based Study. Pharmacoepidemiol Drug Safe 23:322
Acknowledgements
This study was funded by UCB Biopharma SRL and Amgen Inc in the context of a post-authorization safety study (PASS) requested by the European Medicines Agency. The study was performed in line with the ENCePP Code of Conduct. The authors had complete autonomy in the process of establishing the protocol, carrying out the analyses, and interpreting the results and retained the full right to publish the results without limitation.
The BIPS team would like to thank all statutory health insurance providers which provided data for this study, namely AOK Bremen/Bremerhaven, DAK-Gesundheit, Die Techniker (TK), and hkk Krankenkasse.
We thank Fabio Riefolo and Natasha Yefimenko from Teamit Institute for the provided PASS scientific study management expertise.
This study is based in part on data from the Clinical Practice Research Datalink obtained under license from the UK Medicines and Healthcare products Regulatory Agency. The data is provided by patients and collected by the NHS as part of their care and support. The interpretation and conclusions contained in this study are those of the author/s alone.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AM is employed by UCB Biopharma SRL. AV, JR, and MB are working at an independent, non-profit research institute, the Leibniz Institute for Prevention Research and Epidemiology – BIPS. EM and FP provided consultancies in protocol preparation for epidemiological studies and data analyses for Amgen. PBL and RL are working at an independent, non-profit research institute, the Bordeaux PharmacoEpi platform (BPE) at Bordeaux University. KV, MM, Marcel de Wilde (MW) report receiving institutional funding support from the European Medicines Agency and Innovative Medicines Initiative. KV, MM, MW have received institutional grants from Johnson and Johnson, UCB, Chiesi, GSK, and Amgen outside this work. DPA’s department has received grant/s from Amgen, Chiesi-Taylor, Lilly, Janssen, Novartis, and UCB Biopharma. His research group has received consultancy fees from Astra Zeneca and UCB Biopharma. Amgen, Astellas, Janssen, Synapse Management Partners and UCB Biopharma have funded or supported training programmes organised by DPA's department. EHT, DR, AJ, MSS, KB, CR, LP, MFR, MA have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tan, E.H., Robinson, D.E., Jödicke, A.M. et al. Drug utilization analysis of osteoporosis medications in seven European electronic health databases. Osteoporos Int 34, 1771–1781 (2023). https://doi.org/10.1007/s00198-023-06837-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06837-0