Abstract
Summary
This articl e includes high-quality randomized controlled trials in recent years and updates the past meta-analysis. It has been proved that cast immobilization can achieve similar functional results, reduce economic burden in the long-term compared with surgery, and provide a basis for doctors to make treatment choices.
Purpose
The efficacy of conservative and surgical treatment of distal radius fractures (DRFs) in adults is still controversial. Recently, some high-quality randomized controlled trials (RCTs) evaluated the efficacy of both treatments. We hypothesized that treatment of DRFs with closed reduction and cast immobilization would achieve functional outcomes similar to surgery.
Methods
This study is a systematic review and summary of RCTs comparing conservative and surgical management of DRFs from 2005 to March 2022. Patients were evaluated for functional and imaging outcomes and complications.
Results
A total of 11 studies [1–11] included 1775 cases of DRFs. At 1-year follow-up, the cast group had lower mean differences (MDs) in DASH scores than the surgery group by − 2.55 (95% CI = − 5.02 to − 0.09, P = 0.04); with an MD of 1.63 (95% CI = 1.08–2.45, P = 0.02), while the surgery group had a lesser complication rate than the cast group.
Conclusions
At 1-year follow-up, the lower DASH scores of the cast group showed advantages of this treatment, but the complication rate was higher than that of the surgery group. There was no massive distinction in other scoring methods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among orthopedic diseases, distal radial fracture (DRF) is one of the most common fractures. According to the literature, the occurrence of DRFs may be multifactorial, and the age groups under 18 and over 65 have the highest proportion of DRFs (30.18 and 25.42/10,000, respectively) [1]. Foreign literature reports predict that by 2028, the number of DRFs in Australian adults over the age of 35 will grow at a rate of 20% per year, and by 2051, 60% increase of cases annually is expected [1, 2]. This phenomenon is due to the aging population. In recent years, the treatment of DRFs is mainly divided into surgical and conservative treatments. The surgical treatment of the distal radius mainly includes special materials, such as a locking plate, a Kirschner wire, and an external fixator. The conservative treatment is mainly closed reduction and cast immobilization [3]. Although the disease is very common and the treatment methods are ideal, the choice between conservative and surgical treatment has caused dilemma among clinicians.
There are some studies which support the view that surgical treatment is more effective than conservative treatment owing to the advantages, such as earlier function recovery and lower reoperation rate [4,5,6]. Although many studies support surgical treatment of DRFs, there are more studies that have reported the complication rate of DRF is still as high as 8–27% [7,8,9]. On the other hand, some studies have shown that the benefits of the cast fixation are similar to surgery. Postoperative consequences were not significantly different between conservative and surgical treatments; hence, cast application is more cost-effective. As a result, older adults who have more DRFs are more likely to choose conservative therapy [10]. In 2020, the American Academy of Orthopedic Surgeons and the American Society for Surgery of the Hand published new Clinical Practice Guidelines on assessing and treating acute DRFs. Strong evidence demonstrates that operational treatment for geriatric patients does not result in improved long-term patient-reported outcomes compared to nonoperative treatment [11]. A recent randomized controlled trial found that specific treatment options have insufficient evidence [12].
This is a meta-analysis based on the relevant contents published for many years. However, a previous meta-analysis was published many years ago and the study needs to be updated. Several randomized control trials (RCTs) tackling this problem have recently been published, with no fewer than three high-quality RCTs included, allowing for a powerful revision of the results.
In this meta-analysis, 11 RCTs [13,14,15,16,17,18,19,20,21,22,23] were included, which evaluated the efficacy of closed reduction and cast immobilization and surgery in treating adult DRFs. We assume that the cast group and surgery group can obtain similar prognostic effect, so as to provide a basis for clinicians to choose conservative treatment.
Methods
Literature search
The PRISMA guidelines [10], which is the ideal reporting item for systematic reviews and meta-analyses, was used to conduct this study. The two authors searched extensively for articles published in PubMed, the Cochrane Library, and EMBASE between 2005 and March 2022. The following retrieval strategy was used: (((((((Radius Fractures[MESH]) OR (Wrist Injuries[Title/Abstract])) OR (Wrist Injuries[MESH])) OR ((radius[Title/Abstract] OR radial[Title/Abstract] OR wrist[Title/Abstract] OR colles[Title/Abstract] OR smith*[Title/Abstract]) AND fracture*[Title/Abstract])) OR (distal near radial[Title/Abstract])) OR (distal near radial[MESH])) OR (fractur*[Title/Abstract])) AND ((((((orthopedic procedure[MESH]) OR (orthopedic procedure[Title/Abstract])) OR (orthopedics[MESH])) OR (orthopedics[Title/Abstract])) AND ((conservative treatment[MESH])) OR (Physical therapy modalities[MESH])) OR (conserv*[Title/Abstract] OR conven*[Title/Abstract] OR non-operat*[Title/Abstract] OR nonsurg*[Title/Abstract] OR cast*[Title/Abstract] OR splint*[Title/Abstract] OR brace*[Title/Abstract] OR Plaster*[Title/Abstract] OR bandage*[Title/Abstract] OR Tap*[Title/Abstract]))) AND ((((surgical procedure, operative[MESH]) OR (surgical procedure, operative[Title/Abstract])) OR (fracture fixation[MESH])) OR (fracture fixation[Title/Abstract]))). Each title, abstract, and main text of the searched studies were examined if it fulfilled the criteria. Also, reference lists were checked for any other literature that could have met the criteria.
Eligibility criteria
In this study, potential inclusion criteria were as follows: (1) RCTs evaluating the outcomes of conservative versus surgical management in DRFs, (2) participants were cases with a definitive diagnosis of DRFs, (3) studies reporting functional outcomes, (4) data from which participant characteristic outcomes can be extracted, and (5) English-language literature. Exclusion criteria were as follows: (1) protocols, abstracts, letters, or meeting minutes, (2) study subjects were < 18 years old. The inclusion and exclusion criteria of 11 RCT studies are shown in Table S4. Complications were defined as malunion of bone, infection (needle tract infection, superficial wound infection, deep wound infection, Tendon irritation, inflammation and rupture, carpal tunnel syndrome, osteoarthritis), secondary operations (carpal tunnel decompression, corrective osteotomy, tendon repair), fracture displacement, complex regional pain syndrome (CRPS), deep vein thrombosis, damage to blood vessels and nerves, implant-related (failure, irritation), scar adhesion and keloid, and de Quervain syndrome.
Data obtaining
Two researchers independently reviewed all studies collected from the database (Qifan. Yang and Jing. Liu). Using standardized tables, the same researchers extracted all relevant data separately. Another senior reviewer decided on all data discrepancies that cannot be resolved through negotiation (Xinyu. Wang). Basic article features (such as title, first author, year of publication, and study design) were retrieved from each included study, as well as sample characteristics (age, gender, and study population), surgical method, scoring criteria, and follow-up time.
Bias risk assessment
Each study was assessed using the Cochrane Collaboration’s risk of bias tool [10]. The risk of bias for each study was divided into three categories from low to high, according to the guideline. The detailed evaluation process included the following items: (1) sequence generation, (2) allocation concealment, (3) participant blinding, (4) outcome evaluation blinding, (5) evaluation of incomplete outcomes, (6) completeness of data presentation, and (7) other biases. Items were identified as unclear when the information provided was insufficient to warrant their award to objects with a low or high risk of bias.
Study quality assessment
Two reviewers (Qifan. Yang and Guoyong. Cai) separately assessed the strength of information using the Jadad scale [11]. Each included study was given a score from 0 to 5 based on how well it performed on the three components of the Jadad scale (Table S1). Participants were chosen at random, grouping was blinded, and each participant was held accountable. One or two stars were given for “yes” response for “randomization” and “blinding,” and one star was granted for the “yes” answer for “accountability.” Studies with one or two stars were assessed as having low quality to establish a minimum criterion for inclusion in the current study.
Statistical analysis
Discrete variables, such as complications of each group, were estimated and pooled by risk ratio (RR) and appropriate 95% confidence interval (CI). Mean difference (MD) and 95% CI were employed to pool continuous variables, such as wrist range of motion (ROM). The pooled variables were subjected to an inverse variance procedure with a random model. The I2 statistic was used to assess the heterogeneity in each analysis. Heterogeneity in each analysis process was identified as lower (I2 less than 25%), moderate (I2 between 25 and 50%), and higher (I2 more than 50%) [11]. For the process with 50% ≤ I2, Begg’s rank correlation [12] and Egger’s weighted regression method were employed to evaluate the publication biases in the analysis processes. The participants’ characteristics and the outcomes of each group were used to stratify the analysis. Review-Manager was used to complete pooled processes and forest plots (version 5.4, The Cochrane Collaboration, Oxford, UK). A P-value of less than 0.05 was considered to be statistically significant in all analyses.
Results
Study inclusion
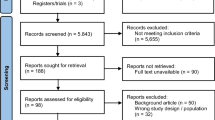
After an initial search, 1436 articles were found in the literature manager, with 216 being eliminated owing to duplication. Most of the remaining articles were removed without conforming to the PICO principles. Finally, 11 studies were chosen from 46 full-text manuscripts for the current investigation. Figure 1 depicts the literature screening procedure.
Study characteristic
A total of 1775 DRFs were included in the current study. The 11 studies were from the UK (n = 2), Pakistan (n = 1), Netherlands (n = 2), Australia (n = 1), Norway (n = 1), USA (n = 1), Finland (n = 1), Sweden (n = 1), and Spain (n = 1). The characteristics of the participants are shown in Table 1.
Risk of bias and quality assessment
The studies examined were deemed to have a low risk of bias and high quality (Fig. 2). The Jadad scale was used as the scoring standard for the 11 RCTS included. The scores were as follows: 4 articles were 4 points, 2 articles were 6 points, and the remaining articles were 7 points. Points were deducted due to a lack of information regarding blinding in some research protocols (Supplementary Table 1).
Meta-analysis of outcome
-
DASH scores (disabilities of the arm shoulder and hand score)
Five RCTs [15, 16, 18, 20, 24] reported DASH score data for 472 patients (Fig. 3). The higher the score, the more disabled and less functional. A score of 0 means normal upper limb function, and a 100 means minimal upper limb function. All patients in the cast group had lower DASH scores than the surgery group after 1 year, with MDs of − 2.55 (95% CI = − 5.02 to − 0.09, P = 0.04). This result was assessed with low heterogeneity (I2 = 42%, P = 0.14) (Fig. 3, Table S3).
The results of sensitivity analysis showed that two experiments [16, 20] had a specific impact on the robustness of the score, which may be related to the sample size and measurement bias. The Egger test result was P = 0.394, with no obvious publication bias. Steady (Table S6).
-
Grip strength
The findings on grip strength were published in four RCTs [15, 16, 19, 24] with a total of 456 individuals (Table S2). There was no significant difference between the cast group and the surgery group, with MDs of 0.24, 95% CI and P values are − 1.8 to 2.28, and the P-value was 0.82. Low heterogeneity was determined (I2 = 0%, P = 0.75) (Table S3).
Sensitivity analysis showed that the overall result of the score was relatively robust. The result of Egger’s test was P = 0.869, with no obvious publication bias (Table S6).
-
EQ-5D-5L(EuroQol five-dimension five-level scale)
The score included three RCTs [15, 19, 22] reporting data on 679 patients (Table S2). There was no significant difference in EQ-5D-5L between the cast group and the surgery group at 1 year after surgery, with an MD of − 0.03 (95% CI = − 0.06 to 0.00, P = 0.05). This result was assessed with low heterogeneity (I2 = 0%, P = 0.83) (Table S3).
Overall, the results of sensitivity analysis showed the scores were relatively robust, and the effects of Egger’s test was P = 0.904, with no significant publication bias (Table S6).
-
EQ-VAS (EuroQol visual analogue scale)
A total of two RCTs [19, 22] reported the following data in Table S2. The results found that the differences between the cast and surgery group were not statistically significant, and heterogeneity was modest (I2 = 0%, P = 0.41), MD = 1.73, P = 0.27, 95% CI = − 1.37 to 4.83 (Table S3).
The sensitivity analysis results show that the overall effect of this score was not robust. Based on previous literature, it is suspected that the result is caused by related factors, such as the small sample size of Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly (CROSSFIRE) Study Group [19]. The result of Egger’s test was P = 0, with a relatively obvious publication bias (Table S6).
-
PRWE (patient-rated wrist evaluation)
As shown in Table S2, PRWE scores were provided in six RCTs [15, 18,19,20, 22, 24], which included 949 patients. Subgroup analyses were performed at 3 months, 6 months, and 1 year after surgery. The pooled results showed that there was no significant difference between the two groups. The data revealed MDs at 1.23, 95% CI: − 1.67 to − 4.14, P = 0.41, and the heterogeneity was high. At 3 months, there was no significant difference. The MDs and 95% CI were − 2.30 (95% CI = − 5.89 to 1.28, P = 0.21), and the heterogeneity was considered to be low at I2 = 0%, P = 0.68, respectively. At 6 months, there was no significant difference. The MDs and 95% CI were − 2.09(95% CI = − 5.53 to 1.35, P = 0.23); the heterogeneity was I2 = 0%, P = 0.42. At 1 year after surgery, the surgery group was 4.88 points higher than the cast group, with a 95% CI of 1.89–7.87, P = 0.01, with high heterogeneity (I2 = 51%, P = 0.07) (Table S3).
Subgroup analysis found that the results showed greater heterogeneity within 1 year, and through sensitivity analysis, we suspected that it was because of the different inclusion criteria of Selles et al. [20], which included more intra-articular fractures (type C1.1), so surgical treatment can achieve better results than conservative treatment. The reported data introduces bias, possibly consistent with the results exhibited by the individual subgroups and the overall results. The result of Egger’s test was P = 0.241, with no significant publication bias (Table S6).
-
ROM (flexion, extension, pronation, supination, radial deviation, and ulna deviation) (Table S3 )
-
o
Flexion
Outcomes at flexion were assessed at 12 months and included a total of four RCTs [15,16,17, 24], including 452 patients. There was no significant difference between the cast group and the surgery group (MD = − 1.09, 95% CI = − 3.63 to 1.46, P = 0.4), which was considered to have low heterogeneity (I2 = 0%, P = 0.42).
-
p
Extension
The data covered four RCTs [15,16,17, 24] with 463 patients. There was no significant difference between the cast group and the surgery group (MD = − 1.06, 95% CI = − 4.51 to 2.39, P = 0.55), which was considered to have low heterogeneity (I2 = 46%, P = 0.13).
-
q
Pronation
The pronation results covered three RCTs [15, 16, 24] with 289 patients. There was no significant difference between the cast group and the surgery group (MD = − 1.07, 95% CI = − 2.94 to 0.80, P = 0.26), which was considered to be highly heterogeneous (I2 = 0%, P = 0.75).
-
r
Supination
A total of three RCTs [15, 16, 24] reported data on supination. The data showed that the difference between the cast group and the surgery group was not statistically significant (MD = − 3.06, 95% CI = − 7.77 to 1.65, P = 0.20), which was considered with high heterogeneity (I2 = 65%, P = 0.06).
-
s
Radial deviation
A total of four RCTs [15,16,17, 24] reported data on radial deviation. The data showed that the difference between the cast group and the surgery group was not statistically significant (MD = 0.56, 95% CI = − 1.74 to 2.87, P = 0.63), which was considered with high heterogeneity (I2 = 59%, P = 0.06).
-
t
Ulna deviation
A total of three RCTs [15, 16, 24] reported data on ulnar deviation. The data showed no statistically significant difference between the cast group and the surgery group (MD = − 1.52, 95% CI = − 3.75 to 0.70, P = 0.18), which was considered with low heterogeneity (I2 = 0%, P = 0.39).
The data showed no statistically significant difference between the cast group and the surgery group (MD = − 0.94, 95% CI = − 2.02 to 0.14, P = 0.09) in ROM; sensitivity analysis showed that the overall results of the ROM score were relatively robust. The result of Egger’s test was P = 0.592, with no significant publication bias (Table S6).
-
o
-
PCS (physical component summary) and MCS (mental component summary)
PCS and MCS data were reported in three RCTs [17, 20, 24] with a total of 347 patients (Table S2). The data showed that there was no significant difference in PCS and MCS between the cast group and the operation group, the MDs were 1.01–4.47, with 95% CI − 0.18 to 2.19 and P values were P = 0.1, − 2.44 to 11.39, P = 0.2. PCS had heterogeneity (I2 = 0%, P = 0.92) and MCS had heterogeneity (I2 = 89%, P = 0.75) (Table S3).
Sensitivity analysis results showed that the PCS and MCS results were less robust, which may be due to the study by Selles, CA [20], and the MCS results were less robust, suspected to be due to Mulders, MAM [24]. Based on literature, it was suspected that the patient’s initial level was related to the subjective reporting results. The Egger test results for PCS and MCS were P = 0.569 and P = 0.373, respectively, with no significant publication bias (Table S6).
Complications
Complication rates were reported for all 1775 patients included in the 11 RCTs [13,14,15,16,17,18,19,20,21,22, 24], and the results are shown in Table S2. Compared with the surgery group, the cast group had a higher incidence of complications, with an RR of 1.63 (95% CI: 1.08–2.45, P = 0.02). The results were rated with high heterogeneity (I2 = 79%, P < 0.00001) (Table S3). The expressly stated complications in the included studies are shown in Table S5. The form can see that the proportion of fracture displacement in the plaster group is relatively large. In the operation group, infection, irritation, and failure of internal fixation need to be paid close attention to.
Sensitivity analysis results were less robust and were suspected to be caused by three studies. According to previous studies, the suspicion was related to different sample sizes and inclusion criteria for complications. The results of Egger’s test had a P = 0.75, with no significant publication bias (Table S6).
Sensitivity analysis and publication bias detection
Through data analysis, some results showed high heterogeneity. We used sensitivity analysis, subgroup analysis, and Egger’s test to explore the source of heterogeneity. It was found that the results are relatively stable, and there was no noticeable difference. The publication bias of the individual results for specific analysis is shown in Table S6.
Discussion
The purpose of this article was to summarize and analyze the research progress and options of cast immobilization and surgical treatment in the management of acute DRFs.
The overall results showed that there was a significant difference in DASH score between the cast group and surgical group MDs = –2.55 (95% CI = –5.02 to –0.09, P = 0.04). With low heterogeneity, the results of DASH scores have higher credibility. The results of data analysis suggest that the recovery of upper limb function in the cast group is better than that in the surgical group. The summarized results of DASH scores are consistent with the hypothetical results of this article, which supports the decision of cast immobilization after the operation of distal radius fracture. It also outlines the evidence related to the incidence of complications after treatment of DRFs at 3 months, 6 months, and above. The cast fixation group had a higher incidence of complications than the surgical group, and the difference was statistically significant. In the heterogeneity analysis section, the results and significance of the specific sensitivity analysis are presented.
Furthermore, according to our findings, there was no substantial change in grip strength, EQ-5D-5L, EQ-VAS, or other indexes between the cast and surgical groups. Although both EQ-VAS studies can be used to analyze high-quality literature, it may not be enough to provide more convincing results due to the limitation of sample size, so it is difficult to conclude that this index provides adequate evidence for clinicians’ decision-making. Therefore, cast therapy may bring better benefits to patients with adult and elderly DRFs than surgical treatment.
The DASH results of the current meta-analysis are consistent with the results of previous studies [16, 20], which support that cast treatment is better than surgical treatment. However, the results of this meta-analysis and Mulders et al. [24] differed from the findings of Selles et al. [20], which mainly included patients with intra-articular fracture displacement of the distal radius (complete joint type C1.1), and closed reduction is acceptable [20]. The patients included in this meta-analysis were confirmed cases of DRFs. Considering that different fracture types may be specific, it will impact the long-term DASH score. In addition, Yifan Chen (2020) believes that surgical treatment of DRFs is better than cast treatment in ROM [25]. This meta-analysis showed no significant difference after 1-year follow-up. This evidence is consistent that of other studies [18, 26].
Regarding ROM, this study does not support the evidence that surgical treatment is more valuable than cast treatment. We performed a meta-analysis of PRWE scores at 3, 6, and 12 months after operation by collecting the data of 6 RCTs [15, 19,20,21, 23, 24]. The results showed that many patients with wrist fractures had no significant difference between 3 and 6 months after surgery. After 1 year, the scores of surgical treatment and conservative treatment began to show statistical differences. However, the follow-up results after 1 year were highly heterogeneous, which was difficult to provide analytical results. This meta-analysis was then verified by subgroup analysis using a random-effect model to investigate the origins of heterogeneity. It was found that except for C.A. Sellers (2021) [20] the literature had high heterogeneity. It was considered that different inclusion criteria may have caused high heterogeneity. Regarding ROM, this study believes that DRFs treated with cast can achieve the same effect as surgical treatment. In some studies, the heterogeneity of supination and radial deviation in the ROM score may also be derived from the difference in the time of wrist movement after DRF. Marjolein A.M [20] mentioned that for patients who underwent DRF surgery, the management of postoperative pain allows the movement of the wrist. For patients treated with DRF surgery, Simio K [16] used a back cast to relieve pain for 10 days, after which the patient received formal guidance to move the wrist actively. The difference in the wrist joint’s braking time and activity time after surgery may have a specific impact on the speed and degree of fracture healing and joint activity recovery.
The author discovered that in adult DRFs, the surgical group had a significantly lower rate of complications than the cast group. However, due to its diversity, sensitivity analysis reveals that the results are consistent, implying that the results are very stable and that there is no noticeable publishing offset, meaning that the findings of this study are highly credible. This evidence differs from the findings of some RCTs [15, 18, 19, 22, 26, 27], which prefer conservative treatment and surgical treatment, and there is no significant statistical difference in complications. The evidence of difficulties in this paper is consistent with [21]. Although surgical treatment has a lower incidence of complications, there is no significant difference between cast treatment and surgical treatment in ROM, grip strength, EQ-5D-5L, EQ-VAS, and so on. An in-depth cost analysis of the DRFs fixation trial (draft) [27] showed that low-cost fixation could provide similar results to ORIF. In addition, a newly published guide on DRFs in the USA [3] provides strong evidence that compared to nonoperative treatment, surgical treatment for geriatric patients (65 years and older) does not result in improved long-term patient-reported outcomes (strong strength). Therefore, at present, we still cannot conclude that surgical treatment can bring better prognosis to such patients.
Our meta-analysis included 11 RCTs for general analysis, of which nine were RCT studies published in the recent 3 years. According to the Jadad scale, four RCTs were scored 4 points, two RCTs scored 6 points, and the remaining RCTs scored 7 points. The included RCTs provided high-quality evidence for treating DRFs in adults. Although the main reason for score deduction of some studies was no information provided regarding blinding, the RCT studies with the lowest score on the Jadad scale are still of high quality. We then tested the publication bias of each index with the Egger test, and the results showed that there was no obvious publication bias, indicating that the results of this article are highly reliable.
Our meta-analysis mainly included patients with DRFs in adults and the elderly, but not children. Considering that the bone density and bone mass of adults and the elderly are different from those of children, the fracture healing speed and bone remodeling of children are faster than those of adults. Many studies have found a strong link between functional and anatomical outcomes in young children who are highly functional and active; hence, we excluded RCTs which involved children. The 11 RCTs included in this meta-analysis are mainly articles published in developed countries such as North America and Europe. Neither research included in the review mentioned whether or not the patients had any additional illnesses. Because it has the potential to cause or contribute to negative repercussions, as a result, this component may cause heterogeneity and possibly diminish the results' dependability.
Conclusion
The current study evaluated the outcomes of cast immobilization and surgery for DRFs. It was analyzed that the cast group exhibited better results in DASH than the surgery group at 1-year follow-up, with no significant differences in ROM, PRWE, and grip strength. In terms of complications, the surgical group showed the lower complication rate within 1 year after surgery. Cast immobilization can reduce the financial burden of a considerable number of patients. Therefore, this study may provide better evidence support for future clinicians to use cast immobilization for DRFs. In the literature included in this article, some of the patients included in the RCT studies had type C fractures. However, most were AO-C1 fractures, which can maintain good stability after reduction, so it still has guiding significance for the treatment of uncomplicated DRF patients. However, the included sample size is far from enough compared with the global incidence of DRF. Therefore, higher quality and more extensive sample size studies are needed in the future for simple DRF fractures and AO-C fractures to improve the reliability of the evidence. For details, see Table S7.
Abbreviations
- DRFs:
-
Distal radius fractures
- RCTs:
-
Randomized controlled trials
References
Reid SA, Andersen JM, Vicenzino B (2020) Adding mobilisation with movement to exercise and advice hastens the improvement in range, pain and function after non-operative cast immobilisation for distal radius fracture: a multicentre, randomised trial. J Physiother 66(2):105–112. https://doi.org/10.1016/j.jphys.2020.03.010
Sanders KM, Nicholson GC, Ugoni AM, Pasco JA, Seeman E, Kotowicz MA (1999) Health burden of hip and other fractures in Australia beyond 2000. Projections based on the Geelong Osteoporosis Study. Med J Aust 170(10):467–470. https://doi.org/10.5694/j.1326-5377.1999.tb127845.x
Shapiro LM, Kamal RN, Management of Distal Radius Fractures Work Group, Nonvoting Clinical Contributor, Nonvoting Oversight Chairs, Staff of the American Academy of Orthopaedic Surgeons and the American Society for Surgery of the Hand (2021) Distal radius fracture clinical practice guidelines-updates and clinical implications. J Hand Surg Am 46(9):807–811. https://doi.org/10.1016/j.jhsa.2021.07.014
Mellstrand-Navarro C, Pettersson HJ, Tornqvist H, Ponzer S (2014) The operative treatment of fractures of the distal radius is increasing: results from a nationwide Swedish study. Bone Joint J 96-B(7):963–969. https://doi.org/10.1302/0301-620X.96B7.33149
Armstrong KA, von Schroeder HP, Baxter NN, Zhong T, Huang A, McCabe SJ (2019) Stable rates of operative treatment of distal radius fractures in Ontario, Canada: a population-based retrospective cohort study (2004–2013). Can J Surg 62(6):386–392. https://doi.org/10.1503/cjs.016218
Rai P, Haque A, Abraham A (2020) A systematic review of displaced paediatric distal radius fracture management: plaster cast versus Kirschner wiring. J Clin Orthop Trauma 11(2):275–280. https://doi.org/10.1016/j.jcot.2019.03.021
Holbrook HS, Doering TA, Mauck BM (2021) Common complications of distal radial fractures. Orthop Clin North Am 52(3):241–250. https://doi.org/10.1016/j.ocl.2021.03.009
Pidgeon TS, Casey P, Baumgartner RE, Ferlauto H, Ruch DS (2020) Complications of volar locked plating of distal radius fractures: a prospective investigation of modern techniques. Hand (N Y) 15(5):698–706. https://doi.org/10.1177/1558944719828001
Lauder A, Hanel DP (2017) Spanning Bridge Plate Fixation of Distal Radial Fractures. JBJS Rev 5(2):e2. https://doi.org/10.2106/JBJS.RVW.16.00044
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101. https://doi.org/10.2307/2533446
Azzopardi T, Ehrendorfer S, Coulton T, Abela M (2005) Unstable extra-articular fractures of the distal radius: a prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br 87(6):837–840. https://doi.org/10.1302/0301-620X.87B6.15608
Martinez-Mendez D, Lizaur-Utrilla A, de-Juan-Herrero J, (2018) Intra-articular distal radius fractures in elderly patients: a randomized prospective study of casting versus volar plating. J Hand Surg Eur 43(2):142–147. https://doi.org/10.1177/1753193417727139
Saving J, Severin Wahlgren S, Olsson K, Enocson A, Ponzer S, Sköldenberg O, Wilcke M, Mellstrand Navarro C (2019) Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: a randomized controlled trial. J Bone Joint Surg Am 101(11):961–969. https://doi.org/10.2106/JBJS.18.00768
Sirniö K, Leppilahti J, Ohtonen P, Flinkkilä T (2019) Early palmar plate fixation of distal radius fractures may benefit patients aged 50 years or older: a randomized trial comparing 2 different treatment protocols. Acta Orthop 90(2):123–128. https://doi.org/10.1080/17453674.2018.1561614
Chung KC, Kim HM, Malay S, Shauver MJ, Wrist and Radius Injury Surgical Trial Group (2020) The wrist and radius injury surgical trial: 12-month outcomes from a multicenter international randomized clinical trial. Plast Reconstr Surg 145(6):1054e–1066e. https://doi.org/10.1097/PRS.0000000000006829
Hassellund SS, Williksen JH, Laane MM, Pripp A, Rosales CP, Karlsen Ø, Madsen JE, Frihagen F (2021) Cast immobilization is non-inferior to volar locking plates in relation to QuickDASH after one year in patients aged 65 years and older: a randomized controlled trial of displaced distal radius fractures. Bone Joint J 103-B(2):247–255. https://doi.org/10.1302/0301-620X.103B2.BJJ-2020-0192.R2
Lawson A, Naylor JM, Buchbinder R, Ivers R, Balogh ZJ, Smith P, Xuan W, Howard K, Vafa A, Perriman D, Mittal R, Yates P, Rieger B, Smith G, Adie S, Elkinson I, Kim W, Sungaran J, Latendresse K, Wong J, Viswanathan S, Landale K, Drobetz H, Tran P, Page R, Beattie S, Mulford J, Incoll I, Kale M, Schick B, Li T, Higgs A, Oppy A, Harris IA, Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly (CROSSFIRE) Study Group (2021) Surgical plating vs closed reduction for fractures in the distal radius in older patients: a randomized clinical trial. JAMA Surg 156(3):229–237. https://doi.org/10.1001/jamasurg.2020.5672
Selles CA, Mulders MAM, Winkelhagen J, van Eerten PV, Goslings JC, Schep NWL, Collaborators VIPAR (2021) Volar plate fixation versus cast immobilization in acceptably reduced intra-articular distal radial fractures: a randomized controlled trial. J Bone Joint Surg Am 103(21):1963–1969. https://doi.org/10.2106/JBJS.20.01344
Tahir M, Khan Zimri F, Ahmed N, Rakhio Jamali A, Mehboob G, Watson KR, Faraz A (2021) Plaster immobilization versus anterior plating for dorsally displaced distal radial fractures in elderly patients in Pakistan. J Hand Surg Eur 46(6):647–653. https://doi.org/10.1177/1753193420977780
Costa ML, Achten J, Ooms A, Png ME, Cook JA, SE., L. (2022) Surgical fixation with K-wires versus casting in adults with fracture of distal radius: DRAFFT2 multicentre randomised clinical trial. BMJ 376:o580. https://doi.org/10.1136/bmj.o580
Martinez-Mendez D, Lizaur-Utrilla A, de Juan-Herrero J (2018) Prospective study of comminuted articular distal radius fractures stabilized by volar plating in the elderly. Int Orthop 42(9):2243–2248. https://doi.org/10.1007/s00264-018-3903-1
Mulders MAM, Walenkamp MMJ, van Dieren S, Goslings JC, Schep NWL, Trial Collaborators VIPER (2019) Volar plate fixation versus plaster immobilization in acceptably reduced extra-articular distal radial fractures: a multicenter randomized controlled trial. J Bone Joint Surg Am 101(9):787–796. https://doi.org/10.2106/JBJS.18.00693
Chen Y, Lin C, Huang X, Lin F, Luo X (2021) Comparison of treatment results between surgical and conservative treatment of distal radius fractures in adults: a meta-analysis of randomized controlled trials. Acta Orthop Traumatol Turc 55(2):118–126. https://doi.org/10.5152/j.aott.2021.20168
Yu GS, Lin YB, Le LS, Zhan MF, Jiang XX (2016) Internal fixation vs conservative treatment for displaced distal radius fractures: a meta-analysis of randomized controlled trials. Ulus Travma Acil Cerrahi Derg 22(3):233–241. https://doi.org/10.5505/tjtes.2015.05995
Chen Y, Chen X, Li Z, Yan H, Zhou F, Gao W (2016) Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: a systematic review and meta-analysis. J Hand Surg Am 41(3):404–413. https://doi.org/10.1016/j.jhsa.2015.12.008
Acknowledgements
Dong. Zhu and Qifan. Yang conceived the design of this manuscript. Qifan. Yang and Guoyong. Cai screened out eligible studies separately. Qifan. Yang and Jing. Liu accomplished data collection, analysis of results, and editing of the final manuscript. Dong Zhu discussed the controversial parts of literature screening and quality evaluation. Dong. Zhu and Xinyu. Wang supervised the entire process and revised the manuscript. All the authors have read and approved the manuscript.
Funding
The authors thank the National Natural Science Foundation of China (Grant numbers: No12072129) for the financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yang, Q., Cai, G., Liu, J. et al. Efficacy of cast immobilization versus surgical treatment for distal radius fractures in adults: a systematic review and meta-analysis. Osteoporos Int 34, 659–669 (2023). https://doi.org/10.1007/s00198-022-06649-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06649-8