Abstract
Summary
Osteoporosis is an underdiagnosed disease that results in bone fragility and risk of fractures. Fracture Liaison Service (FLS) is a secondary prevention model which identifies patients at risk for fragility fractures. The introduction of a FLS protocol showed an increase of anti-osteoporotic drug prescription and significant reduction of all-cause mortality.
Introduction
Hip fractures are the most severe osteoporotic fracture due to their associated disability and elevated risk of mortality. FLS programs have enhanced the management of osteoporosis-related fractures. Our objective is to analyze the effect of the FLS model over survival and 2-year mortality rate following a hip fracture.
Methods
We conducted a prospective cohort study on patients over 60 years of age who suffered a hip fracture during 3 consecutive years, before and after the implementation of the FLS in our center (i.e., between January 2016 and December 2018). Patients’ information was withdrawn from our local computerized database. Patients were followed for 2 years after the hip fracture. Mortality and re-fracture rates were compared between the two groups using a multivariate Cox proportional hazard model.
Results
A total of 1101 patients were included in this study (i.e., 357 before FLS implementation and 744 after FLS implementation). Anti-osteoporotic drugs were more frequently prescribed after FLS implementation (583 (78.4%) vs 44 (12.3%); p < 0.01). There was an increase of adherence to treatment after FLS implementation (227 (38.9%) vs 12 (3.3%); p = 0.03). A total of 222 (29.8%) patients after FLS implementation and 114 (31.9%) individuals before FLS implementation (p = 0.44) died during the follow-up period. A second fracture occurred in 49 (6.6%) patients after FLS implementation and in 26 (7.3%) individuals before FLS implementation (p = 0.65). Patients who were treated with anti-osteoporotic drugs after the implementation of the FLS protocol had a lower all-cause 1-year and 2-year mortality compared with patients managed before the implementation of the FLS protocol (adjusted hazard ratio (HR) 0.75, 95% confidence interval (CI) 0.59–0.96; HR 0.87, 95% CI 0.69–1.09, respectively).
Conclusions
The implementation of a FLS protocol was associated with an increase of anti-osteoporotic treatment, higher adherence, and greater survival in elderly hip fracture patients. There was a significant reduction of all-cause mortality in the FLS patients treated with anti-osteoporotic. However, the application of the FLS did not affect the risk of suffering a second fragility fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is an underdiagnosed disease which is characterized by a low bone density, increased bone fragility, and subsequently a higher risk of fracture [1]. The total number of fragility fractures in six western European countries (i.e., France, Germany, Italy, Spain, the UK, and Sweden) could be increased from 2.7 million in 2017 to 3.3 million in 2030 [2]. Hip fractures are the most serious fragility fractures due to their associated disability, higher hospitalization costs, and high mortality rates [3]. However, due to the poor worldwide secondary prevention organization, osteoporotic treatment is initiated in a low number of hip fracture patients [4].
In 2012, the International Osteoporosis Foundation (IOF) facilitated the implementation of Fracture Liaison Service (FLS) globally, which is a post-fracture model of care that identifies all patients who have a higher risk of a secondary fracture [5]. FLS programs have enhanced the management of osteoporosis-related fractures, have shown their clinical effectiveness, and minimized the burden of this disease [6]. Nevertheless, the success of FLS depends on its organization and structure; and better results are obtained when this model of care provides a holistic management of the patient [7].
Our research team conducted a previous study in which we observed that the implementation of the FLS improved the 1-year overall survival of patients with hip fractures compared with that of those not subjected to the FLS protocol [8]. Accordingly, this study is a continuation of our previous research, in which we prolonged the post-FLS implementation follow-up period to 2 years. We hypothesize that the use of an intensive FLS model of care in our institution could improve the survivorship of elderly hip fracture patients. Therefore, the primary aim of this study was to analyze the effect of the FLS model over the survival and the first-year and second-year mortality rates following a hip fracture. The secondary aim was to determine the risk of suffering a second osteoporotic fracture and the adherence to treatment.
Methods
Study design
A prospective cohort study was conducted on hip fracture patients over 60 years old, who were treated in our institution between January 2016 and December 2018. The first group of patients were diagnosed between January 2016 and December 2016, before the implementation of the FLS. Patients in the second group were diagnosed between January 2017 and December 2018, after the implementation of the FLS protocol. Patient’s records were withdrawn from the regional public Andalusian healthcare system database, which is linked to the national Spanish mortality registry. Patients with pathological fractures (i.e., osteomalacia, Paget’s disease, history of malignancy) were excluded from the study. The following information was collected from our local computerized database: age, gender, American Society of Anesthesiologists (ASA) score, fracture side, type of fracture (femoral neck, trochanteric or subtrochanteric), type of surgical treatment (i.e., cannulated screws, proximal femoral nail, hemiarthroplasty, or total hip replacement), and initiation, use, and adherence of anti-osteoporotic drugs. Patients were followed from the date of the initial hip fracture (index date) until death of any cause, or end of the 2-year follow-up. Second osteoporotic fractures (i.e., contralateral hip, distal radius, proximal humerus, and vertebral fractures) were considered secondary outcomes. Exposure to drugs used for treatment of osteoporosis was assessed only if these were used at any point after the index date.
FLS protocol
Before the implementation of the FLS protocol, patients received a standard fracture care during hospitalization. Patients had an outpatient visit 1 month after the index date and further visits were scheduled depending on the evolution of the patients’ and surgeons’ preferences.
On the other hand, FLS patients followed the protocol previously described by our institution [8]. Briefly, patents underwent a series of laboratory tests during the inpatient period (including a basic biochemistry test, calcium serum levels, albumin, vitamin D, among others). In addition, mobility was assessed using the functional ambulation category (FAC) scale and autonomy was evaluated using Barthel’s scale. During the inpatient period, medical comorbidities were treated and physical therapy was started. All patients and their carers received an exercise program. Osteoporotic treatment was started on discharge according to the European guidance for diagnosis and management of osteoporosis, and the recommendations of the International Osteoporosis Foundation (IOF) [9], including calcium and vitamin D supplements. Oral bisphosphonates (i.e., alendronic acid and risedronate) were not prescribed in patients with renal impairment or gastric intolerance. In those subjects, subcutaneous denosumab was prescribed. Teriparatide was prescribed in cases with severe osteoporosis. Patients had outpatient visit appointment after 1, 6, and 12 months from the index date. In these visits, Barthel’s and FAC scales were repeated, fracture care was received, and potential health issues were identified.
Statistical analysis
Data were analyzed with SPSS 24.0 software (SPSS Inc., Chicago, IL, USA), and G*power 3.1.9.6 (Universität Kiel, Germany). Categorical variables were presented as absolute values and percentages. Means were presented with their corresponding standard deviations (SD). The distribution of the continuous variables was assessed using the Shapiro–Wilk test. Differences between the demographic features were analyzed using Student’s t and chi-square tests. Patient survival was determined using a Kaplan–Meier survivorship analysis. Two different analyses were performed. First is a survival analysis where the outcomes were either death or end of a 24-month follow-up; here patients lost to follow-up were censored. The second analysis was done to estimate the risk of a second fracture to the end of the 24-month follow-up period; in this analysis, deaths and patients lost to follow-up were censored to avoid possible bias. Mortality and second osteoporotic fracture rates were compared between the two groups using a multivariate Cox proportional hazard model adjusted to potential confounders: age, gender, type of fracture, ASA score, and anti-osteoporotic drug treatment. Post hoc power analyses for Student’s t and chi-square tests were used with an α-error probability of 0.05.
Results
A total of 1101 patients fulfilled the inclusion–exclusion criteria (239 males and 862 females) (Table 1). The mean patient age was 82.43 ± 7.84 years (i.e., before FLS implementation 82.36 ± 8.20, and after FLS implementation 82.49 ± 7.66, p = 0.29). The FLS protocol was initiated in 674 patients from a total of 744 (90.6%) patients during the implementation period. Anti-osteoporotic treatment was given in 44 cases (12.3%) before FLS implementation, compared to 583 (78.4%) patients after FLS implementation (odds ratio (OR) of 9.37 (7.00–12.55), p < 0.01). There were no statistically significant comorbidity differences between the two groups (ASA scale 2.58 ± 0.70 vs. 2.54 ± 0.62, p = 0.44) (Table 1). However, overall survival was higher after the implementation of the FLS protocol compared to that in the period before its implementation (i.e., 598.02 ± 235.59 vs. 568.51 ± 260.47 days respectively, p < 0.01, power 95%) (Table 1).
In total, 336 patients (30.52%) died during the 2-year follow-up period: 114 patients (31.9%) before FLS implementation and 222 patients (29.8%) after FLS implementation (p = 0.44) (Table 1). A total of 75 patients (6.8%) suffered a second osteoporotic fracture: 26 patients (7.3%) before FLS implementation and 49 patients (6.6%) after FLS implementation (p = 0.65), from which 30 (2.7%) were contralateral hip fractures (i.e., 10 (2.8%) and 20 (2.7%) in each group, respectively) (Table 1). There was an increase of adherence to treatment after FLS implementation (30.5%) compared to adherence before its application (3.3%) (p = 0.03) (Table 1).
There was a widespread deficiency of albumin (2.66 ± 0.62 g/dL) and vitamin D (14.09 ± 10.83 ng/dL) levels in the FLS cohort. These levels worsened as the age of the patients increased (Table 2). Moreover, we found a deficiency of vitamin D in 95% of these hip fracture patients (38.7% with severe deficiency, 42.7% with moderate deficiency, and 13.6% with relative deficiency) (Fig. 1).
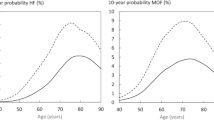
The Cox proportional hazard model showed an adjusted 1-year and 2-year hazard ratio (HR) for all-cause mortality of 0.76 (95% CI 0.58–0.98) and 0.87 (95% CI 0.69–1.09) in patients treated after the implementation of the FLS protocol compared with individuals treated before the implementation of the FLS protocol, respectively. The second osteoporotic fracture HR was 0.84 (95% CI 0.52–1.36) (Table 3; Figs. 1 and 2).
Patients included in the FLS protocol after its implementation in our department had an adjusted 1-year mortality HR of 0.72 (95% CI 0.55–0.97) and adjusted 2-year mortality HR of 0.86 (95% CI 0.68–1.08) compared with all individuals treated before its implementation (treated or not treated with anti-osteoporotic drugs) (Table 4). The Cox proportional hazard model showed significant all-cause 1-year mortality HR of 0.60 (0.45–0.81) and 2-year mortality HR of 0.75 (0.59–0.96) in the FLS patients treated with anti-osteoporotic drugs compared with all patients before FLS implementation (treated or not treated with anti-osteoporotic drugs) (Table 4; Fig. 2). No differences in the risk of suffering a second osteoporotic fracture were found between patients treated before FLS implementation and individuals included in the FLS protocol, those included and treated with anti-osteoporotic drugs, or patients included but not treated with anti-osteoporotic drugs (Table 4).
Discussion
In the present study, we observed a significant increase in the 2-year survival following a hip fracture in patients subjected to the FLS protocol who were treated with anti-osteoporotic drugs. Moreover, patients included in the FLS protocol in our department had an adjusted 1-year mortality hazard ratio lower than those individuals treated before its implementation. A recent survival analysis showed that hip fracture patients had a lower life expectancy compared to the general population and their high risk of dying remained constant [10]. A larger study also showed that hip fracture is associated with excess short- and long-term all-cause mortality in both sexes [11]. In addition, patients with multiple fractures had an increase in the incidence of mortality in a provincial Canadian FLS program suggesting the special attention required for these individuals [12]. Furthermore, hip fracture patient survival is related with the presence of comorbidities at 2 years of follow-up [13]. A recent systematic review and meta-analysis conducted on Fracture Liaison Services demonstrated a lower probability or subsequent fractures and mortality [14].
Another finding of the present study was the increase of prescription of anti-osteoporotic drugs with the implementation of the FLS program. Previous studies have shown that the use of anti-osteoporotic medications for the secondary prevention after a hip fracture was low, regardless of sex, age, comorbidities, or healthcare system [15, 16]. The use of these drugs could be incremented in different ways. The prescription of anti-osteoporotic drugs during the hip fracture hospitalization period greatly improves the possibilities of receiving treatment [17]. The implementation of a FLS protocol also increases the rates of osteoporotic treatment [6].
On the other hand, our study showed that the implementation of the FLS program significantly increased the adherence of hip fracture patients to osteoporotic treatment. Despite this favorable result, a greater adherence than 40% should be achieved [18]. Another recent study from a French institution showed an estimated persistence with any class of osteoporotic medication of 84% [19]. Improving adherence to osteoporosis medication is a challenging issue where multicomponent interventions with active patient involvement are the most effective strategy to increase adherence [18]. Many factors are associated with poorer medication adherence: lower education and activity levels, higher age, higher treatment cost and dosing frequency and medication-related side effects, and patient care under different medical specialties [20].
We found a lower mortality in hip fracture patients treated with anti-osteoporotic medication in the context of a FLS program. These results are in consonance with a nationwide study that showed a reduction of mortality after hip fracture among patients treated with antiresorptive therapy [21]. It seems that osteoporotic treatment, especially bisphosphonates, may be related with a decreased risk of death following a fragility fracture [22]. In addition, the maintenance of optimal vitamin D levels may be associated with a decrease risk of mortality and several types of chronic diseases [23]. Additionally, calcium supplements (alone or with concomitant vitamin D) would not be recommended in those individuals with normal calcium intake due to the potential adverse cardiovascular effects [24].
However, we did not find a reduction in the second fragility fracture rate in hip fracture patients after the implementation of the FLS protocol at 2 years of follow-up. This finding is not in concordance with other studies that showed a significant reduction of second osteoporotic fracture rates. A previous study reported a lower incidence of hip, vertebral, and wrist fractures in the subsequent 12-month period in patients who were treated for osteoporosis [25]. However, another study suggested that FLS programs may have a limited value in reducing subsequent fractures in patients > 85 years [26]. Moreover, it seems that studies performed on FLS programs had heterogeneous designs and study populations. Therefore, further studies are needed to determinate the effect of FLS protocols on subsequent fracture risk [27].
The hip fracture event is often the first opportunity for the treatment of the osteoporosis in elderly patients. However, there is no specific age to treat osteoporosis. Osteoporotic treatment is safe and may even be particularly effective in the mortality and morbidity reduction in hip fracture patients [28]. Furthermore, the absolute risk of atypical femoral fractures remained low compared with risks of other fragility fractures [29]. However, the recent COVID-19 pandemic has significantly disrupted Fracture Liaison Service programs and may have contributed to an increase fragility fracture rates in elderly patients [30].
Nevertheless, there were several limitations to the present study. Firstly, this was an observational study, and further randomized controlled studies would be recommended to determine the efficacy of FLS protocols. However, such studies could face ethical issues because FLS protocols have already shown to achieve better outcomes when compared with the traditional management of these patients. Secondly, the sample size of the pre-intervention cohort population was relatively smaller than of the FLS cohort population. However, the statistical power of our results was above 90%. Finally, the follow-up period in this study was limited to 2 years. Therefore, the conduction of further studies, with longer follow-up periods, would be recommended to evaluate the long-term effects of the FLS protocols on hip fracture patients.
This study also has strengths. To the best of our knowledge, this is the first study to report an association between the implementation of an intensive FLS model and the reduction of the 2-year mortality rate of patients with hip fractures in a single hospital. The prospective design of this study would not be expected to introduce significant selection bias. In addition, the results of this study were adjusted to potential confounders that could influence mortality, using a Cox proportional hazard model.
Conclusions
The implementation of a FLS protocol was associated with an increase of anti-osteoporotic drug prescription and adherence to this treatment in elderly hip fracture patients. We found a higher survival of these patients after FLS protocol implementation. Moreover, our study showed a significant reduction of all-cause mortality in the FLS patients treated with anti-osteoporotic drugs compared with all patients before FLS implementation. However, we found no differences in the risk of suffering a second osteoporotic fracture.
References
Johnston CB, Dagar M (2020) Osteoporosis in older adults. Med Clin North Am 104:873–884. https://doi.org/10.1016/j.mcna.2020.06.004
for the International Osteoporosis Foundation, Borgström F, Karlsson L et al (2020) Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos 15:59. https://doi.org/10.1007/s11657-020-0706-y
Veronese N, Maggi S (2018) Epidemiology and social costs of hip fracture. Injury 49:1458–1460. https://doi.org/10.1016/j.injury.2018.04.015
Kim SC, Kim M-S, Sanfélix-Gimeno G et al (2015) Use of osteoporosis medications after hospitalization for hip fracture: a cross-national study. Am J Med 128:519-526.e1. https://doi.org/10.1016/j.amjmed.2015.01.014
IOF Fracture Working Group, Åkesson K, Marsh D et al (2013) Capture the fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152. https://doi.org/10.1007/s00198-013-2348-z
Wu C-H, Tu S-T, Chang Y-F et al (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone 111:92–100. https://doi.org/10.1016/j.bone.2018.03.018
Shipman KE, Doyle A, Arden H et al (2017) Development of fracture liaison services: what have we learned? Injury 48:S4–S9. https://doi.org/10.1016/j.injury.2017.08.030
González-Quevedo D, Bautista-Enrique D, Pérez-del-Río V et al (2020) Fracture liaison service and mortality in elderly hip fracture patients: a prospective cohort study. Osteoporos Int 31:77–84. https://doi.org/10.1007/s00198-019-05153-w
on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF), Kanis JA, Cooper C et al (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44. https://doi.org/10.1007/s00198-018-4704-5
Barahona M, Barrientos C, Cavada G et al (2020) Survival analysis after hip fracture: higher mortality than the general population and delayed surgery increases the risk at any time. Hip Int 30:54–58. https://doi.org/10.1177/1120700020938029
Katsoulis M, Benetou V, Karapetyan T et al (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281:300–310. https://doi.org/10.1111/joim.12586
the Ontario Osteoporosis Strategy Fracture Screening and Prevention Program Evaluation Team, Sujic R, Luo J et al (2020) Multiple simultaneous fractures are associated with higher all-cause mortality: results from a province-wide fracture liaison service. Osteoporos Int 31:291–296. https://doi.org/10.1007/s00198-019-05207-z
González Quevedo D, Mariño IT, Sánchez Siles JM et al (2017) Patient survival and surgical re-intervention predictors for intracapsular hip fractures. Injury 48:1831–1836. https://doi.org/10.1016/j.injury.2017.06.014
Li N, Hiligsmann M, Boonen A et al (2021) The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int 32:1517–1530. https://doi.org/10.1007/s00198-021-05911-9
Kristensen PK, Ehrenstein V, Shetty N, Pedersen AB (2019) Use of anti-osteoporosis medication dispensing by patients with hip fracture: could we do better? Osteoporos Int 30:1817–1825. https://doi.org/10.1007/s00198-019-05066-8
Chau YT, Nashi N, Law LS-C et al (2020) Undertreatment of osteoporosis following hip fracture: a retrospective, observational study in Singapore. Arch Osteoporos 15:141. https://doi.org/10.1007/s11657-020-00816-2
Kuiper BW, Graybill S, Tate JM et al (2018) After the fall: improving osteoporosis treatment following hip fracture. Osteoporos Int 29:1295–1301. https://doi.org/10.1007/s00198-018-4416-x
On behalf of the European Society for Clinical and Economic Aspect of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO), Cornelissen D, de Kunder S et al (2020) Interventions to improve adherence to anti-osteoporosis medications: an updated systematic review. Osteoporos Int 31:1645–1669. https://doi.org/10.1007/s00198-020-05378-0
Delbar A, Pflimlin A, Delabrière I et al (2021) Persistence with osteoporosis treatment in patients from the Lille University Hospital Fracture Liaison Service. Bone 144:115838. https://doi.org/10.1016/j.bone.2020.115838
Yeam CT, Chia S, Tan HCC et al (2018) A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int 29:2623–2637. https://doi.org/10.1007/s00198-018-4759-3
Brozek W, Reichardt B, Zwerina J et al (2016) Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: a nationwide study. Osteoporos Int 27:387–396. https://doi.org/10.1007/s00198-015-3415-4
Sattui SE, Saag KG (2014) Fracture mortality: associations with epidemiology and osteoporosis treatment. Nat Rev Endocrinol 10:592–602. https://doi.org/10.1038/nrendo.2014.125
Charoenngam N, Shirvani A, Holick MF (2019) Vitamin D for skeletal and non-skeletal health: what we should know. J Clin Orthop Trauma 10:1082–1093. https://doi.org/10.1016/j.jcot.2019.07.004
Chiodini I, Bolland MJ (2018) Calcium supplementation in osteoporosis: useful or harmful? Eur J Endocrinol 178:D13–D25. https://doi.org/10.1530/EJE-18-0113
Yusuf AA, Cummings SR, Watts NB et al (2018) Real-world effectiveness of osteoporosis therapies for fracture reduction in post-menopausal women. Arch Osteoporos 13:33. https://doi.org/10.1007/s11657-018-0439-3
Sanli I, van Helden SH, ten Broeke RHM et al (2019) The role of the Fracture Liaison Service (FLS) in subsequent fracture prevention in the extreme elderly. Aging Clin Exp Res 31:1105–1111. https://doi.org/10.1007/s40520-018-1054-2
de Bruin IJA, Wyers CE, van den Bergh JPW, Geusens PPMM (2017) Fracture liaison services: do they reduce fracture rates? Ther Adv Musculoskelet Dis 9:157–164. https://doi.org/10.1177/1759720X17706464
Vandenbroucke A-M, Luyten F, Flamaing J, Gielen E (2017) Pharmacological treatment of osteoporosis in the oldest old. CIA 12:1065–1077. https://doi.org/10.2147/CIA.S131023
Black DM, Geiger EJ, Eastell R et al (2020) Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates. N Engl J Med 383:743–753. https://doi.org/10.1056/NEJMoa1916525
Kong SH, Hwang BK, Yoon B-H (2021) The impact of COVID-19 on the optimal management of osteoporosis. J Bone Metab 28:115–122. https://doi.org/10.11005/jbm.2021.28.2.115
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
David González-Quevedo, Verónica Pérez-del-Rio, Diego Moriel-Garceso, Naiara Fernandez-Arroyabe, Gaspar Garcia-Melendez, Mario Montañez-Ruiz, Manuel Bravo-Bardají, and David García-de-Quevedo have received in the last 5 years honoraria for lecture fees or financial support for attending symposia from Lilly, Gedeon-Richter, and Amgen.
Iskandar Tamimi reports no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Clinical Evidence: 2
Rights and permissions
About this article
Cite this article
González-Quevedo, D., Pérez-del-Río, V., Moriel-Garceso, D. et al. A 2-year follow-up of a novel Fracture Liaison Service: can we reduce the mortality in elderly hip fracture patients? A prospective cohort study. Osteoporos Int 33, 1695–1702 (2022). https://doi.org/10.1007/s00198-022-06298-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06298-x