Abstract
Summary
In this study, we found that regional disparity in incidence of hip fractures has converged. Also, annual hip fracture risk ratios between genders have systematically diminished over time.
Introduction
Several studies have reported secular trends in hip fracture incidence, but knowledge about the possible causes is limited. We studied potential explanations by examining spatio-temporal epidemiology of the fractures and estimating relative risks between genders.
Methods
This observational study was based on all inpatient hospital discharges in 1972–2018 in Finland. We divided the data by gender, 5-year age groups and Finnish sub-regions and estimated gender and age standardized spatio-temporal rates of hip fractures by using a Bayesian age-period-cohort model.
Results
In 1972, women’s hip fracture incidence was 1.2–1.3 times higher in western and coastal Finland compared to eastern and inland areas. Also, women had approximately 1.7 times higher average risk to get a hip fracture compared to men. Today, the hip fracture differences between the areas have converged to insignificant and the relative risk between genders has diminished to 1.2. Age-specific relative risks indicate greater hip fracture risk for younger men and older women, and the women’s risk increases beyond the risk of men at age 65 which is ten years later than in the beginning of the study period.
Conclusion
Incidence of hip fracture has converged significantly between regions and genders. Especially factors related with socioeconomic development and increased frailty and longevity seem to be important. The hip fracture incidence rate ratio between women and men has systematically decreased in time, and more attention should be paid to hip fracture risk in men in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are a major public health problem worldwide and an important cause of mortality and disability in elderly people [1]. However, the variability in incidence of hip fracture among populations is considerable and the incidence also differs significantly between genders as women are more likely to experience hip fracture [2]. Notably, in recent times the incidence has been declining in many western countries such as in Finland and other Nordic countries [3, 4].
The Scandinavian countries have the highest incidence of hip fractures in the world and the age-standardized rate is greater than 200-fold compared to some African countries [3]. The incidence does not vary only between countries but also within countries [5,6,7,8,9,10]. For instance, Norway has reported different trends in different regions which highlights that there is a possibility of regional differences in secular trends within the same country [11].
The hip fracture incidence in men is approximately half that noted in women within countries [2]. Overall, men seem to have more fractures than women before the age of 50 years [12]. After menopause, women begin to lose bone density, which exposes them to a higher risk of fracture [13]. In particular, efforts have been made to prevent hip fractures in women, but men’s osteoporosis (a disease characterized by low bone mass) has been reported to be underdiagnosed and undertreated [14,15,16].
Considering these previously discussed factors, we studied long-term trends regionally and between genders in Finland. As the differences in hip fracture incidences worldwide are regional variations, the possible variations in spatio-temporal incidences within a country are likely to reveal explanations and add understanding to the incidence, epidemiology and risk factors of hip fractures in the worldwide level. Also, nationwide region and gender-specific analyses give important data on the incidence and trends of hip fractures, which help to plan public health strategies to prevent fractures.
Material and methods
This research was based on the Care Register for Health Care [17, 18]. It is a Finnish nationwide database containing data of all inpatient hospital discharges since 1969 and it is maintained by Finnish Institute for Health and Welfare.
Inclusion and exclusion criteria
The inclusion criteria for our research were hip fracture treatment periods in which primary or secondary diagnosis is a hip fracture (Finnish version of ICD-8 [used during 1969–1986]: 82000, 82001, 82002, 82003, 82010, 82011, 82012 and 82013; ICD-9 [1987–1995]: 8200A, 8201A, 8202A, 8203A, 8203B and 8203C; and ICD-10 [1996–2018]: S720, S721, S722). By using personal identity codes, we extracted data from all periods spent in hospitals from 1969 to 2018, from every included patient. Because the interest of this study was to focus on (first) age-related hip fractures, we finally included only patients of 50 years or older since 1972 in our analyses.
Definition of the significance of the first age-related hip fracture
In this study, we are interested in patients’ first age-related (low energetic) hip fracture. It is well known that a previous fracture predisposes to a new one [19]. One-third of female hip fracture patients have had at least one fragility fracture prior to hip fracture [20, 21], among men every fifth [21]. As the first hip fracture predisposes to the next one, it must be well understood and prevented.
Pathophysiology of hip fracture has led to a view of frailty syndrome behind the hip fracture. It refers to an age-related decline in several physiological systems which predisposes to an osteoporotic fracture such as hip fracture [22]. It is mainly caused by complex aging mechanisms that are determined by underlying genetic, epigenetic, health behaviour and environmental factors. Thus, the event of the first age-related hip fracture can be seen as an indicator of the moment in time when the risk factors associated with aging have exceeded a critical threshold and can lead to a fracture even with low-energy trauma [23]. Therefore, the first hip fracture defines the upper limit for the time of the development for critical hip fracture risk factors, and in that view, it is significant and the most interesting.
Definition of clearance period
Problems with a straightforward use of register data have been demonstrated as the use of calendar year boundaries that causes erroneously counted estimates. This is because patients having their fracture during the final months of each year are counted as separate cases for two years and on the other hand the patient may have several fractures during the same year. Also, a problem with linked register data is to define the difference between admissions due to fresh hip fractures and hospitalizations due to ongoing treatment episodes or reoperations [23].
To avoid these biased estimates, and because we are interested in the patients’ first aging-related hip fracture, we have used a hip fracture free clearance period to sort out new admissions from readmissions. A previous study has demonstrated that seven to ten years are needed until the risk of a new hip fracture has reduced to the same level as that without a preceding hip fracture [23], so a conservative ten-year clearance period was selected in this study and e.g. patients aged 50 at the event of hip fracture were followed back until age 40. The same ten-year clearance criterion has been used in Denmark before [24]. Because we had data only back to 1969, the clearance period used during the 1970s was shorter, but at least three years.
Analysis
We used official population data from Statistics Finland to obtain the population figures for each sub-region (a region consisting of 1–17 municipalities (average 4.4) which together form a commuting region [25]) and year, separately for men, women and 5-year age groups. Group-specific hip fracture incidences were counted by dividing the number of incident fractures by risk population’s follow-up person-years which were approximated using midyear populations. The standardized incidence rates were calculated by using direct standardization with gender and 5-year age group stratification and the average population (aged 50+) in Finland from 1972 to 2018 as a standard population.
Because of the small amount of cases in the sub-regions, we used a similar Bayesian spatio-temporal age-period-cohort model as introduced by Papoila et al. [26] with minor modifications (different number of age groups, periods and regions) for estimating the spatio-temporal rates. In short, Yijgr denote the number of hip fractures for age group i = 1, …, 10, period j = 1, …, 47, gender g = 1, 2 and region r = 1, …, 70, and nijgr stands for the associated population counts. We assumed that incidence counts with rates nijgrλijgr follow a Poisson distribution. The linear predictor of the model can then be written as ηijgr = log(λijgr) = μg + θig + ϕjg + ψk + ur + νr + δjr, where μg is a gender-specific intercept, θig and ϕjg denote gender-specific age and period effects, ψk represents joint cohort effects with k being the appropriate cohort index for used age group and period intervals, u and v are spatially structured and unstructured random effects, and δ is included to consider space–time interactions. To take into account potentially similar incidence rates in nearby regions we modeled u with an intrinsic Gaussian Markov random field that utilizes a neighborhood matrix that defines adjacent regions. For a Bayesian hierarchical model, we defined the prior and hyperprior distributions as well as linear constraints required for the model following the suggested specifications [26]. We estimated several models to make sure that our choices provided consistent estimates. Estimation was done in R with INLA package following partly the R scripts published as supporting information by Papoila et al. [26].
Results
Annual numbers of the first aging-related hip fractures between 1972 and 2018 in Finland by age group and gender are reported in Supplementary Table 1. The numbers have tripled from about 2000 in early 1970s to over 6000 during the latest five years. The proportion of hip fractures among people aged 85+ has increased from 14% in 1972 to 42% in 2018 (among people aged 50+). That means about 8 times more hip fractures among women aged 85+ and over 13 times more among men aged 85+ in 2018 (vs. 1972).
Regional incidence of hip fractures
Fig. 1 presents the regional standardized incidence rates of hip fractures by age, cohort and time period in Finland. The rates are presented for every second year from 1972 to 2018 and scaled so that the overall mean rate corresponds to one. The regional differences are systematic in the country as the highest hip fracture incidences are located mainly in western Finland, closer to Scandinavian countries. As seen also from the figure, the increasing hip fracture trend broke in late-1990s and started to decline in the whole country. The secular trends do not differ significantly between sub-regions in Finland.
Sub-regional hip fracture incidence rates standardized by age, cohort, and time period in Finland in every second year from 1972 to 2018 and scaled so that the overall mean rate corresponds to one. Finland is located in northern Europe, and borders with Scandinavian countries of Sweden and Norway in the west and Russia in the east. Baltic Sea surrounds Finland to the southwest
In Fig. 2, the high-frequency hip fracture region in the west, which is shown in Fig. 1, is compared with the lower-frequency region in the east, in both genders. The coastal area has been studied separately, even though it partly overlaps with western area, as the coast is largely Swedish-speaking and known to be a substantial Scandinavian gene flow area, making it different from the rest of the country.
Comparisons of regional hip fracture age-standardized incidence rates for 100,000 person years in men and women in Finland in 1972–2018. The shaded areas represent the 95% confidence intervals. The geographic divide to east/west and coast/inland are not mutually exclusive geographic regions but reflect two methods for partitioning the country. Subfigures (a) and (c) represent the gender-specific differences between eastern and western parts of the country, (b) and (d) between coastal and inland areas
Fig. 2a and 2b represents differences in hip fracture incidence in women. At the beginning of the study period, the hip fracture incidence was 1.3 times higher in the west than in the east and 1.2 times higher near the coast than inland. The differences have reduced between these areas as the increase has been first greater in inland and eastern areas, and after trend break, the decrease greater in western and coastal areas. There is no significant difference in the fracture incidence between these regions today.
Fig. 2c and 2d represents differences in hip fracture incidence in men. Men were 1.1 times in greater risk of hip fracture in west than in east Finland in 1972 but the risk has reduced being indifferent. There has not been significant difference in risk of hip fracture between men in coast and inland, only during the trend break men in coast were 1.1 times in higher risk of fracture than men in inland.
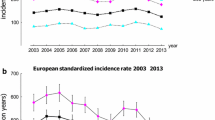
Risk of hip fracture between women and men
In Fig. 3, the hip fracture incidence rates are presented in women and men, and the relative risk of hip fracture is estimated between genders in Finland. As seen in Fig. 3a, the hip fracture incidence was higher in women than in men throughout the whole study period. The increasing trend broke in the late-1990s, first in women and a couple of years later in men. Also, the relative risk of experiencing a hip fracture in women compared to men has significantly changed during the observation period. In 1972, women had approximately 1.7 times higher average risk of experiencing a hip fracture when compared to men, whereas in 2018, the relative risk between genders was 1.2.
Fig. 3b shows the relative risks of hip fracture by age group between women and men. The relative risk is greater for men than for women in the youngest age groups, however it increases rapidly for women up to the age of 80–85 and begins to narrow again between the genders in the oldest age groups. The shape of the age-specific risk graph has remained similar throughout the period of the study, but the graph has shifted downwards reflecting the diminishing relative risk between women and men. During the years of 1972–1981 the risk of hip fracture for women increased beyond the risk of men after the age of 55, whereas in 2009–2018, the risk of women exceeded the risk of men only after the age of 65. The greatest age group specific relative risk (ages 75–85) has dropped from approximately 1.9 to less than 1.5 from 1972–1981 to 2009–2018.
Discussion
In this nationwide observational study of hip fracture patients, we found that the incidence of hip fracture has varied widely between regions in Finland in the past, but the differences have become smaller. The differences have been larger among women than men and the highest incidence has been in the coastal area, extending from southern Finland to the west.
The difference in hip fracture incidence has not only been reduced between the regions but also between genders’ age-adjusted incidence rates. In recent years, the annual relative hip fracture risk between genders has been 1.2. The shape of the age-specific risk graph has remained similar during the study period indicating a relatively greater risk of hip fracture for younger men and older women in the population. However, it is noteworthy that the age at which women’s average risk increases above men’s risk has been delayed by nearly ten years.
Regional differences
Our finding of the regional differences in the incidence of hip fractures is in line with several previous studies reporting intra-country differences [5,6,7,8,9,10]. The possible underlying causes for hip fracture are basically divided into genetic and non-genetic factors (including lifestyle and environmental factors).
Differences in the incidence of hip fractures have been observed between different ethnic groups and this has supported the notion of a possible genetic susceptibility to hip fracture [3]. The Finnish population has been found to be divided regionally in the east–west direction in terms of gene variation and morbidity. The west Finland is largely Swedish-speaking and known to be a substantial Scandinavian gene flow area [27,28,29]. Also, as Scandinavian countries have the highest incidence of hip fractures in the world, we considered genetic susceptibility as a possible factor in the regional differences.
As seen in Fig. 1, there is a divergence between east and west Finland in terms of hip fracture incidence. The division seems to follow fairly close to the approximate borderline of the treaty of Nöteborg (1323) which reflects the genetic population structure before internal migration events that have taken place since around 1950 [28]. This supports the hypothesis of genetic susceptibility to hip fracture. However, Finnish gene variations have been reported to be substantial especially in men-transmitted Y-chromosome [29], and conversely, the regional hip fracture differences in our study are moderate for men. Also, the hip fracture diversity in women has narrowed so rapidly that it seems unlikely to be explained by gene mixing due to migration. Considering these speculated factors, it seems unlikely that the regional disparity can be explained by gene flow.
Worldwide systematic reviews have also concluded that trends in hip fracture incidence suggest other than genetic background factors [2, 3]. High-income countries have higher age standardized hip fracture rates indicating that increased socioeconomic status, life expectancy and urbanization are correlated with hip fracture rates. The correlations tend to be more pronounced in women than in men [3]. Also, there has been a debate about the effect of latitude to hip fracture incidence due to lower vitamin D absorption at higher latitudes [2, 6, 7, 9].
In the past, Finland has been strongly divided between western farming culture and eastern hunting culture. Until the mid-1850s, living conditions in eastern and northern Finland were worse than in the rest of the country. The structural diversity has been leveling off, but the inequalities still persist [27]. However, mortality among middle-aged people decreased faster in the east and north Finland during the last century than elsewhere in Finland [30]. The consequences of the increase in life expectancy (and simultaneous qualitative change in population living long enough to get hip fractures, i.e. increased longevity and frailty) and socioeconomic status are likely to be reflected in our results, as the incidence of hip fractures increased more strongly in the east than in the west before the mid-1990s. The regional differences in our study do not seem to follow the latitudes, even though the latitude related conditions are clearly different in southern Finland than above the arctic circle in northern Finland, therefore the present study does not strengthen the latitude-related hip fracture risk theory.
The higher hip fracture rates in developed countries have been thought to be related in part to lifestyle [3]. A healthier and more active lifestyle is associated with a lower hip fracture incidence [31,32,33]. Lifestyle differences have been reported between the largest Finnish cities. In 2014, the use of vegetables among Helsinki residents was low for every fifth resident, and correspondingly for every third resident in Oulu. Smoking varied less among large Finnish cities as 11–16% of inhabitants smoked. Lack of physical activity during free time varied between 16 and 24% [34]. However, regional comprehensive long-term lifestyle trends are needed to draw further conclusion about the possible impact of lifestyle on regional hip fracture disparity.
In addition to the present study, Norway and Japan have reported converging regional incidences of hip fracture [7, 10]. The Japanese highlight reduced regional differences in levels of nutrient intake [10] and the Norwegians believe in more extensive structural changes, such as healthier older adults [7]. Previous Finnish studies have also speculated that a cohort effect toward healthier elderly populations could partly explain the hip fracture incidence development in Finland [4, 23].
In principle, also the migration from lower risk countries could have affected the lowering rates. However, the number of elderly immigrants in Finland is negligible (about 20,000 aged 65 or more in 2019, and clearly less earlier) and most of them are from the nearby areas of former Soviet Union, i.e. with similar environmental and genetic background as the other population. Therefore, it is not likely that migration would have any role in the current analysis, but in the future that might be an important factor to be considered.
Relative risk between genders
The incidence of hip fracture has changed dramatically in recent decades, and in our study, the condition typically suffered by women has become more and more a trouble of both genders. A similar relative risk reduction has recently been reported from Spain and Denmark, but these studies did not focus on the first aging-related hip fracture. In Spain women/men hip fracture risk ratio was reduced by half (to 2.40) and in Denmark by third (to 1.7–1.9 depending on the fracture site) over two decades [35, 36].
It is likely that the narrowed hip fracture risk is mostly a result of reduction in the risk of women as the decline in hip fracture incidence has been particularly clear among women [4]. The impact of life expectancy must also be taken into account as age-standardization cannot account for potential qualitative change in population risk caused by increase longevity and frailty. Compared to 1988, the life expectancy of Finns at the age of 65 has increased by 0.6 years more in men than in women [37]. In Denmark the increase in life expectancy, especially in men, has been faster than the change in age at hip fractures, which has resulted in the mean life expectancy exceeding the mean age at hip fracture, unlikely in the 1990s [36]. Similar phenomenon is likely explaining our results as longer lifetime increases critical late-life exposure time for experiencing a fracture.
Osteoporosis is an important risk factor for fragility fractures [1]. However, osteoporosis especially in men has remained underdiagnosed and undertreated [14,15,16]. Independent predictor for being investigated for osteoporosis is female gender [38] and women are more likely to receive intervention after an osteoporotic fracture than men [15, 39]. Less common prevention and early treatment of consequences of osteoporosis among men might reduce the relative hip fracture risk between genders. However, the prevention of hip fracture in men is hampered by the fact that men are less likely than women to experience a previous osteoporotic fracture before a hip fracture [21], which would present as an opportunity for hip fracture prevention. Despite the limit, men have a higher post fracture mortality rate than women [40], so their risk should be taken seriously.
There was no significant difference in secular trends in hip fracture between women and men in Finland during the study period. Also, regionally in east–west and coastal–inland areas, secular trends in genders have followed the same pattern. From this it can be assumed that possible population level factors, at least in these areas, do not differ significantly between men and women.
In our analysis, men appear to be reaching the similar hip fracture risk as women. Notably, as we have reported only annual hip fracture rates, longitudinal studies are needed to analyze whether the lifetime risk of experiencing a hip fracture has changed between genders.
Strengths and limitations
The strengths of this study include the use of data from national registers and databases characterized by a high data validity [18] and complete demographics of the background population. Also, the study provides detailed regional analyses revealing variations in gender, age and region-specific trends of hip fracture incidence in a novel way.
The primary limitation of our study is an observational study design that allows only indirect inferences meaning that the exact reasons to the secular changes will remain partly inconclusive and the register-based data gives limited information on confounders or other explanatory factors.
Conclusion
The regional disparity in hip fracture incidence has been evident in women, and moderate among men, but the differences have decreased. Changing risk ratios between genders put men at a relatively higher risk of hip fracture than before. The gender differences in age-adjusted incidence rates have diminished over time, and the women’s risk of fracture increases beyond the risk of men ten years later than in the beginning of the study period.
Data availability
Original individual level study data were from the Care Register for Health Care maintained by Finnish Institute for Health and Welfare. These confidential data are not publicly available and require research permissions that can be applied from the Health and Social Data Permit Authority FinData (findata.fi). Annual numbers of the first aging dependent hip fractures by age groups and gender are shown in Supplementary Table 1.
Code availability
The R codes used to generate the results can be obtained from the authors upon request.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256. https://doi.org/10.1007/s00198-012-1964-3
Cauley JA, Chalhoub D, Kassem AM, Fuleihan GE (2014) Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol 10:338–351. https://doi.org/10.1038/nrendo.2014.51
Kannus P, Niemi S, Parkkari J, Sievänen H (2018) Continuously declining incidence of hip fracture in Finland: analysis of nationwide database in 1970–2016. Arch Gerontol Geriatr 77:64–67. https://doi.org/10.1016/j.archger.2018.04.008
Barbier S, Ecochard R, Schott A et al (2009) Geographical variations in hip fracture risk for women: strong effects hidden in standardised ratios. Osteoporos Int 20:371–377. https://doi.org/10.1007/s00198-008-0687-y
Curtis EM, van der Velde R, Moon RJ, van den Bergh JPW, Geusens P, de Vries F, van Staa TP, Cooper C, Harvey NC (2016) Epidemiology of fractures in the United Kingdom 1988–2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone 87:19–26. https://doi.org/10.1016/j.bone.2016.03.006
Forsén L, Søgaard AJ, Holvik K, Meyer HE, Omsland TK, Stigum H, Dahl C (2020) Geographic variations in hip fracture incidence in a high-risk country stretching into the Arctic: a NOREPOS study. Osteoporos Int 31:1323–1331. https://doi.org/10.1007/s00198-020-05346-8
Héquette-Ruz R, Beuscart J, Ficheur G, Chazard E, Guillaume E, Paccou J, Puisieux F, Genin M (2020) Hip fractures and characteristics of living area: a fine-scale spatial analysis in France. Osteoporos Int 31:1353–1360. https://doi.org/10.1007/s00198-020-05363-7
Odén A, Kanis JA, McCloskey EV, Johansson H (2014) The effect of latitude on the risk and seasonal variation in hip fracture in Sweden. J Bone Miner Res 29:2217–2223. https://doi.org/10.1002/jbmr.2250
Orimo H, Yaegashi Y, Hosoi T, Fukushima Y, Onoda T, Hashimoto T, Sakata K (2016) Hip fracture incidence in Japan: estimates of new patients in 2012 and 25-year trends. Osteoporos Int 27:1777–1784. https://doi.org/10.1007/s00198-015-3464-8
Emaus N, Olsen LR, Ahmed LA, Balteskard L, Jacobsen BK, Magnus T, Ytterstad B (2011) Hip fractures in a city in Northern Norway over 15 years: time trends, seasonal variation and mortality. Osteoporos Int 22:2603–2610. https://doi.org/10.1007/s00198-010-1485-x
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697. https://doi.org/10.1016/j.injury.2006.04.130
Karlamangla A, Burnett-Bowie S, Crandall CJ (2018) Bone health during the menopause transition and beyond. Obstet Gynecol Clin N Am 45:695–708. https://doi.org/10.1016/j.ogc.2018.07.012
Papaioannou A, Kennedy C, Ioannidis G et al (2008) The osteoporosis care gap in men with fragility fractures: the Canadian Multicentre Osteoporosis Study. Osteoporos Int 19:581–587. https://doi.org/10.1007/s00198-007-0483-0
Adler RA (2014) Osteoporosis in men: a review. Bone Res 2:14001. https://doi.org/10.1038/boneres.2014.1
Bor A, Matuz M, Gyimesi N, Biczók Z, Soós D (2015) Gender inequalities in the treatment of osteoporosis. Maturitas 80:162–169. https://doi.org/10.1016/j.maturitas.2014.11.001
Finnish Institute for Health and Welfare. Care Register for Health Care. https://thl.fi/en/web/thlfi-en/statistics/information-on-statistics/register-descriptions/care-register-for-health-care
Sund R (2012) Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health 40:505–515. https://doi.org/10.1177/1403494812456637
Kanis JA, Johnell O, De Laet C, et.al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375-382 DOI https://doi.org/10.1016/j.bone.2004.03.024
Maggi S, Siviero P, Gonnelli S, Caffarelli C, Gandolini G, Cisari C, Rossini M, Iolascon G, Mauro G, Nuti R, Crepaldi G (2011) The burden of previous fractures in hip fracture patients. The break study. Aging Clin Exp Res 23:183–186. https://doi.org/10.1007/BF03324958
Frederiksen A, Abrahamsen B, Johansen PB, Sørensen HA (2018) Danish, national cross-sectional observational study on the prevalence of prior major osteoporotic fractures in adults presenting with hip fracture-limitations and scope for fracture liaison services in prevention of hip fracture. Osteoporos Int 29:109–114. https://doi.org/10.1007/s00198-017-4247-1
Gielen E, Verschueren SS, O’neill TW, Pye SR, O’connell MDL, Lee DM, Ravindrarajah RR, Claessens FF, Laurent MM, Milisen KK, Tournoy JJ, Dejaeger MM, Wu FC, Vanderschueren DD, Boonen SS (2012) Musculoskeletal frailty: a geriatric syndrome at the core of fracture occurrence in older age. Calcif Tissue Int 91:161–177. https://doi.org/10.1007/s00223-012-9622-5
Sund R (2007) Utilization of routinely collected administrative data in monitoring the incidence of aging dependent hip fracture. Epidemiol Perspect Innov 4:2. https://doi.org/10.1186/1742-5573-4-2
Giversen IM (2006) Time trends of age-adjusted incidence rates of first hip fractures: a register-based study among older people in Viborg County, Denmark, 1987–1997. Osteoporos Int 17:552–564. https://doi.org/10.1007/s00198-005-0012-y
Statistics Finland. Sub-regional units 2020. https://www.stat.fi/en/luokitukset/seutukunta/seutukunta_1_20200101/
Papoila AL, Riebler A, Amaral-Turkman A, São-João R, Ribeiro C, Geraldes C, Miranda A (2014) Stomach cancer incidence in Southern Portugal 1998–2006: a spatio-temporal analysis. Biom J 56:403–415. https://doi.org/10.1002/bimj.201200264
Karvonen JS, Rimpelä AH (1998) Diminishing regional contrasts? The east–west-divide in health behaviour among Finnish adolescents. Health Place 4:161–170. https://doi.org/10.1016/s1353-8292(98)00008-2
Kerminen S, Havulinna AS, Hellenthal G, Martin AR, Sarin A, Perola M, Palotie A, Salomaa V, Daly MJ, Ripatti S, Pirinen M (2017) Fine-scale genetic structure in Finland. G3 (Bethesda) 7:3459–3468. https://doi.org/10.1534/g3.117.300217
Palo JU, Ulmanen I, Lukka M, Ellonen P, Sajantila A (2009) Genetic markers and population history: Finland revisited. Eur J Hum Genet 17:1336–1346. https://doi.org/10.1038/ejhg.2009.53
Valkonen T, Martelin T, Rimpelä A (1990) Eriarvoisuus kuoleman edessä. In Tilastokeskuksen tutkimuksia 172 Helsinki: Hakapaino
Benetou V, Orfanos P, Feskanich D, Michaëlsson K, Pettersson-Kymmer U, Eriksson S, Grodstein F, Wolk A, Bellavia A, Ahmed LA, Boffeta P, Trichopoulou A (2016) Fruit and vegetable intake and hip fracture incidence in older men and women: the CHANCES Project. J Bone Miner Res 31:1743–1752. https://doi.org/10.1002/jbmr.2850
Lagerros Y, Hantikainen E, Michaëlsson K, Ye W, Adami H, Bellocco R (2017) Physical activity and the risk of hip fracture in the elderly: a prospective cohort study. Eur J Epidemiol 32:983–991. https://doi.org/10.1007/s10654-017-0312-5
Shen G, Li Y, Zhao G et al (2015) Cigarette smoking and risk of hip fracture in women: a meta-analysis of prospective cohort studies. Injury 46:1333–1340. https://doi.org/10.1016/j.injury.2015.04.008
Kaikkonen R, Murto J, Pentala O, et al. (2014) Terveys- ja hyvinvointierot erot suurissa kaupungeissa 2013. Terveyden ja hyvinvoinnin laitos
Mazzucchelli Esteban R, Pérez-Fernández E, Crespí-Villarías N, García-Vadillo A, Rodriguez-Caravaca G, Gil de Miguel A, Carmona L (2017) Trends in osteoporotic hip fracture epidemiology over a 17-year period in a Spanish population: Alcorcón 1999–2015. Arch Osteoporos 12:84. https://doi.org/10.1007/s11657-017-0376-6
Abrahamsen B, Laursen H, Skjødt M, Jensen M, Vestergaard P (2020) Age at hip fracture and life expectancy in Denmark—secular trends over two decades. Bone 130. https://doi.org/10.1016/j.bone.2019.115083
Statistics Finland (2019) Average life expectancy at birth was 78.9 years for boys and 84.3 years for girls in 2018. https://www.stat.fi/til/kuol/2018/01/kuol_2018_01_2019-10-24_tie_001_en.html
Bliuc D, Bliuc D, Ong C, Ong C, Eisman J, Eisman J, Center J, Center J (2005) Barriers to effective management of osteoporosis in moderate and minimal trauma fractures: a prospective study. Osteoporos Int 16:977–982. https://doi.org/10.1007/s00198-004-1788-x
Leslie W, Leslie W, Giangregorio L, Giangregorio L, Yogendran M, Yogendran M, Azimaee M, Azimaee M, Morin S, Morin S, Metge C, Metge C, Caetano P, Caetano P, Lix L, Lix L (2012) A population-based analysis of the post-fracture care gap 1996–2008: the situation is not improving. Osteoporos Int 23:1623–1629. https://doi.org/10.1007/s00198-011-1630-1
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital. This work was partly supported by the Finnish Cultural Foundation; Ester and Uuno Kokki fund and VTR (Regional State Funds) for project in 2018: Fractures in Finland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study formal consent is not required.
Conflict of interest
Salla-Riikka Pekonen, Juho Kopra, Heikki Kröger, Toni Rikkonen and Reijo Sund declare that they have no conflict of interest. There has been no significant financial support for this work that could have influenced this outcome.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Perspectives for regional hip fracture trends
Supplementary Information
ESM 1
(PDF 208 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pekonen, SR., Kopra, J., Kröger, H. et al. Regional and gender-specific analyses give new perspectives for secular trend in hip fracture incidence. Osteoporos Int 32, 1725–1733 (2021). https://doi.org/10.1007/s00198-021-05906-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-05906-6






