Abstract
Summary
We conducted a large, retrospective cohort study using data from Taiwan’s National Health Insurance Research Database to evaluate whether the risk of developing osteoporosis is associated with sepsis. Our study found that adults younger than 65 years with sepsis had a significantly increased risk of developing osteoporosis.
Introduction
There have been limited studies regarding the osteoporosis risk associated with sepsis. Our purpose is to evaluate whether the risk of developing osteoporosis is associated with sepsis.
Methods
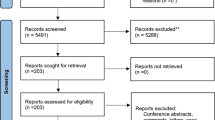
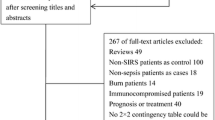
We conducted a large, retrospective cohort study using data from Taiwan’s National Health Insurance Research Database. From the insurance claims data, a total of 13,178 patients diagnosed with sepsis from 2000 to 2012 were included in the sepsis cohort, and a propensity score-matched cohort included 13,178 individuals without sepsis. To calculate the incidence of osteoporosis, both groups were followed until 2013. Cox regression analysis was performed to obtain the hazard ratios (HRs) to assess the risk of developing osteoporosis. The Kaplan–Meier method was used to estimate the cumulative incidence of osteoporosis.
Results
The overall incidences of osteoporosis (per 1,000 person-years) in the sepsis and non-sepsis groups were 10.2 and 10.7, respectively. The risk of osteoporosis significantly increased in the presence of sepsis (adjusted HR = 1.17, 95% confidence interval (CI) = 1.04–1.31). The risk of osteoporosis in the sepsis group was significantly higher than that in the non-sepsis group for young patients aged 20–49 years and patients aged 50–64 years (adjusted HR = 1.93, 95% CI = 1.08–3.44; adjusted HR = 2.01, 95% CI = 1.52–2.65, respectively). The Kaplan–Meier curves of cumulative probability also showed a significantly increased risk of osteoporosis in patients aged 20–49 years and aged 50–64 years with sepsis compared with non-sepsis (P = 0.025; P < 0.001, respectively).
Conclusion
Adults younger than 65 years with sepsis had a significantly increased risk of developing osteoporosis.



Similar content being viewed by others
References
Rachner TD, Khosla S, Hofbauer LC (2011) Osteoporosis. Now and the future. Lancet 377(9773):1276–1287
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28(5):1531–1542
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29(11):2520–2526
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R (2014) National Osteoporosis Foundation: Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Siris ES, Adler R, Bilezikian J, Bolognese M, Dawson-Hughes B, Favus MJ, Harris ST, Jan de Beur SM, Khosla S, Lane NE, Lindsay R, Nana AD, Orwoll ES, Saag K, Silverman S, Watts NB (2014) The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int 25(5):1439–1443
Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K (2016) International Forum of Acute Care Trialists. Assessment of global incidence and mortality of hospital-treated Sepsis. Current estimates and limitations. Am J Respir Crit Care Med 193(3):259–272
Angus DC, van der Poll T (2013) Severe sepsis and septic shock. N Engl J Med 369(9):840–851
Walkey AJ, Lagu T, Lişndenauer PK (2015) Trends in infection and sepsis sources in the United States. A population-based study. Ann Am Thorac Soc 12(2):216–220
Chen YJ, Chen FL, Chen JH, Wu MM, Chen YL, Chien DS, Ko Y (2019) Epidemiology of sepsis in Taiwan. Medicine (Baltimore) 98(20):e15725
Lee P, Nair P, Eisman JA, Center JR (2016) Bone failure in critical illness. Crit Care Med 44(12):2270–2274
Smith LM, Cuthbertson B, Harvie J, Webster N, Robins S, Ralston SH (2002) Increased bone resorption in the critically ill: association with sepsis and increased nitric oxide production. Crit Care Med 30(4):837–840
Orford N, Cattigan C, Brennan SL, Kotowicz M, Pasco J, Cooper DJ (2014) The association between critical illness and changes in bone turnover in adults: a systematic review. Osteoporos Int 25(10):2335–2346
Orford NR, Bailey M, Bellomo R, Pasco JA, Cattigan C, Elderkin T, Brennan-Olsen SL, Cooper DJ, Kotowicz MA (2017) The association of time and medications with changes in bone mineral density in the 2 years after critical illness. Crit Care 21(1):69
Van den Berghe G, Van Roosbroeck D, Vanhove P, Wouters PJ, De Pourcq L, Bouillon R (2003) Bone turnover in prolonged critical illness: effect of vitamin D. J Clin Endocrinol Metab 88(10):4623–4632
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D (2006) Sepsis occurrence in acutely ill patients investigators. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34(2):344–353
Hongo T, Kotake K, Muramatsu H, Omura D, Yano Y, Hasegawa D, Momoki N, Takahashi K, Nozaki S, Fujiwara T (2019) Loss of bone mineral density following sepsis using Hounsfield units by computed tomography. Acute Med Surg 6(2):173–179
Puthucheary ZA, Sun Y, Zeng K, Vu LH, Zhang ZW, Lim RZL, Chew NSY, Cove ME (2017) Sepsis reduces bone strength before morphologic changes are identifiable. Crit Care Med 45(12):e1254–e1261
National Health Research Institutes. National Health Insurance Research Database. https://nhird.nhri.org.tw/en/index.html Accessed on July 5, 2020
Hsieh C-Y, Su C-C, Shao S-C, Sung S-F, Lin S-J, Yang Y-HK, Lai EC-C (2019) Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol 11:349–358
Nishizawa Y, Ohta H, Miura M, Inaba M, Ichimura S, Shiraki M, Takada J, Chaki O, Hagino H, Fujiwara S, Fukunaga M, Miki T, Yoshimura N (2013) Guidelines for the use of bone metabolic markers in the diagnosis and treatment of osteoporosis (2012 edition). J Bone Miner Metab 31(1):1–15
Shapses SA, Weissman C, Seibel MJ, Chowdhury HA (1997) Urinary pyridinium cross-link excretion is increased in critically ill surgical patients. Crit Care Med 25(1):85–90
Chaudhry H, Zhou J, Zhong Y, Ali MM, McGuire F, Nagarkatti PS, Nagarkatti M (2013) Role of cytokines as a double-edged sword in sepsis. In Vivo 27(6):669–684
Lacativa PG, Farias ML (2010) Osteoporosis and inflammation. Arq Bras Endocrinol Metabol 54(2):123–132
Gowen M, MacDonald BR, Hughes DE, Skjodt H, Russell RG (1986) Immune cells and bone resorption. Adv Exp Med Biol 208:261–273
Grimm G, Vila G, Bieglmayer C, Riedl M, Luger A, Clodi M (2010) Changes in osteopontin and in biomarkers of bone turnover during human endotoxemia. Bone. 47(2):388–391
Denhardt DT, Noda M, O'Regan AW, Pavlin D, Berman JS (2001) Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodeling, and cell survival. J Clin Invest 107(9):1055–1061
Chang IC, Chiang TI, Yeh KT, Lee H, Cheng YW (2010) Increased serum osteopontin is a risk factor for osteoporosis in menopausal women. Osteoporos Int 21(8):1401–1409
Lips P, van Schoor NM (2011) The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab 25(4):585–591
de Haan K, Groeneveld AB, de Geus HR, Egal M, Struijs A (2014) Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: systematic review and meta-analysis. Crit Care 18(6):660
Upala S, Sanguankeo A, Permpalung N (2015) Significant association between vitamin D deficiency and sepsis: a systematic review and meta-analysis. BMC Anesthesiol 15:84
Amrein K, Schnedl C, Holl A, Riedl R, Christopher KB, Pachler C, Urbanic Purkart T, Waltensdorfer A, Münch A, Warnkross H, Stojakovic T, Bisping E, Toller W, Smolle KH, Berghold A, Pieber TR, Dobnig H (2014) Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU Randomized Clinical Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA 312(15):1520–1530
Terashima A, Okamoto K, Nakashima T, Akira S, Ikuta K, Takayanagi H (2016) Sepsis-induced osteoblast ablation causes immunodeficiency. Immunity. 44(6):1434–1443
Manolagas SC (2000) Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr Rev 21(2):115–137
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Lee, YF., Tsou, HK., Leong, PY. et al. Association of sepsis with risk for osteoporosis: a population-based cohort study. Osteoporos Int 32, 301–309 (2021). https://doi.org/10.1007/s00198-020-05599-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05599-3