Abstract
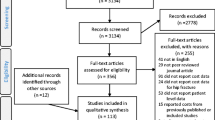
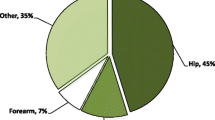
Fragility fractures (FF) are the main clinical consequence of osteoporosis. FF lead to a loss in quality of life (QL), increased dependency and higher costs due to loss of productivity. Despite this, very few studies have been performed about the indirect or social costs of FF. The objective of this review was to systematically synthesize published evidence regarding indirect costs of FF. We conducted a systematic literature review of empirical studies published as peer review papers between 1998 and 2019. A total of 295 papers were found about costs and osteoporosis. After an iterative process, only 16 papers fit the criteria of selection. Despite the important consequences for QL, only seven studies have included research of the issue and only one about dependency. Treatments are cost-effective, but adherence is low. Multiple fractures, older age and low socioeconomic profile imply higher costs. Most studies are performed using the human capital methodology. The main two variables are loss of productivity and absenteeism. Most of the people included in the samples are out of the active population. Those studies that include a follow-up period vary in a range between 3 months and 2 years. Depending on sample and methodology, the indirect costs (IC) are between 2 and 50%. The direct costs associated with FF generally far outweigh the IC. There is a lack of studies about the effects of treatments and adherence and about the dependency system. The changing role of women in coming generations will increase indirect costs.

Similar content being viewed by others
References
Consensus development conference (1993) Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94(6):646–650
Sozen T, Ozisik L, Calik Basaran N (2017) An overview and management of osteoporosis. Eur J Rheumatol 4(1):46–56
World Health Organization. Who Scientific Group on the Assessment of Osteoporosis At Primary Health. World Health. 2007;May(May 2004):1–13
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O’Malley CD (2014) Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos 9:182
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: Medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1–2)
World_Health_Organization. Guidelines for preclinical evaluation and clinical trials in osteoporosis. World Health Organization; 1998
Kanis JA (2002) Osteoporosis III: Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 359(9321):1929–1936
Kanis JA, Johnell O, Oden A, Borgstrom F, Johansson H, De Laet C, Jönsson B (2005) Intervention thresholds for osteoporosis in men and women: a study based on data from Sweden. Osteoporos Int 16(1):6–14
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, Muratore M, Casciaro S (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop 7(3):171–181
Abrahamsen B, Van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20(10):1633–1650
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15(10):767–778
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35(5):293–305
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28(5):1531–1542
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22(5):1277–1288
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Cummings SR, Melton LJ (2002) Epidemiology and consequences of osteoporotic fractures. Lancet. 359:1761–1767
Åkesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–2046
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M (2010) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15(4):721–739
Lindsay R, Cooper C, Hanley DA, Barton I, Broy SB, Flowers K (2001) Risk of new vertebral fracture. J Am Med Assoc 285(3):7–10
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28(3):775–780
Ray NF, Chan JK, Thamer M, Melton LJ (1997) Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res 12(1):24–35
Hoerger TJ, Downs KE, Lakshmanan MC, Lindrooth RC, Plouffe LEO Jr, Wendling B, West SL, Ohsfeldt RL (1999) Healthcare use among US women aged 45 and older: total costs and costs for selected postmenopausal health risks. J Womens Health Gend Based Med 8(8):1077–1089
Chrischilles E, Shireman T, Wallace R (1994) Costs and health effects of osteoporotic fractures. Bone. 15(4):377–386
Phillips S, Fox N, Jacobs J, Wright WE (1988) The direct medical costs of osteoporosis for American women aged 45 and older, 1986. Bone. 9(5):271–279
Johnell O (1997) The socioeconomic burden of fractures today and in the 21st century - the American journal of medicine. Am J Med 103(2):S20–S26
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22(3):465–475
Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jönsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU. Arch Osteoporos 6(1–2):59–155
Eekman DA, Ter Wee MM, Coupé VMH, Erisek-Demirtas S, Kramer MH, Lems WF (2014) Indirect costs account for half of the total costs of an osteoporotic fracture: a prospective evaluation. Osteoporos Int 25(1):195–204
Fujiwara S, Zhao X, Teoh C, Jaffe DH, Taguchi Y (2019) Disease burden of fractures among patients with osteoporosis in Japan: health-related quality of life, work productivity and activity impairment, healthcare resource utilization, and economic costs. J Bone Miner Metab 37(2):307–318
Borgström F, Sobocki P, Ström O, Jönsson B (2007) The societal burden of osteoporosis in Sweden. Bone. 40(6):1602–1609
Gisbert JP, Bonfill X. ¿Cómo realizar, evaluar y utilizar revisiones sistemáticas y metaanálisis? Gastroenterol Hepatol. 2004;27(3):129-149. https://doi.org/10.1016/S0210-5705(03)79110-9
Urrútia G, Bonfilll X (2013) La declaración prisma: Un paso adelante en la mejora de las publicaciones de la revista Española de salud pública. Rev Esp Salud Publica 87(2):99–102
Ng CS, Lau TC, Ko Y (2017) Cost of osteoporotic fractures in Singapore. Value Heal Reg Issues 12:27–35
Jürisson M, Pisarev H, Kanis J, Borgström F, Svedbom A, Kallikorm R, Lember M, Uusküla A (2016) Quality of life, resource use, and costs related to hip fracture in Estonia. Osteoporos Int 27(8):2555–2566. Available from: https://doi.org/10.1007/s00198-016-3544-4
Marques A, Lourenço, da Silva JAP (2015) The burden of osteoporotic hip fractures in Portugal: costs, health related quality of life and mortality. Osteoporos Int 26(11):2623–2630
Qu B, Ma Y, Yan M, Wu HH, Fan L, Liao DF, Pan XM, Hong Z (2014) The economic burden of fracture patients with osteoporosis in western China. Osteoporos Int 25(7):1853–1860
Bleibler F, Rapp K, Jaensch A, Becker C, König HH (2014) Expected lifetime numbers and costs of fractures in postmenopausal women with and without osteoporosis in Germany: a discrete event simulation model. BMC Health Serv Res 14(1):1–18
Bleibler F, Konnopka A, Benzinger P, Rapp K, König HH (2013) The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany - a demographic simulation model. Osteoporos Int 24(3):835–847
Bayray A, Enquselassie F, Gebreegziabher Z. Costs of osteoporosis related fractures in hospital admitted patients, Tigrai, Northern Ethiopia: a retrospective study. Ethiop Med J. 2013;51(3):177-186. http://www.ncbi.nlm.nih.gov/pubmed/24669674. Accessed 29 Jan 2020
Tarride JE, Hopkins RB, Leslie WD, Morin S, Adachi JD, Papaioannou A, Bessette L, Brown JP, Goeree R (2012) The burden of illness of osteoporosis in Canada. Osteoporos Int 23(11):2591–2600
Dimai HP, Redlich K, Peretz M, Borgström F, Siebert U, Mahlich J. Economic burden of osteoporotic fractures in Austria. Health Econ Rev. 2012;2(1):12. https://doi.org/10.1186/2191-1991-2-12
Dimai HP, Redlich K, Schneider H, Siebert U, Viernstein H, Mahlich J (2012) Direct and indirect costs of fractures due to osteoporosis in Austria. Gesundheitswesen. 74(10):90–98
Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET (2010) Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. Pharmacoeconomics. 28(5):395–409
Konnopka A, Jerusel N, König HH (2009) The health and economic consequences of osteopenia- and osteoporosis-attributable hip fractures in Germany: estimation for 2002 and projection until 2050. Osteoporos Int 20(7):1117–1129
Ström O, Borgström F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Ceder L, Thorngren KG, Sernbo I, Jönsson B (2008) Long-term cost and effect on quality of life of osteoporosis-related fractures in Sweden. Acta Orthop 79(2):269–280
Dzajkovska B, Wertheimer AI, Mrhar A (2007) The burden-of-illness study on osteoporosis in the Slovenian female population. Pharm World Sci 29(4):404–411
Borgström F, Sobocki P, Ström O, Jönsson B. The societal burden of osteoporosis in Sweden. Bone. 2007;40(6):1602-1609. https://doi.org/10.1016/j.bone.2007.02.027
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(S02):S3-S7. https://doi.org/10.1007/s00198-004-1702-6
Fox C, Edwards MH, Dennison EM, Cooper C (2015) Personal and societal burden of osteoporotic fractures. Clin Rev Bone Miner Metab 13(2):53–60
Boonen S, Singer AJ (2008) Osteoporosis management: impact of fracture type on cost and quality of life in patients at risk for fracture I. Curr Med Res Opin 24(6):1781–1788
Acknowledgements
The authors wish to thank UCB Pharma, the Research Group SEJ-393: Public Economy and Globalization at the University of Granada, and the Dept. of Applied Economics for their support. We also thank Kate Burton for helping us with the English grammar.
Funding
This study was funded by UCB Pharma.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Manuel Ruiz-Adame and Manuel Correa declare that they have no conflict of interest.
Ethical approval
No specific approval was required for this bibliographic research study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruiz-Adame, M., Correa, M. A systematic review of the indirect and social costs studies in fragility fractures. Osteoporos Int 31, 1205–1216 (2020). https://doi.org/10.1007/s00198-020-05319-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05319-x