Abstract
Summary
This study identified the costs and health-related quality of life impacts of several post-fracture multidisciplinary care pathways specific to individual skeletal site (hip, distal forearm, vertebrae, humerus). These care pathways may assist healthcare providers in allocating resources for osteoporotic fractures in more effective and cost-efficient ways.
Introduction
This micro-costing study was undertaken to provide the estimated healthcare costs of several fracture site-specific health service use pathways associated with different trajectories of health-related quality of life (HRQoL) 12-months post-fracture.
Methods
The study included 4126 adults aged ≥ 50 years with a fragility fracture (1657 hip, 681 vertebrae, 1354 distal forearm, 434 humerus) from the International Costs & Utilities Related to Osteoporotic fractures Study (ICUROS). ICUROS participants were asked to recall the frequency and duration (where applicable) of their health and community care service use at 4- and 12-month follow-up visits. Patient-level costs were identified and aggregated to determine the average cost of healthcare use related to the fracture in each care pathway (presented in Australian 2021 dollars). Mean cost differences were calculated and analysed using a one-way analysis of variance (ANOVA) and post hoc Bonferroni correction to determine any statistically significant differences.
Results
The total direct cost of fractures was estimated at $89564, $38926, $18333, and $38461AUD per patient for hip, vertebral, wrist, and humeral participants, respectively. A Kruskal–Wallis test yielded a statistically significant difference in cost values between most care pathways (p < 0.001). Of the 20 care pathways, those associated with recovery of HRQoL had lower mean costs per patient across each fracture site.
Conclusions
This study identified the costs and HRQoL impacts of several multidisciplinary care pathways for individual fracture sites based on the health service utilization of an international cohort of older adults. These care pathways may assist healthcare providers in allocating resources for fragility fractures in more effective and cost-efficient ways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is an increasingly prevalent condition representing one of the greatest global health risks for individuals 50 years of age or older. Given the exponential increase in ageing populations, it is estimated that 500 million people worldwide will have osteoporosis by 2025, resulting in approximately 13.5 million fractures annually [1]. The significant health consequences of osteoporosis lie in the associated fragility fractures, which can be a life-changing event. Fragility fractures impact on quality of life and ability to undertake basic activities of daily living [2, 3], and increase the risk of early mortality for at least 5 years [4, 5]. In addition to their physical and mental impacts, fragility fractures also carry a significant economic burden for the healthcare system and the individuals themselves [6,7,8].
The cost of providing fracture care is substantial. The total annual expense for all osteoporosis-related fractures in the USA was approximately $57 billion (USD) in 2018, with an estimated increase to over $95 billion (USD) by 2040 [6]. Similarly, osteoporosis and the 4.3 million fragility fractures that it causes annually across Europe costs the healthcare system in excess of €56 billion each year based on data from 2019 [9]. Australia has one of the highest rates of bone disorders in the world, with direct costs associated with osteoporosis of $3.4 billion (AUD) in 2017, and a projected increase to $3.8 billion (AUD) by 2022 [7]. Fragility fractures incur short- and long-term costs, which differ between fracture sites. More severe fractures, such as fractures of the hip and vertebral, are most costly due to the need for more healthcare service (e.g. hospitalization, surgical procedures, rehabilitation) [7, 8]. Although hip and vertebral fractures are the most costly fracture types [8, 10], the higher incidence of non-hip-non-vertebral fractures contributes to a large proportion of total fracture-related costs [7, 8].
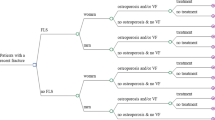
Fragility fractures most commonly occur at the hip, distal forearm (wrist), vertebrae, and humerus — collectively referred to as major osteoporotic fractures (MOFs). We recently identified several fracture site-specific health service use pathways (hereafter referred to as ‘care pathways’) using data from over 4,000 older men and women participating in the International Costs and Utilities Related to Osteoporotic fractures Study (ICUROS) [11]. Further analysis showed these care pathways were associated with different trajectories of HRQoL recovery at 12 months post-fracture [11]. However, it remains uncertain whether a greater recovery of HRQoL was achieved at an increased cost. The present micro-costing study was undertaken to determine whether the care pathways associated with greater HRQoL recovery are also cost-efficient.
Materials and methods
There were three major components to this study: (1) identifying distinct care pathways for individual fracture sites and analysing associations with recovery of HRQoL; (2) estimating the mean cost per patient in each care pathway; and (3) determining any statistically significant cost differences between the post-fracture care pathways.
ICUROS study design
ICUROS was an observational study that aimed to determine the HRQoL impact and cost consequences of fragility fractures in over 6000 older adults (≥ 50 years) across 11 countries — Australia, Austria, Estonia, France, Italy, Lithuania, Mexico, Russia, Spain, the UK, and the USA. The EuroQoL questionnaire (EQ-5D-3L) was used to assess HRQoL in all participants at baseline (including recall of HRQoL 4 weeks prior to the fracture), and prospectively at 4, 12, and 18 months post-fracture (there was a 2-week window for follow-up at each timepoint). ICUROS participants were also questioned about the use of health and community care services related to the study fracture via telephone interviews. Each participant was asked to recall the frequency and duration (where applicable) of their healthcare use at 4, 12, and 18 months. Where possible, healthcare use was verified via review of patient medical records. A detailed description of the ICUROS study design can be found elsewhere [12, 13].
Identification of care pathways
Twenty fracture site-specific care pathways (also referred to as ‘classes’) were identified in a previous study [11] using multi-level latent class analyses. A description of the methods has been published elsewhere [11, 14]. In brief, latent class analysis — a statistical method used to categorize participants within a study based on specific indicator variables [15] — was used to identify subgroups of participants with common patterns of health service use over the 12 months post-fracture. To determine the optimal model fit — i.e. the number of classes included in the final model — a one-class model was developed and subsequently increased in a stepwise fashion until a model with the lowest Bayesian Information Criterion, a significant Lo-Mendell-Rubin likelihood test, and the highest entropy value was found [15]. Once classes were identified, multivariable logistic regression was applied to analyse the associations of each class with recovery of HRQoL. Table 1 summarizes the classes identified for each fracture site and their associations with HRQoL recovery.
Costs of healthcare services
All costing methods were guided by a previous costing study [16]. Health service use data comprised of direct and non-direct healthcare services that were related to the study facture only, and were categorized into in-hospital care, outpatient care, supported living (e.g. residential aged care), community care services, pharmaceutical use, and diagnostic imaging. Patient-level costs were identified and aggregated to determine the average cost of healthcare use related to the fracture in each class. A societal perspective was taken with direct costs of fracture and osteoporosis management included, as well as informal care. Although the ICUROS is a multinational study including participants from 11 countries, all costs were retrieved from the Australian healthcare system and therefore presented in Australian dollars (AUD). Where costs were reported in earlier years, these were inflated to 2021 costs using the Australian consumer price index [17]. An itemized table of the unit cost of each healthcare service and the sources of costing information is presented in Supplementary File 1.
In-hospital care
Data pertaining to in-hospital care included non-admitted hospital services (e.g. emergency department (ED) presentations), hospital admissions including specialty care (geriatrics and orthopaedics), nursing care, and subacute care (i.e. inpatient rehabilitation). Costs attributed to ED presentations were taken from the Australian Independent Hospital Pricing Authority (IHPA) [18]. Hip fractures were assumed to be Triage Category 3 (injury), vertebral and humeral fractures Triage Category 4 (injury), and distal forearm fractures Triage Category 5 (injury). Hospital costs were assumed to vary by fracture type; therefore, costs for hospital admissions were calculated for each fracture site. An average cost per day in hospital was calculated by dividing the average cost per separation by the average length of stay in hospital for patients admitted under specific Australian Refined Diagnosis Related Groups (AR-DRGs) from the Australian IHPA [18]. This was then multiplied by the length of stay recorded by each ICUROS participant. Decisions about which AR-DRG codes to use were made through discussion with geriatricians and orthopaedic surgeons. Supplementary File 1 includes a list of AR-DRGs codes used to calculate hospital costs for each individual fracture.
Outpatient care
Outpatient care was defined as fracture management that occurred in the outpatient setting rather than in the hospital setting (either admitted or non-admitted) and included outpatient clinic visits, fracture/falls clinic appointments, rehabilitation day centre visits, allied healthcare (e.g. occupational therapy, physiotherapy), and primary care centre/general practitioner visits. Costs for outpatient care were sourced from the Australian IHPA [18] and the Medicare Benefits Schedule (MBS) [19]. An assumption for allied healthcare was made that participants attended a private clinic for these visits, not a hospital or outpatient clinic. Details of calculations can be found in Supplementary File 1.
Supported living
The daily cost for residing in a residential aged care (RAC) facility was calculated by averaging the cost of a resident bed day of a small-sized facility and a larger-sized facility in Australia during 2021 [20]. Data regarding days living within an RAC facility were collected using 4 weeks recall at each follow-up point. As the total number of days in a RAC facility during the 12 months follow-up was unattainable from ICUROS data, an assumption was made that once a participant was admitted to a RAC facility, they would remain there for the remainder of the 12-month follow-up period. It was also assumed that admission to a RAC facility occurred steadily throughout the year; therefore, the average length of stay in RAC was assumed to be 6 months [16].
Community care
Fracture-related use of community care services encompassed home visits by a health professional, phone counselling sessions, home and equipment modifications, and both professional and informal home help services. Costs of phone counselling was calculated by averaging the cost of nurse counsels and other health professional counsels [19]. The number of hours of professional home help was collected using recall of the previous 4 weeks at each follow-up point, and then extrapolated over the respective 12-month follow-up period and costed using the standard mid-level hourly rate of home care workers [21]. The same hourly rate was used for volunteer home help (e.g. help from family and friends), assuming that the participant would have required paid community services if care by a family member was not possible. The cost of home and equipment modifications undertaken by participants was collected as part of the ICUROS study and inflated to 2021 AUD using the Australian consumer price index [17].
Pharmaceutical use
Pharmaceutical use considered relevant for treatment of MOFs included (i) medications to manage osteoporosis (bisphosphonates, teriparatide, denosumab, oestrogen receptor modulators, strontium ranelate); (ii) calcium and vitamin D supplements (separately, and in combination); (iii) pain-relieving analgesics (opioids and non-opioids); and (iv) anti-depressant/anti-anxiety medications. It was assumed that people who reported taking osteoporosis-related medications at the first follow-up (4 months) were likely to use the recommended/scheduled dose over the 12-month study period. The cost of each osteoporosis-related medication was sourced from the Pharmaceutical Benefits Scheme (PBS) [22] and cost per year was calculated based on reported dosage. An average cost per year was then calculated for the four medication categories. This method was also employed to calculate the total cost of anti-depressant/anti-anxiety medication use. Etidronate and strontium ranelate are no longer available through the PBS and therefore could not be costed in this analysis. It was assumed that people who reported taking vitamin D and/or calcium supplements used the recommended daily dose for 12 months. The costs of supplements for different brands from Pharmacy Online Australia [23] were averaged. Use of opioid and non-opioid analgesics was assumed to be taken as needed, and therefore only costed for a maximum of 14 days [16]. Supplementary File 1 includes a list of all medications included in our study with the relevant PBS codes used, the schedule fee of each medication, and the cost calculations.
Diagnostic imaging
Diagnostic imaging data included routine medical imaging procedures (X-ray, computerized tomography [CT] scan, magnetic resonance imaging [MRI]) and relevant diagnostic imaging procedures for osteoporosis diagnosis (dual-energy X-ray absorptiometry [DXA]).
Cost analyses
To determine the mean cost per participant in each class, healthcare use rates were multiplied by the determined cost, and then divided by the number of participants in the class [24]. Mean cost differences were calculated and analysed using a one-way analysis of variance (ANOVA) and post hoc Bonferroni correction to determine any statistically significant differences (p-value < 0.05). All analyses were performed using STATA (version 16) software.
Results
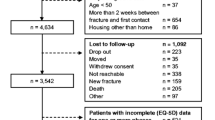
Of the 5650 participants potentially eligible for these analyses, 1524 participants were excluded due to loss to follow-up (n = 486), withdrawal from the study (n = 351), sustaining a new fracture during follow-up (n = 192), death (n = 246), or other reasons (n = 249), leaving a total of 4126 participants in this analysis (1657 hip, 1354 distal forearm, 681 vertebral, and 434 humeral fractures). The mean age of the total population was 71.5 ± 10.9 years, and the sample was predominately female (n = 3446; 83.5%). These variables differed between MOF sites: participants with a hip fracture were the oldest (76.6 ± 10.1) and distal forearm participants the youngest (67.1 ± 10.1), whereas the proportion of females was highest in distal forearm fracture participants (89.9%) and lowest in hip fracture participants (79.7%). Hip fracture participants had lower educational attainment and lower income levels compared to other MOF participants. Participant demographic characteristics are presented in Supplementary File 2 by class. Mean and median use of all healthcare services are presented in Supplementary File 3.
Hip fracture
The total direct cost per hip fracture patient was estimated to be $89,564AUD ($62,327USD; €46,029). In-hospital care contributed to the majority of total costs in patients (48.5%), followed by community care (40.9%) and residential aged care (8.1%). Mean costs per patient were the highest in class 3 and lowest in class 7 (Table 2). A Kruskal–Wallis test yielded a statistically significant difference in cost values between classes (H = 183.5, p < 0.001). The mean cost per patient in class 6 (the class which was associated with improved HRQoL recovery) was significantly lower than all other classes apart from classes 2, 5, and 7. Similarly, mean cost differences for class 7 (also associated with improved HRQoL recovery) were significantly lower than all other classes apart from classes 2 and 6.
Distal forearm fracture
The total mean cost of distal forearm fractures was $18,333AUD ($12,758USD; €9,422) per patient. Community care contributed to the majority of total costs in patients (51.9%), followed by in-hospital care (31.7%) and outpatient care (10.7%). The mean cost per patient varied by class and was highest for class 1 and the lowest for class 5 (Table 3). A Kruskal–Wallis test yielded statistically significant differences in cost values between each class (H = 618.4, p < 0.001). Class 3 was associated with improved HRQoL recovery and the mean cost per patient in class 3 was significantly lower than all other classes except for class 2 and class 5. Similarly, mean cost differences for class 5 were significantly lower than all classes apart from classes 2 and 3.
Vertebral fracture
The total direct cost of vertebral fractures was estimated to be $38,926AUD ($27,088USD; €20,005) per patient. In-hospital care contributed to the majority of total costs (48.1%), followed by community care (41.9%) and residential aged care (4.7%). Mean costs for vertebral fracture participants were the highest in class 2 and lowest in class 4 (Table 4). A Kruskal–Wallis test yielded a statistically significant difference in cost values between classes (H = 240.2, p < 0.001). The mean costs per patient were significantly lower for class 4 compared to all other classes. Conversely, mean cost differences for class 2, which was associated with decreased odds of HRQoL recovery, were significantly higher than all other classes apart from class 3.
Humeral fracture
The mean cost of humeral fractures was estimated to be $38,461AUD ($26,765USD; €19,766) per patient. In-hospital care contributed to the majority of total costs (45.7%), followed by community care (42.5%) and outpatient care (6.1%). Mean costs were the highest in class 4 and lowest in class 2 (Table 5). A Kruskal–Wallis test yielded a statistically significant difference in cost values between classes (H = 225.6, p < 0.001). The mean cost per patient in class 2, the class that was associated with improved HRQoL recovery, was significantly lower than all other classes apart from class 3. Conversely, mean cost differences for class 4, which was associated with decreased odds of HRQoL recovery, were significantly higher than all other classes. Mean cost differences between all classes and post hoc Bonferroni test results are presented in Table 6.
Discussion
Several distinct care pathways (i.e. common combinations of health and community care services in the 12 months post-fracture) and the impact of each of these care pathways on the odds of the patients’ HRQoL recovery were identified in a large observational cohort of MOF patients across 10 countries. This study used a patient-level micro-costing approach to estimate the per-patient costs of each site-specific fracture care pathway, and undertake a cost comparison of each care pathway. We found that classes associated with an increased recovery of HRQoL also had lower mean costs per patient across each MOF site. This study supports and facilitates the introduction of site-specific fracture care pathways across a range of healthcare settings.
For hip fractures, participants grouped in class 6 and class 7 were associated with increased odds of HRQoL recovery at 12 months compared to the other classes. Class 7 was the least costly class in hip fracture patients ($28,349 per patient); however, as mentioned in our previous paper [11], this class was not representative of the typical hip fracture cohort (this class had a very low rate of hospitalizations) and was explained by a sizeable country-specific bias (Russian participants). Class 6 was the second least costly, suggesting that participants in this class achieved benefits in HRQoL at a significantly lower cost compared to most classes. Class 6 was characterized by hospital admissions, greater utilization of outpatient healthcare services (including primary care centre visits and allied health visits), and non-opioid analgesics. Similar findings were seen for distal forearm fracture patients, in that the two classes associated with improved odds of HRQoL recovery were also the least costly (classes 3 and 5), although these two classes were quite different in terms of health service use: class 3 was characterized by higher use of outpatient health services (outpatient department visits, primary care centre visits, and allied health visits), whereas class 5 was characterized by hospital presentations without admission and higher medication use (osteoporosis-related; vitamin D/calcium supplementation; non-opioid analgesics). There was no statistically significant difference in costs between these two classes, although both were significantly lower than most. For patients with a vertebral or humeral fracture, one class in each fracture group was associated with improved odds of HRQoL recovery. Both these classes were characterized by ED presentations (without admission), primary care centre visits, and higher osteoporosis-related medication use, vitamin D/calcium supplementation, and non-opioid analgesic use, and were significantly less costly compared to most other classes. Results from this study showed that classes associated with decreased recovery of HRQoL also had the highest rates of healthcare utilization across most healthcare and community service categories, and therefore, higher average cost per patient. This suggests that higher utilization of healthcare may be an indicator of poorer health outcomes in patients post-MOF. This may be explained by the patient demographics of each class (Supplementary File 2), exposing that patients in the ‘improved HRQoL classes’ were generally younger and therefore less frail and most likely less dependent on healthcare services.
Important information is provided in this study on the distribution of healthcare costs post-fracture. In line with previous studies [8, 25,26,27,28], treatment and management of hip fractures in ICUROS participants was associated with the highest costs per patient, followed by vertebral, humeral, and distal forearm fracture patients, respectively. There were substantial differences in health service use at the country level [14], although this was anticipated given the various healthcare system structures across countries participating in the ICUROS. The large economic burden of fractures was predominantly due to in-hospital care, representing over 50% of total direct costs across each fracture site in our study (except for distal forearm fractures). Patients with hip fracture had the highest rate of hospital admissions and subsequent admission to a rehabilitation ward, which contributed to the highest costs per patient. Clinical novel solutions to reduce hospital length of stay and associated in-hospital costs for hip fracture patients are warranted [29]. Admission rates to a RAC facility were low across non-hip fracture groups, similar to results from a recent cohort study that reported risk of institutionalization 6 months after multiple fracture sites compared to hip fractures [30]. In terms of outpatient care, healthcare utilization and costs were similar across each fracture site. While hospitalisations represent the first line of expenses, community care such as health professional home visits, home and equipment modifications, and professional home help services were also a heavy budget item across all fracture sites, close to in-hospital care. Costs for community care were highest in hip fracture patients, driven mainly by higher rates of both formal and informal home help (35.5% and 69.2%, respectively). Annual costs of medication use were similar across each fracture site, although, fracture-related treatment (osteoporosis-related medications and vitamin D/calcium supplements) varied between fractures: it was highest in vertebral fracture patients and lowest in distal forearm fracture patients. Previous longitudinal studies [31, 32] have reported this same variation in osteoporosis pharmaceutical interventions, highlighting that not all fragility fracture patients receive the appropriate care for prevention of subsequent fractures. Total costs for medical imaging were similar across each fracture site; DXA scans were uncommon in patients except for patients with vertebral fracture (27%), once again consistent with prior studies [31, 32].
Strengths and limitations
There were a number of strengths to this study. Health and community care service use was obtained from the largest multi-country, prospective observational study on HRQoL consequences of fractures conducted to date, where variables were captured using the identical study protocol across all 10 countries (excluding the USA). Unit costs of health services were derived from using patient-level data rather than using AR-DRG costing and involved utilizing published Australian Commonwealth and state government resources (IHPA, MBS, and PBS). Additionally, this analysis was undertaken under the guidance of leading experts in economic evaluations [16]. A major strength of the ICUROS was that the population was not restricted to hip fracture patients or hospitalized fracture cases. An important gap in osteoporosis literature is that research on the costs for site-specific fractures other than hip fractures is relatively scarce [33, 34]. This study included health service utilization costs of all four MOF sites allowing for analyses of individual fractures.
However, there are also limitations to this study. First, some of the health service use data was collected using self-report with possible recall bias, though most countries in ICUROS did verify self-report inpatient care with hospital record reviews. Second, the costs determined in this study are related to the Australian healthcare system, which does not include out-of-pocket costs to participants, and as such, may not be able to be directly generalized to healthcare systems in other countries. Australia has a publicly funded universal healthcare system (Medicare) which provides free or low-cost access to government-provided community and hospital care, as well as subsidized pharmaceuticals. Private health insurance gives people a choice outside the public system where the patient contributes towards the cost of health services that are not fully subsidized [35]. Additionally, it may be seen as problematic to estimate costs from one country’s healthcare system where health service use was derived from several countries; however, the alternative of using country-specific unit costs is likely to be non-differential and would introduce further measurement error given that health service costs vary by healthcare systems. Third, the total costs of each care pathway may be underestimated as a number of assumptions regarding health service use had to be made (e.g. days in RAC, hospital admission data was limited to ward type), and indirect costs such as productivity loss and disability were not included. Nevertheless, this study did provide detailed cost information on social and community care such as unpaid care provided by friends and family, home and equipment modifications as a consequence of the fracture, and formal home care (e.g. provision of meals, nursing care, live-in help, etc.), unlike previous costing studies [8, 25, 36, 37]. Finally, we were unable to undertake a traditional cost-effectiveness analysis, as this type of analysis requires a randomized controlled trial in which participants are randomized to a ‘usual care’ group. Potential limitations regarding the ICUROS study design have been described elsewhere [11, 38].
Conclusions
In conclusion, we identified the costs and HRQoL impacts of several multidisciplinary care pathways for individual MOF sites based on the health service utilization of an international cohort of older adults. These care pathways may assist healthcare providers in allocating resources for MOFs in more effective and cost-efficient ways. This will be particularly important for clinicians and healthcare organizations when making plans for a healthcare system capable of addressing the needs of an increasing number of older individuals at significant risk of fracture and HRQoL deficits.
Data availability
The data for these analyses was accessed from the International Costs and Utilities Related to Osteoporotic fractures Study (ICUROS) central database. Access to this database should be discussed with the data custodians (Prof. John Kanis and Prof Fredrik Borgström) and the principal investigators of each participating country (http://www.icuros.org/).
Code availability
Not applicable.
References
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Sànchez-Riera L, Wilson N (2017) Fragility fractures & their impact on older people. Best Pract Res Clin Rheumatol 31:169–191
Talevski J, Sanders KM, Vogrin S et al (2021) Recovery of quality of life is associated with lower mortality 5-year post-fracture: the Australian arm of the International Costs and Utilities Related to Osteoporotic Fractures Study (AusICUROS). Arch Osteoporos 16:112
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Lewiecki EM, Ortendahl JD, Vanderpuye-Orgle J, Grauer A, Arellano J, Lemay J, Harmon AL, Broder MS, Singer AJ (2019) Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR Plus 3:e10192
Tatangelo G, Watts J, Lim K et al (2019) The cost of osteoporosis, osteopenia, and associated fractures in Australia in 2017. J Bone Miner Res 34:616–625
Borgstrom F, Karlsson L, Ortsater G et al (2020) Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos 15:59
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, McCloskey EV, Willers C, Borgstrom F (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16:82
Baaj AA, Downes K, Vaccaro AR, Uribe JS, Vale FL (2011) Trends in the treatment of lumbar spine fractures in the United States: a socioeconomics perspective: clinical article. J Neurosurg Spine 15:367–370
Talevski J, Sanders KM, Busija L, Beauchamp A, Duque G, Borgstrom F, Kanis JA, Svedbom A, Stuart AL, Brennan-Olsen S (2021) Health service use pathways associated with recovery of quality of life at 12-months for individual fracture sites: analyses of the International Costs and Utilities Related to Osteoporotic fractures Study (ICUROS). Bone 144:115805
Svedbom A, Borgstom F, Hernlund E et al (2018) Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos Int 29:557–566
Borgstrom F, Lekander I, Ivergard M et al (2013) The International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS)–quality of life during the first 4 months after fracture. Osteoporos Int 24:811–823
Talevski J, Sanders KM, Busija L et al (2021) Health service use and quality of life recovery 12 months following major osteoporotic fracture: latent class analyses of the International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS). J Bone Miner Res 36:252–261
Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model 14:535–569
Watts JJ, Abimanyi-Ochom J, Sanders KM (2013) Osteoporosis costing all Australians: a new burden of disease analysis - 2012 to 2022. Sydney: Osteoporosis Australia. Available from: https://healthybonesaustralia.org.au/wp-content/uploads/2020/11/Burden-of-Disease-Analysis-2012-2022.pdf. Accessed 11 July 2021
Australian Bureau of Statistics. Consumer price index, Australia. Available at: https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/latest-release. Accessed 11 July 2021
Commonwealth of Australia. Independent Hospital Pricing Authority Annual Report 2020–21. Available from: www.ihpa.gov.au/ihpa-annual-report-2020-21
Department of Health and Ageing (2020) MBS Online. Available from: http://www9.health.gov.au/mbs/search.cfm
The Royal Commission into Aged Care Quality and Safety (2020) The cost of residential aged care (Research Paper 9). 2020. Commonwealth of Australia. Available from: https://agedcare.royalcommission.gov.au/publications/research-paper-9-cost-residential-aged-care
Fair Work Ombudsman (2020) Pay Guide - Social, Community, Home Care and Disability Services Industry Award (MA000100). Available from: https://www.fairwork.gov.au/pay/minimum-wages/social-and-community-services-industry-pay-rates. Accessed: December 2020
Department of Health and Ageing (2020) PBS Online. Available from: https://www.pbs.gov.au/pbs/home
Pharmacy Online Australia (2020) Available from: http://www.pharmacyonline.com.au/. Accessed December 2012
Major G, Ling R, Searles A, Niddrie F, Kelly A, Holliday E, Attia J, Bogduk N (2019) The costs of confronting osteoporosis: cost study of an Australian fracture liaison service. JBMR Plus 3:56–63
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Lindsay R, Burge RT, Strauss DM (2005) One year outcomes and costs following a vertebral fracture. Osteoporos Int 16:78–85
Mahabier KC, Hartog DD, Van Veldhuizen J, Panneman MJ, Polinder S, Verhofstad MH, Van Lieshout EM (2015) Trends in incidence rate, health care consumption, and costs for patients admitted with a humeral fracture in The Netherlands between 1986 and 2012. Injury 46:1930–1937
Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A, Leal J (2017) Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int 28:2791–2800
Talevski J, Guerrero-Cedeno V, Demontiero O, Suriyaarachchi P, Boersma D, Vogrin S, Brennan-Olsen S, Duque G (2020) Implementation of an electronic care pathway for hip fracture patients: a pilot before and after study. BMC Musculoskelet Disord 21:837
Benzinger P, Riem S, Bauer J, Jaensch A, Becker C, Buchele G, Rapp K (2019) Risk of institutionalization following fragility fractures in older people. Osteoporos Int 30:1363–1370
Balasubramanian A, Tosi LL, Lane JM, Dirschl DR, Ho PR, O’Malley CD (2004) Declining rates of osteoporosis management following fragility fractures in the U.S., 2000 through 2009. J Bone Joint Surg Am 96:e52
Leslie WD, Giangregorio LM, Yogendran M, Azimaee M, Morin S, Metge C, Caetano P, Lix LM (2012) A population-based analysis of the post-fracture care gap 1996–2008: the situation is not improving. Osteoporos Int 23:1623–1629
Talevski J, Sanders KM, Duque G, Connaughton C, Beauchamp A, Green D, Millar L, Brennan-Olsen SL (2019) Effect of clinical care pathways on quality of life and physical function after fragility fracture: a meta-analysis. J Am Med Dir Assoc 20:926 e921-926 e911
Bliuc D, Nguyen TV, Eisman JA, Center JR (2014) The impact of nonhip nonvertebral fractures in elderly women and men. J Clin Endocrinol Metab 99:415–423
Willis E, Reynolds L, Keleher H (2016) Understanding the Australian health care system. Elsevier Australia (2nd Edition)
Tarride JE, Guo N, Hopkins R, Leslie WD, Morin S, Adachi JD, Papaioannou A, Bessette L, Brown JP, Goeree R (2012) The burden of illness of osteoporosis in Canadian men. J Bone Miner Res 27:1830–1838
Maravic M, Jouaneton B, Vainchtock A, Tochon V (2012) Economic burden of osteoporosis in women: data from the 2008 French hospital database (PMSI). Clin Exp Rheumatol 30:222–227
Talevski J, Sanders KM, Watts JJ et al (2022) Sex differences in recovery of quality of life 12 months post-fracture in community-dwelling older adults: analyses of the Australian arm of the International Costs and Utilities Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 33:67–75
Acknowledgements
We are grateful to the quality of life and Epidemiology Working Group of the Committee of Scientific Advisors for the International Osteoporosis Foundation under whose supervision this study was undertaken. The Mexican sub-study is grateful to Danai Curiel, and Fernando Carlos MHE Mexico City. The global study team would like to thank Ingrid Lekander, Erik Landfeldt, Martin Kleman, Moa Ivergård, and Viktor Wintzell for contributing to the study. We thank Karen Lim for her assistance with data cleaning for the analyses.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions JT was supported by an Australian National Health and Medical Research Council (NHMRC, of Australia) Postgraduate Scholarship (1151089). On its international level, the ICUROS is sponsored by Amgen, Eli Lilly, Medtronic, Novartis, Sanofi-Aventis, Servier, and Pfizer. In Australia, the study was supported by the National Health and Medical Research Council with supplementary funding from Merck Pty Ltd. In Austria, the study was sponsored by Central Association of Austrian Social Security Institution, Austrian Society for Bone and Mineral Research (AuSBMR), Merck Sharp & Dohme, Servier GmbH, Medtronic GmbH, Amgen GmbH, Novartis GmbH, Nycomed GmbH, Roche GmbH, Sanofi-Aventis GmbH, and Daiichi-Sankyo GmbH. In Mexico, the study was supported by CONACyT. In Lithuania, the work was supported by the National Osteoporosis Center. In the USA, Amgen Inc., Ingenix Pharmaceutical Services, Eli Lilly and Company, Medtronic Spine LLC, and Pfizer (formerly Wyeth) sponsored the study. Hoffmann La Roche and Amgen provided support. In Estonia, the study was supported by the Estonian Science Foundation, and the Estonian Ministry of Education and Research. In Russia, the study was supported by Hoffmann La Roche, Amgen, and the Russian Osteoporosis Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethics approval
ICUROS adhered to the Declaration of Helsinki and was approved by the relevant research ethics committees in each country. Access to ICUROS data was approved from the principal investigators in each country (excluding the USA) and Melbourne Health Human Research Ethics Committee (2010.115).
Consent to participate
Informed consent was obtained from all individual patients included in the study and all study patients could withdraw from the study at any time at their own request.
Consent for publication
All authors approved the final manuscript for publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Talevski, J., Sanders, K.M., Lal, A. et al. A micro-costing analysis of post-fracture care pathways: results from the International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS). Osteoporos Int 33, 1895–1907 (2022). https://doi.org/10.1007/s00198-022-06460-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06460-5