Abstract
Summary
The risk of vertebral fracture is unclear in end-stage renal disease. We report a high vertebral fracture prevalence and incidence in transplantation-eligible patients on dialysis, suggesting that these patients may benefit from radiographic screening for vertebral fractures. Parathyroid hormone had a U-shaped association with vertebral fracture risk.
Introduction
Vertebral fractures are often overlooked, but even undiagnosed vertebral fractures negatively impact physical functioning, quality of life, and mortality. The risk of vertebral fractures in end-stage renal disease (ESRD) patients is unclear, and parathyroid hormone (PTH) might play a role in the development of vertebral fractures. We therefore determined vertebral fracture prevalence and incidence in ESRD patients and assessed associations of vertebral trabecular bone mineral density (BMD) and PTH with vertebral fracture.
Methods
In 146 transplantation-eligible patients on dialysis, we determined vertebral fractures on lateral chest radiographs, which image the thoracic and upper lumbar spine. We determined incident vertebral fractures in 70 patients with follow-up radiographs (23 received a kidney transplant) after median 1.8 years. Vertebral trabecular BMD was measured with computed tomography, and PTH measured with 2-site immunoassays, categorized in tertiles with the middle tertile as reference. We used Poisson regression to assess associations of vertebral trabecular BMD and PTH with vertebral fracture.
Results
Mean age of the study population was 52 ± 13 years, and 98 (67%) were male. Median dialysis duration was 26 (IQR 13–55) months. Vertebral fractures were present in 50/146 patients (34%) and incident vertebral fractures occurred in 20/70 patients (29%). Vertebral trabecular BMD was not associated with vertebral fracture prevalence (relative risk 0.97, 95% CI 0.89 to 1.04). For the lowest PTH tertile (< 11 pmol/L), the relative risk of vertebral fracture was greater although not significant (2.28, 95% CI 0.97 to 5.97) and was significantly greater for the highest PTH tertile (≥ 30 pmol/L; 2.82, 95% CI 1.22 to 7.27) after adjustment for potential confounders.
Conclusions
The prevalence and incidence of vertebral fractures is high even in relatively young and healthy ESRD patients. Vertebral trabecular BMD is not associated with vertebral fracture, and the association of PTH with vertebral fracture risk appears U-shaped. Nevertheless, our study did not measure vertebral BMD using DXA and assessed vertebral fractures using lateral chest radiographs and not spine radiographs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with end-stage renal disease (ESRD) have a high risk of fractures. The risk of hip fractures is four times higher in patients on dialysis compared with the general population [1]. While hip fractures are mostly clinically apparent, many vertebral fractures are presented atypically [2]. Vertebral fractures are easily missed on radiographs [3]. Hence, they often remain undiagnosed, but even undiagnosed vertebral fractures negatively impact physical functioning [4], quality of life [5], and mortality risk [6]. Nevertheless, due to poor documentation in cohorts and dialysis registries, the risk of vertebral fracture in ESRD remains largely unknown [7].
Patients with ESRD have distinct risk factors for fracture beyond traditional risk factors due to chronic kidney disease-mineral and bone disorder [7]. The disturbed bone metabolism, also known as renal osteodystrophy, comprises a spectrum of loss of bone mass due to high bone turnover and microstructural abnormalities due to suppressed bone turnover [8]. These specific types of renal osteodystrophy cannot be distinguished with conventional markers of bone fragility, such as bone mineral density (BMD) [9]. Clinicians commonly rely on parathyroid hormone (PTH) to estimate bone turnover in ESRD; however, the prognostic utility of BMD and PTH for fracture risk in ESRD is unclear [10]. A recent meta-analysis indicated that lower BMD at the lumbar spine was associated with prevalent fractures among patients on dialysis, but not in age-adjusted analyses [11]. This suggests that vertebral BMD may not independently predict fracture risk in ESRD. Furthermore, studies observed that both low and high PTH values were associated with hip and vertebral fracture risk among patients with ESRD, but with various cut-off values [12,13,14,15]. There is also an unclear relationship of PTH with BMD, with three studies of in total 289 patients on dialysis reporting negative associations of PTH with BMD at cortical sites (such as the distal radius), but inconsistent associations with BMD at trabecular sites (such as the spine) [16,17,18].
In this study, we determined vertebral fracture prevalence in patients on dialysis using lateral chest radiographs and determined vertebral fracture incidence in patients with follow-up radiographs, who remained on dialysis or received a kidney transplant. We examined the relationships of vertebral trabecular BMD and PTH with the risk of vertebral fracture and additionally the relationship of PTH with vertebral trabecular BMD.
Materials and methods
Study population
We used data from the NOCTx study, a prospective cohort that compared progression of coronary artery calcification between patients treated with different renal replacement therapies. Between December 2009 and February 2016, NOCTx recruited 181 patients from eight centers in the Netherlands, who were on chronic hemodialysis or peritoneal dialysis with a minimum dialysis duration of 2 months, who were on hemodialysis and switched to nocturnal hemodialysis, or who were on dialysis and received a kidney transplant. At inclusion, all dialysis patients were eligible for transplantation. NOCTx included patients between 18 and 75 years and excluded patients with a life expectancy < 3 months or pre-emptive transplantation. All subjects gave written informed consent. NOCTx has been approved by the Medical Ethics Committee of the University Medical Center Utrecht and was conducted in accordance with the declaration of Helsinki.
Patients were treated according to the KDIGO guidelines by their attending nephrologist [10]. Conventional hemodialysis was delivered 3× 4–5 h per week in-center with default 3.0 mEq/L dialysate calcium. Peritoneal dialysis was delivered as continuous ambulant peritoneal dialysis (n = 16) or automated peritoneal dialysis (n = 8) with default 2.5 mEq/L dialysate calcium. Nocturnal hemodialysis was delivered ≥ 4× 8 h per week at home with default 3.0 mEq/L dialysate calcium. Kidney transplant recipients received standard immunosuppressant regimens consisting of tacrolimus, mycophenolate mofetil, and prednisone in tapering doses (cumulative dose in first 2 months typically 1.0–1.4 g, maintenance dose 5–7.5 mg/day from 3 months post-transplantation). Acute rejections were treated with 3× 1 g of methylprednisolone intravenously.
We studied vertebral fracture prevalence in patients that underwent a lateral chest radiograph as part of routine care within 6 months of inclusion in NOCTx (n = 148). For kidney transplant recipients, this was the screening radiograph performed the day of transplantation. We excluded two patients because of poor-quality radiographs leaving a sample of 146 patients. We studied associations of PTH in all patients with no history of parathyroidectomy and non-missing PTH values (n = 131). We assessed the incidence of vertebral fractures in patients that underwent a second lateral chest radiograph as part of routine care > 1 year after the first radiograph during maximum 3 years follow-up (n = 70).
BMD measurements
In NOCTx, all patients underwent non-enhanced cardiac multi-slice computed tomography (CT) at inclusion, using a single iCT 256 scanner (Philips Medical Systems, Best, the Netherlands), which is checked for image quality and stability at least once every 2 weeks as part of our quality assurance system. The acquisition parameters were as follows: 120 kV, 40–50 mAs, rotation time 270 ms, and 128 × 0.625 mm collimation; table height was set by the attending medical physicist in order to position the patient in the isocenter of the gantry. A single reader (TJ) determined volumetric trabecular BMD of three consecutive thoracic vertebrae in the T7–T10 range [19]. The reader placed a region of interest (ROI) at the center of the vertebra and changed its placement to exclude the cortical edge, bone islands, large veins, or calcified herniated disks, or excluded a vertebra entirely if it was fractured (n = 6). We calculated BMD in milligram per centimeter cube by multiplying the mean CT value per patient (in Hounsfield units) with a calibration factor of 0.871 (calibration factor coefficient of variation 6.1%) [20]. With this iCT 256 scanner-specific calibration factor, vertebral trabecular BMD can be measured accurately without a phantom, correlating highly with phantom-based BMD values (r = 0.987) [20].
In a random sample of 85 scan re-reads by the same reader, the 95% limits of agreement were − 7.6 (95% CI − 8.4 to − 6.8) and 11.5 (95% CI 10.7 to 12.3) mg/cm3, and intra-observer reliability (ICCagreement) was 0.99. In previous studies, the interscan variation has been shown to be low (2.8%) [19].
Parathyroid hormone
Parathyroid hormone was measured as part of routine care at clinical laboratories, with intact 2-site immunoassays (Beckman-Coulter, Fullerton, USA; Abbott Diagnostics, Abbott Park, USA; or Roche Diagnostics, Indianapolis, USA). Reference intervals of these assays are 1.3–9.3 pmol/L, 1.6–7.2 pmol/L, and 1.6–6.9 pmol/L, respectively. PTH values were averaged over measurements of the 3 months preceding the first lateral chest radiograph (mostly two measurements (60%), range 1–4 measurements).
Vertebral fracture assessment
Using lateral chest radiographs, which show the thoracic and upper lumbar spine, two trained physicians (TJ and NG) independently identified vertebral fractures and graded them according to Genant’s semiquantitative method [21]. This method allows to exclude other possible causes of vertebral deformity, such as Scheuermann’s disease, remodeling of vertebral bodies due to degenerative disk disease, or scoliosis. Lateral chest radiographs are reliable for the diagnosis of vertebral fractures, with excellent agreement and reliability compared with lateral spine radiographs (95–98% and 0.88–0.91, respectively) [22]. Fractures were graded by type (wedge, biconcave, or crush deformity) and severity: grade 1 (20–25% height loss), grade 2 (25–40% height loss), or grade 3 (> 40% height loss). All radiographs were re-read in consensus readings and verified by an expert geriatrician (HW). On average, we evaluated 10.8 ± 1.4 vertebrae per patient, which included the seventh thoracic vertebra in 145 (99%) patients and the first lumbar vertebra in 124 (85%) patients. The prevalence of vertebral fractures did not differ significantly between patients with ≤ 10 evaluable vertebrae (18/61 fractures) and patients with > 10 evaluable vertebrae (32/85 fractures) (P = 0.40).
We defined the incidence of a fracture as any new vertebral fracture not present on the first radiograph or deterioration of an existing fracture to a higher grade. We defined the follow-up time as the time between the first and second radiographs. We evaluated an average of 10.6 ± 1.3 vertebrae per patient, which included the seventh thoracic vertebra in all patients and the first lumbar vertebra in 53 (76%) patients.
Other study variables
At inclusion, study personnel recorded demographics at the University Medical Center Utrecht. Body mass index was calculated by dividing weight (kg) by height (m2), based on chart review. Smoking status was self-reported and categorized as current and non-current smoking. Biochemical parameters (total calcium, albumin, phosphate, C-reactive protein, and total alkaline phosphatase) were measured in clinical laboratories in the 8 recruiting centers, and values were averaged over measurements of 3 months preceding inclusion (commonly 2–3 measurements). Medication use and medical history were assessed by chart review. We defined dialysis duration as the time between the first day of dialysis and the inclusion date, minus the time with a functioning kidney transplant, expressed in months.
Statistical analyses
We reported normally distributed variables as mean (± standard deviation), non-normally distributed variables as median (interquartile range, IQR), and categorical data as number (percentage). We tabulated patient characteristics according to vertebral fracture prevalence. We categorized PTH as tertiles, as we expected a U-shaped relationship with vertebral fracture [7].
We evaluated associations of kidney transplantation versus dialysis with vertebral fracture incidence, of vertebral trabecular BMD with vertebral fracture prevalence, and lastly of PTH tertiles with both vertebral fracture prevalence and vertebral trabecular BMD. For vertebral fracture prevalence and incidence as outcome measure, we used Poisson regression due to the high event rate and reported relative risks (RR) with 95% confidence intervals (CI) [23]. For vertebral fracture prevalence as outcome measure, we adjusted for potential confounders age (years), sex, dialysis duration (months), and diabetes (type I or type II/absent). For vertebral fracture incidence as outcome measure, we adjusted for age (years), sex, and follow-up time (years), and stratified by dialysis or kidney transplantation, as we suspected distinct fracture etiologies. For vertebral trabecular BMD as outcome measure, we used linear regression and adjusted for potential confounders as described above.
To evaluate the continuous associations of PTH with vertebral fracture prevalence and vertebral trabecular BMD, we constructed P-splines adjusted for age (years) and sex [24]. We considered P values ≤ 0.05 (two-tailed) statistically significant and used R 3.4.1 (R Foundation Statistical Computing) for all analyses.
Sensitivity analyses
To test the robustness of the associations, we repeated the analyses of the association of PTH with vertebral fracture prevalence stratified by age (< 50 or ≥ 50 years); sex; history of diabetes, cardiovascular disease, current smoking, or transplantation; treatment with hemodialysis or peritoneal dialysis; use of prednisone; calcium-containing phosphate binders; vitamin D analogues; and cinacalcet. Furthermore, we repeated the analyses of the association of vertebral trabecular BMD with vertebral fracture prevalence excluding grade 1 fractures.
Results
Study population
The mean age of the study population (n = 146) was 52 ± 13 years, 98 (67%) were male, median dialysis duration was 26 (IQR 13–55) months, and 18 (12%) had diabetes. Eighteen patients (12%) were on long-term corticosteroids (low-dose up to 10 mg/day), while none used bisphosphonates and 23 (18%) used cinacalcet.
Patients that could not be evaluated for vertebral fractures (n = 35) due to missing radiographs were similar in patient characteristics: mean age 51 ± 14 years, 23 (66%) were male, median dialysis duration was 31 (IQR 15–74) months, and eight (23%) had diabetes (Table S1).
Vertebral fracture prevalence and incidence
In total, 50 patients (34%) had 84 prevalent vertebral fractures. Patients with prevalent vertebral fractures were older, more often male, had longer dialysis durations, and more often used cinacalcet than patients without prevalent vertebral fractures (Table 1).
We assessed incident vertebral fractures in a subset of 70 patients: 47 who continued treatment with dialysis and 23 who received a kidney transplant at inclusion. The kidney transplant recipients (n = 23) had a mean estimated glomerular filtration rate of 54 ± 19 mL/min/1.73m2.
Patients that could not be evaluated for incident vertebral fractures (n = 76) were similar in patient characteristics: mean age 51 ± 13 years, 23 (70%) were male, median dialysis duration was 31 (IQR 16–64) months, and 9 (12%) had diabetes. Furthermore, these patients were similar regarding treatment modality (38 patients on hemodialysis, 13 on peritoneal dialysis, 25 kidney transplant recipients versus 35, 12, and 23, respectively) and vertebral fracture prevalence (27/76 patients, 36% versus 23/70, 33%).
After a median follow-up of 1.8 years (IQR 1.3–2.7) or 137 person-years, 20 patients (29%) developed 24 new vertebral fractures. Compared with patients without incident vertebral fracture, patients with incident vertebral fracture were older (mean 60 versus 52 years) and had more often a previous vertebral fracture (55% versus 24%) (Table 2). Patient characteristics of patients that received a kidney transplant (n = 23) and patients that remained on dialysis (n = 47) were comparable (Table S2), although the use of corticosteroids and bisphosphonates during follow-up was higher among kidney transplant recipients (100% versus 21% and 17% versus none). The risk of incident vertebral fracture did not differ significantly for kidney transplant recipients (6/23 with incident vertebral fracture) compared with patients on dialysis (14/47 with incident vertebral fracture) after adjustment for age, sex, and follow-up time (adjusted RR for kidney transplant recipients compared with patients on dialysis 0.94, 95% CI 0.32 to 2.43).
Associations of vertebral trabecular BMD with vertebral fracture
Mean vertebral trabecular BMD was 139 ± 41 mg/cm3 in patients without a prevalent vertebral fracture (n = 96) and 120 ± 44 mg/cm3 in patients with a prevalent vertebral fracture (n = 50). Vertebral trabecular BMD was associated with a lower risk of vertebral fracture prevalence in unadjusted models 0.93 (95% CI 0.86 to 0.99) but not when adjusted for potential confounders 0.97 (95% CI 0.89 to 1.04) (Table S3). These associations were numerically similar when grade 1 fractures (n = 32) were excluded (unadjusted 0.90, 95% CI 0.79 to 1.01; and adjusted 0.95, 95% CI 0.83 to 1.06).
Associations of PTH with vertebral fracture and vertebral trabecular BMD
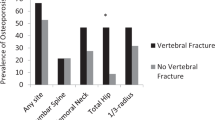
One hundred thirty-one patients had no history of parathyroidectomy and non-missing PTH values (Table S4). Vertebral fractures were the least prevalent in patients in the middle PTH tertile (16% versus 38% and 43%; P < 0.05) (Table 3). Compared with the middle tertile, the adjusted RR of vertebral fracture prevalence was 2.28 for the lowest tertile (95% CI 0.97 to 5.97) and 2.82 for the highest tertile (95% CI 1.22 to 7.27). Correspondingly, the continuous association of PTH with prevalent vertebral fracture risk appeared U-shaped, with the lowest risk around 29 pmol/L (Fig. 1). Notably, patients in the lowest tertile had significantly lower total alkaline phosphatase levels (median 69 versus 85 and 91 IU/L, P = 0.02).
We repeated these analyses stratified by various patient characteristics (Table S5), which all showed similar trends. The U-shaped association of PTH with vertebral fracture risk appeared even stronger in vitamin D analogues users (n = 87) (adjusted RR 3.68, 95% CI 1.12 to 16.52 for the lowest and 3.57, 95% CI 1.14 to 15.61 for the highest PTH tertile). Patient characteristics were similar between vitamin D analogue users and non-users (Table S6), except for higher phosphate (1.49 versus 1.19 mmol/L) and PTH values (23 versus 11 pmol/L) among vitamin D analogue users.
In the lowest PTH tertile, vertebral trabecular BMD tended to be lower with linear regression compared with the middle tertile (adjusted regression coefficient − 9.7 mg/cm3, 95% CI − 22.7 to 3.3), while in the highest tertile vertebral trabecular BMD was significantly higher (14.6 mg/cm3, 95% CI 1.4 to 27.8) (Table 3). For the continuous associations, lower PTH values tended to track with lower vertebral trabecular BMD values (Figure S1).
Discussion
Our study indicates that vertebral fractures have a high prevalence (34%) and incidence (29% after median 1.8 years follow-up) in a relatively young population (mean age 52 years) of patients with ESRD. Also, our data show no relationship of CT-measured vertebral trabecular BMD with vertebral fracture and suggest a U-shaped relationship of PTH with vertebral fracture.
The vertebral fracture prevalence in our study is remarkably high compared with the general population. In a population-based study of European men and women aged 50–54 years, the prevalence ranged between 5 and 17% as determined with morphometric approaches [25], and between 2 and 11% in a population-based study of Dutch men and women aged 45–59 years as determined with algorithm-based qualitative methods and a morphometric approach [26]. In general, reproducibility is highest with algorithm-based qualitative methods [27], followed by Genant’s semiquantitative technique used by us, which in turn has higher reproducibility than morphometric approaches (e.g., the McCloskey and Eastell methods and quantitative morphometry) [28]. Considering, vertebral fracture prevalence in our ESRD cohort is more than twice as high as in the general population, which could have been even higher if we had also evaluated the lower lumbar spine.
The prevalence of vertebral fractures is poorly documented in cohorts and dialysis registries [7] and has been reported in only few studies of patients on dialysis [29]. Four studies reported prevalences between 21 and 33% for patients generally older (mean ages between 54 and 69 years) [14, 30,31,32], whereas one study reported 9% vertebral fractures without mentioning age of the study population or method of vertebral fracture assessment [33] and another study reported 11% vertebral fractures among slightly younger incident kidney transplant recipients (49.7 versus 52.2 years), although it was unclear whether only the lumbar spine was evaluated [34]. In general, our estimates might be higher due to geographic variation in vertebral fracture prevalence between Northern and Southern Europe [25] or different referral patterns for dialysis [35]. Also, one of these studies used stricter criteria for wedge fractures (the most common type of vertebral fracture [26]) only adjudicating grade 2 and 3 fractures [14], and another study did not specify vertebral fracture adjudication method [34]. Yet another study found 55% vertebral fractures in older patients on hemodialysis (mean 64 years old) but used quantitative morphometry [36]. We employed Genant’s semiquantitative technique to adjudicate fractures, which allows to exclude other possible causes of vertebral deformity [21] and has a higher reproducibility than morphometric approaches used in previous studies [28]. This supports the high vertebral fracture prevalence of 34% we currently report.
Our study is the first to report vertebral fracture incidence in patients with ESRD using radiographs to assess vertebral fractures. Two previous studies reported 4.8 [12] and about 10 [37] vertebral fractures per 1000 person-years in patients on dialysis, with vertebral fractures identified by International Classification of Diseases, Ninth revision (ICD-9) codes in claim files of the United States Renal Data system. However, this methodology is likely to underestimate vertebral fracture incidence because of clinical underdiagnosis [3]. We used standardized methods by 2 independent trained physicians to adjudicate fractures, which is much more sensitive than ICD-9 codes. Our data indicate a high vertebral fracture incidence (146 per 1000 person-years) among patients with ESRD. Although causes of vertebral fracture may differ for patients on dialysis and kidney transplant recipients, our data showed similar vertebral fracture rates for both groups, far exceeding rates reported in placebo groups of large osteoporosis drug trials [38]. This high incidence warrants a better understanding of the impact of mineral metabolism disturbances on bone strength in order to prevent these fractures.
In this first study to measure vertebral trabecular BMD with cardiac CT in patients with ESRD, we did not find associations of vertebral trabecular BMD with vertebral fracture, similar to a previous study using quantitative CT [32]. Cardiac CT vertebral trabecular BMD correlates well with quantitative CT lumbar spine BMD (r = 0.91–0.93) [19], which is considered a useful and appropriate method for BMD testing [39, 40]. The discrepancy between vertebral trabecular BMD and fracture might be explained by physiological anabolic effects of PTH, which are most pronounced on trabecular bone [41]. Indeed, we found an association of higher PTH with higher vertebral trabecular BMD, whereas previous studies reported inconsistent associations [16,17,18]. Because of this, vertebral trabecular BMD may not be useful to assess fracture risk in ESRD. Moreover, our findings indicate that BMD testing is redundant in these patients. The clinical purpose of BMD is to identify high-risk patients for fracture, but with the currently reported vertebral fracture risk, patients on dialysis can all be regarded as high-risk patients for fracture and rather may benefit from radiographic screening for vertebral fractures.
Our data suggest a U-shaped association of PTH with vertebral fracture risk. We used continuous associations to indicate the precise direction of the associations per PTH picomoles per liter. This allowed us to estimate the shape of fracture risk for the whole range of PTH compared with predefined PTH categories or quantiles, indicating the lowest vertebral fracture risk around 29 pmol/L. Our finding complements previous studies reporting optimal PTH values for fracture risk around 32 pmol/L [12], above 21 pmol/L [13], above 7 pmol/L [14], between 16 and 32 pmol/L [15], and below 95 pmol/L [42]. In order to draw conclusions about the target PTH range in clinical practice, randomized controlled trials are needed to define optimal PTH values for fracture.
Our results should be interpreted within certain limitations. We used lateral chest radiographs and not spine radiographs, which may have complicated vertebral fracture diagnosis, although lateral chest radiographs have excellent agreement and reliability compared with spine radiographs [22]. Also, lateral chest radiographs did not allow for fracture assessment of the lower lumbar spine, as we could only evaluate the spine down to the first lumbar vertebra in most patients. Nevertheless, one could even expect a higher prevalence of vertebral fractures with additional lumbar spine radiography. Furthermore, the radiographs were performed as part of routine care, which may have introduced indication bias. However, only two radiographs (1%) were performed with the indication of back pain. Another limitation is that the majority of our study population was male, while it has been indicated that the inter-observer agreement is not good for the diagnosis of vertebral fracture in males [43]. Further limitations include that PTH was measured with multiple assays, that we did not additionally measure vertebral BMD using conventional dual-energy X-ray absorption (DXA), and that we did not have data on historical corticosteroid use or vitamin D status. Notwithstanding, most patients used vitamin D analogues, rendering vitamin D deficiency unlikely as cause of vertebral fractures. Finally, all patients in this study were eligible for transplantation and some were treated with home hemodialysis. This population may therefore be somewhat healthier than the average dialysis population. On the other hand, a high vertebral fracture risk in our population indicates an even higher risk in the general dialysis population.
This study has several strengths. We adjudicated fractures on radiographs based on 2 independent trained physicians, instead of recall of fracture history or radiographic reports. We thus also detected less severe fractures, corroborating the high vertebral fracture prevalence. Also, the patients on dialysis and kidney transplant recipients were well comparable, as all dialysis patients were eligible for transplantation, and all kidney transplant recipients were on dialysis before transplantation.
In conclusion, even relatively young and healthy patients with ESRD are at high risk of vertebral fractures. CT-measured vertebral trabecular BMD is not associated with vertebral fracture and may therefore not be useful to assess fracture risk in ESRD. Rather, patients may benefit from radiographic screening for vertebral fractures. Nevertheless, our study did not measure vertebral BMD using DXA and assessed vertebral fractures using lateral chest radiographs and not spine radiographs. The association of PTH with vertebral fracture risk appears to be U-shaped, with the lowest risk around 29 pmol/L. The target PTH range for fracture needs investigation by randomized controlled trials.
References
Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C (2000) Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 58:396–399
van der Jagt-Willems HC, van Munster BC, Lems WF (2013) Vertebral fractures in elderly adults: atypical presentation rather than asymptomatic. J Am Geriatr Soc 61:2047–2048
Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL, Group IS (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20:557–563
Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, Segal M, Genant HK, Cummings SR (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J (2000) Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 15:1384–1392
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Pimentel A, Urena-Torres P, Zillikens MC, Bover J, Cohen-Solal M (2017) Fractures in patients with CKD-diagnosis, treatment, and prevention: a review by members of the European Calcified Tissue Society and the European Renal Association of Nephrology Dialysis and Transplantation. Kidney Int 92:1343–1355
Malluche HH, Porter DS, Monier-Faugere MC, Mawad H, Pienkowski D (2012) Differences in bone quality in low- and high-turnover renal osteodystrophy. J Am Soc Nephrol 23:525–532
Salam S, Gallagher O, Gossiel F, Paggiosi M, Khwaja A, Eastell R (2018) Diagnostic Accuracy of Biomarkers and Imaging for Bone Turnover in Renal Osteodystrophy. J Am Soc Nephrol 29:1557–1565
Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, Moe SM, Shroff R, Tonelli MA, Toussaint ND, Vervloet MG, Leonard MB (2018) Diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder: synopsis of the kidney disease: Improving global outcomes 2017 Clinical Practice Guideline Update. Ann Intern Med 168:422–430
Bucur RC, Panjwani DD, Turner L, Rader T, West SL, Jamal SA (2015) Low bone mineral density and fractures in stages 3-5 CKD: an updated systematic review and meta-analysis. Osteoporos Int 26:449–458
Danese MD, Kim J, Doan QV, Dylan M, Griffiths R, Chertow GM (2006) PTH and the risks for hip, vertebral, and pelvic fractures among patients on dialysis. Am J Kidney Dis 47:149–156
Coco M, Rush H (2000) Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 36:1115–1121
Atsumi K, Kushida K, Yamazaki K, Shimizu S, Ohmura A, Inoue T (1999) Risk factors for vertebral fractures in renal osteodystrophy. Am J Kidney Dis 33:287–293
Iimori S, Mori Y, Akita W, Kuyama T, Takada S, Asai T, Kuwahara M, Sasaki S, Tsukamoto Y (2012) Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients--a single-center cohort study. Nephrol Dial Transplant 27:345–351
Urena P, Bernard-Poenaru O, Ostertag A, Baudoin C, Cohen-Solal M, Cantor T, de Vernejoul MC (2003) Bone mineral density, biochemical markers and skeletal fractures in haemodialysis patients. Nephrol Dial Transplant 18:2325–2331
Lacativa PG, de Mendonca LM, de Mattos Patricio Filho PJ, Pimentel JR, da Cruz Goncalves MD, Fleiuss de Farias ML (2005) Risk factors for decreased total body and regional bone mineral density in hemodialysis patients with severe secondary hyperparathyroidism. J Clin Densitom 8:352–361
Jorgensen HS, Winther S, Bottcher M, Hauge EM, Rejnmark L, Svensson M, Ivarsen P (2017) Bone turnover markers are associated with bone density, but not with fracture in end stage kidney disease: a cross-sectional study. BMC Nephrol 18:284
Budoff MJ, Khairallah W, Li D, Gao YL, Ismaeel H, Flores F, Child J, Carson S, Mao SS (2012) Trabecular bone mineral density measurement using thoracic and lumbar quantitative computed tomography. Acad Radiol 19:179–183
Budoff MJ, Malpeso JM, Zeb I, Gao YL, Li D, Choi TY, Dailing CA, Mao SS (2013) Measurement of phantomless thoracic bone mineral density on coronary artery calcium CT scans acquired with various CT scanner models. Radiology 267:830–836
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
van der Jagt-Willems HC, van Munster BC, Leeflang M, Beuerle E, Tulner CR, Lems WF (2014) Diagnosis of vertebral fractures on lateral chest X-ray: intraobserver agreement of semi-quantitative vertebral fracture assessment. Eur J Radiol 83:2177–2180
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706
Eilers PHC, Marx BD (1996) Flexible smoothing with B-splines and penalties. Stat Sci 11:89–102
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1018
Oei L, Koromani F, Breda SJ et al (2018) Osteoporotic vertebral fracture prevalence varies widely between qualitative and quantitative radiological assessment methods: the Rotterdam study. J Bone Miner Res 33:560–568
Lentle BC, Berger C, Probyn L et al (2018) Comparative analysis of the Radiology of osteoporotic vertebral fractures in women and men: cross-sectional and longitudinal observations from the Canadian Multicentre Osteoporosis Study (CaMos). J Bone Miner Res 33:569–579
Grados F, Roux C, de Vernejoul MC, Utard G, Sebert JL, Fardellone P (2001) Comparison of four morphometric definitions and a semiquantitative consensus reading for assessing prevalent vertebral fractures. Osteoporos Int 12:716–722
Sidibe A, Auguste D, Desbiens LC, Fortier C, Wang YP, Jean S, Moore L, Mac-Way F (2019) Fracture risk in dialysis and kidney transplanted patients: a systematic review. JBMR Plus 3:45–55
Rodriguez-Garcia M, Gomez-Alonso C, Naves-Diaz M, Diaz-Lopez JB, Diaz-Corte C, Cannata-Andia JB, Asturias Study G (2009) Vascular calcifications, vertebral fractures and mortality in haemodialysis patients. Nephrol Dial Transplant 24:239–246
Jamal SA, Chase C, Goh YI, Richardson R, Hawker GA (2002) Bone density and heel ultrasound testing do not identify patients with dialysis-dependent renal failure who have had fractures. Am J Kidney Dis 39:843–849
Mares J, Ohlidalova K, Opatrna S, Ferda J (2009) Determinants of prevalent vertebral fractures and progressive bone loss in long-term hemodialysis patients. J Bone Miner Metab 27:217–223
Mohini R, Dumler F, Rao DS (1991) Skeletal surveys in renal osteodystrophy. ASAIO Trans 37:635–637
Segaud N, Legroux I, Hazzan M, Noel C, Cortet B (2018) Changes in bone mineral density after kidney transplantation: 2-year assessment of a French cohort. Osteoporos Int 29:1165–1175
Mendelssohn DC, Kua BT, Singer PA (1995) Referral for dialysis in Ontario. Arch Intern Med 155:2473–2478
Fusaro M, Tripepi G, Noale M, Vajente N, Plebani M, Zaninotto M, Guglielmi G, Miotto D, Dalle Carbonare L, D'Angelo A, Ciurlino D, Puggia R, Miozzo D, Giannini S, Gallieni M (2013) High prevalence of vertebral fractures assessed by quantitative morphometry in hemodialysis patients, strongly associated with vascular calcifications. Calcif Tissue Int 93:39–47
Beaubrun AC, Kilpatrick RD, Freburger JK, Bradbury BD, Wang L, Brookhart MA (2013) Temporal trends in fracture rates and postdischarge outcomes among hemodialysis patients. J Am Soc Nephrol 24:1461–1469
Black DM, Cummings SR, Karpf DB et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Expert Panel on Musculoskeletal I, Ward RJ, Roberts CC et al (2017) ACR Appropriateness Criteria((R)) Osteoporosis and Bone Mineral Density. J Am Coll Radiol 14:S189–S202
Kanis JA, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for C, Economic Aspects of O, the Committees of Scientific A, National Societies of the International Osteoporosis F (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Goltzman D (2018) Physiology of parathyroid hormone. Endocrinol Metab Clin N Am 47:743–758
Jadoul M, Albert JM, Akiba T, Akizawa T, Arab L, Bragg-Gresham JL, Mason N, Prutz KG, Young EW, Pisoni RL (2006) Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int 70:1358–1366
Fechtenbaum J, Briot K, Paternotte S, Audran M, Breuil V, Cortet B, Debiais F, Grados F, Guggenbuhl P, Laroche M, Legrand E, Lespessailles E, Marcelli C, Orcel P, Szulc P, Thomas T, Kolta S, Roux C, bone section of the French Rheumatology Society (2014) Difficulties in the diagnosis of vertebral fracture in men: Agreement between doctors. Joint Bone Spine 81:169–174
Funding
The NOCTx study was financially supported by unrestricted grants from Amgen, Baxter, Fresenius Medical Care, Novartis, Roche, and Shire Pharmaceuticals. Thijs Thomas Jansz was supported financially by a grant from the Wellerdieck de Goede foundation mediated by the Friends of UMC Utrecht foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All subjects gave written informed consent. NOCTx has been approved by the Medical Ethics Committee of the University Medical Center Utrecht and was conducted in accordance with the declaration of Helsinki.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jansz, T.T., Goto, N.A., van Ballegooijen, A.J. et al. The prevalence and incidence of vertebral fractures in end-stage renal disease and the role of parathyroid hormone. Osteoporos Int 31, 515–524 (2020). https://doi.org/10.1007/s00198-019-05187-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05187-0