Abstract
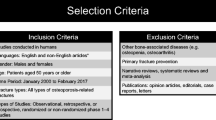
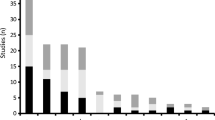
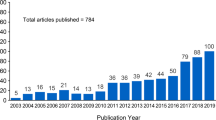
The analysis aimed to identify the treatment gaps in current fracture liaison services (FLS) and to provide recommendations for best practice establishment of future FLS across the Asia-Pacific region. The findings emphasize the unmet need for the implementation of new programs and provide recommendations for the refinement of existing ones. The study’s objectives were to evaluate fracture liaison service (FLS) programs in the Asia-Pacific region and provide recommendations for establishment of future FLS programs. A systematic literature review (SLR) of Medline, PubMed, EMBASE, and Cochrane Library (2000–2017 inclusive) was performed using the following keywords: osteoporosis, fractures, liaison, and service. Inclusion criteria included the following: patients ≥ 50 years with osteoporosis-related fractures; randomized controlled trials or observational studies with control groups (prospective or retrospective), pre–post, cross-sectional and economic evaluation studies. Success of direct or indirect interventions was assessed based on patients’ understanding of risk, bone mineral density assessment, calcium intake, osteoporosis treatment, re-fracture rates, adherence, and mortality, in addition to cost-effectiveness. Overall, 5663 unique citations were identified and the SLR identified 159 publications, reporting 37 studies in Asia-Pacific. These studies revealed the unmet need for public health education, adequate funding, and staff resourcing, along with greater cooperation between departments and physicians. These actions can help to overcome therapeutic inertia with sufficient follow-up to ensure adherence to recommendations and compliance with treatment. The findings also emphasize the importance of primary care physicians continuing to prescribe treatment and ensure service remains convenient. These findings highlight the limited evidence supporting FLS across the Asia-Pacific region, emphasizing the unmet need for new programs and/or refinement of existing ones to improve outcomes. With the continued increase in burden of fractures in Asia-Pacific, establishment of new FLS and assessment of existing services are warranted to determine the impact of FLS for healthcare professionals, patients, family/caregivers, and society.
Similar content being viewed by others
References
Organisation WH (2004) WHO scientific group on the assessment of osteoporosis at primary health care level: summary meeting report. In: Organisation WH (ed)
Curtis E, Moon R, Dennison E, Harvey N, Cooper C (2016) Recent advances in the pathogenesis and treatment of osteoporosis. Clin Med (London) 16(4):360–364. https://doi.org/10.7861/clinmedicine.16-4-360
Kanis JA (2007) Assessment of osteoporosis at the primary health care level. University of Sheffield, UK
IOF IOF (2013) The Asia-Pacific regional audit: epidemiology, costs & burden of osteoporosis
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413. https://doi.org/10.1007/PL00004148
IOF IOF (2009) The Asian audit: epidemiology, costs, and burden of osteoporosis in Asia 2009
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Jiang Y, Ni W (2016) Expected lifetime numbers, risks, and burden of osteoporotic fractures for 50-year old Chinese women: a discrete event simulation incorporating FRAX. J Bone Miner Metab 34(6):714–722. https://doi.org/10.1007/s00774-015-0724-9
Karlsson MK, Hasserius R, Obrant KJ (1993) Individuals who sustain nonosteoporotic fractures continue to also sustain fragility fractures. Calcif Tissue Int 53(4):229–231. https://doi.org/10.1007/BF01320906
CH W, ST T, Chang YF, Chan DC, Chien JT, Lin CH et al (2017) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Osteoporos Sarcopenia 3:S51–SS2
Bliuc D, Eisman JA, Center JR (2006) A randomized study of two different information-based interventions on the management of osteoporosis in minimal and moderate trauma fractures. Osteoporos Int 17(9):1309–1317. https://doi.org/10.1007/s00198-006-0078-1
Inderjeeth C, Raymond W, Geelhoed E, Briggs A, Briffa K, Oldham D et al. (eds) (2016) OPO103 Fracture liaison service implemented in a metropolitan tertiary centre in Western Australia improved treatment and recurrent fracture rates by 12 months. EULAR. Ann Rheum Dis
Moriwaki K, Komaba H, Noto S, Yanagisawa S, Takiguchi T, Inoue H, Toujo T, Fukagawa M, Takahashi HE (2013) Cost-effectiveness of alendronate for the treatment of osteopenic postmenopausal women in Japan. J Bone Miner Res 28(2):395–403. https://doi.org/10.1002/jbmr.1755
Chan DC, Hung LW, Chang CH, Peng JK, Chou YC, Chiu WY et al (2013) Fragility fracture liaison service at National Taiwan University Hospital. Osteoporos Int 24:S649
Lo P, Wen Y, Tsai Y (2015) PMS57 Cost-effectiveness analysis of biphosphonates for secondary prevention of hip fracture in Taiwan. Value Health 18(3):A162–A1A3. https://doi.org/10.1016/j.jval.2015.03.942
Hung LW, Hong CH, Yang RS, Chan DC (eds) (2016) Improving hip fracture care in northern Taiwan: a preliminary results of the hip fracture patients. FFN Global Congress
Amphansap T, Stitkitti N, Dumrongwanich P (2016) Evaluation of Police General Hospital’s fracture liaison service (PGH’s FLS): the first study of a fracture liaison service in Thailand. Osteoporos Sarcopenia 2(4):238–243. https://doi.org/10.1016/j.afos.2016.09.002
Barrack CM, McGirr EE, Fuller JD, Foster NM, Ewald DP (2009) Secondary prevention of osteoporosis post minimal trauma fracture in an Australian regional and rural population. Aust J Rural Health 17(6):310–315. https://doi.org/10.1111/j.1440-1584.2009.01103.x
Chandran M, Cheen M, Ying H, Lau TC, Tan M (2016) Dropping the ball and falling off the care wagon. Factors correlating with nonadherence to secondary fracture prevention programs. J Clin Densitom 19(1):117–124. https://doi.org/10.1016/j.jocd.2015.06.009
Chandran M, Tan MZ, Cheen M, Tan SB, Leong M, Lau TC (2013) Secondary prevention of osteoporotic fractures—an “OPTIMAL” model of care from Singapore. Osteoporos Int 24(11):2809–2817. https://doi.org/10.1007/s00198-013-2368-8
Chen JS, Hogan C, Lyubomirsky G, Sambrook PN (2009) Management of osteoporosis in primary care in Australia. Osteoporos Int 20(3):491–496. https://doi.org/10.1007/s00198-008-0686-z
Cooper MS, Palmer AJ, Seibel MJ (2012) Cost-effectiveness of the concord minimal trauma fracture liaison service, a prospective, controlled fracture prevention study. Osteoporos Int 23(1):97–107. https://doi.org/10.1007/s00198-011-1802-z
Fisher AA, Davis MW, Rubenach S, Sivakumaran S, Smith P, Budge M (2006) Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma 20(3):172–180. https://doi.org/10.1097/01.bot.0000202220.88855.16
Fraser S, Wong PK (2017) Secondary fracture prevention needs to happen in the country too: the first two and a half years of the Coffs Fracture Prevention Clinic. Aust J Rural Health 25(1):28–33. https://doi.org/10.1111/ajr.12291
Ganda K, Schaffer A, Pearson S, Seibel MJ (2014) Compliance and persistence to oral bisphosphonate therapy following initiation within a secondary fracture prevention program: a randomised controlled trial of specialist vs. non-specialist management. Osteoporos Int 25(4):1345–1355. https://doi.org/10.1007/s00198-013-2610-4
Ganda K, Schaffer A, Seibel MJ (2015) Predictors of re-fracture amongst patients managed within a secondary fracture prevention program: a 7-year prospective study. Osteoporos Int 26(2):543–551. https://doi.org/10.1007/s00198-014-2880-5
Huang CM, CY S, Chien LY, Guo JL (2011) The effectiveness of an osteoporosis prevention program among women in Taiwan. Appl Nurs Res 24(4):e29–e37. https://doi.org/10.1016/j.apnr.2010.02.006
Inderjeeth C, Glennon D, Poland K, Ingram K, Prince R, Van V et al (2010) A multimodal intervention to improve fragility fracture management in patients presenting to emergency departments. Med J Aust 193(3):149–153
Jones G, Warr S, Francis E, Greenaway T (2005) The effect of a fracture protocol on hospital prescriptions after minimal trauma fractured neck of the femur: a retrospective audit. Osteoporos Int 16(10):1277–1280. https://doi.org/10.1007/s00198-005-1960-y
Kim D, Mackenzie D, Cutfield R (2016) Implementation of fracture liaison service in a New Zealand public hospital: Waitemata district health board experience. N Z Med J 129(1445):50–55
Kuo I, Ong C, Simmons L, Bliuc D, Eisman J, Center J (2007) Successful direct intervention for osteoporosis in patients with minimal trauma fractures. Osteoporos Int 18(12):1633–1639. https://doi.org/10.1007/s00198-007-0418-9
Laslett LL, Whitham JN, Gibb C, Gill TK, Pink JA, McNeil JD (2007) Improving diagnosis and treatment of osteoporosis: evaluation of a clinical pathway for low trauma fractures. Arch Osteoporos 2(1–2):1–6. https://doi.org/10.1007/s11657-007-0010-0
Lih A, Nandapalan H, Kim M, Yap C, Lee P, Ganda K, Seibel MJ (2011) Targeted intervention reduces refracture rates in patients with incident non-vertebral osteoporotic fractures: a 4-year prospective controlled study. Osteoporos Int 22(3):849–858. https://doi.org/10.1007/s00198-010-1477-x
Lin PC, Wang CH, Chen CS, Liao LP, Kao SF, HF W (2009) To evaluate the effectiveness of a discharge-planning programme for hip fracture patients. J Clin Nurs 18(11):1632–1639. https://doi.org/10.1111/j.1365-2702.2008.02695.x
Moriwaki K, Noto S (2017) Economic evaluation of osteoporosis liaison service for secondary fracture prevention in postmenopausal osteoporosis patients with previous hip fracture in Japan. Osteoporos Int 28(2):621–632. https://doi.org/10.1007/s00198-016-3777-2
Myers TA, Briffa NK (2003) Secondary and tertiary prevention in the management of low-trauma fracture. Aust J Physiother 49(1):25–29. https://doi.org/10.1016/S0004-9514(14)60185-9
Nakayama A, Major G, Holliday E, Attia J, Bogduk N (2016) Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int 27(3):873–879. https://doi.org/10.1007/s00198-015-3443-0
Peng LN, Chen WM, Chen CF, Huang CK, Lee WJ, Chen LK (2016) Survival benefits of post-acute care for older patients with hip fractures in Taiwan: a 5-year prospective cohort study. Geriatr Gerontol Int 16(1):28–36. https://doi.org/10.1111/ggi.12429
Sidwell A, Wilkinson T, Hanger H (2004) Secondary prevention of fractures in older people: evaluation of a protocol for the investigation and treatment of osteoporosis. Intern Med J 34(3):129–132. https://doi.org/10.1111/j.1444-0903.2004.00554.x
Suzuki N, Arai K, Kon S, Yamanaka K, Otsuka H, Koizumi M, Hosaka N, Tsuchiya M, Mochizuki T, Kuraishi T, Murayama T, Tashi H, Oike N, Wakasugi M, Takahashi Y, Nakadai M, Endo N (2017) Challenges to prevent secondary fractures in patients with hip fractures in Joetsu Myoko, Japan through the increased use of osteoporosis treatment and collaboration with family doctors. J Bone Miner Metab 35(3):315–323. https://doi.org/10.1007/s00774-016-0758-7
Teede HJ, Jayasuriya IA, Gilfillan CP (2007) Fracture prevention strategies in patients presenting to Australian hospitals with minimal-trauma fractures: a major treatment gap. Intern Med J 37(10):674–679. https://doi.org/10.1111/j.1445-5994.2007.01503.x
Tulk C, Lane P, Gilbey A, Johnston H, Chia K, Mitchell L, Bagga H, Wong PKK (2013) Improving osteoporosis management following minimal trauma fracture in a regional setting: the Coffs Fracture Card Project. Aust J Rural Health. 21(6):343–349. https://doi.org/10.1111/ajr.12072
Vaile J, Sullivan L, Bennett C, Bleasel J (2007) First fracture project: addressing the osteoporosis care gap. Intern Med J 37(10):717–720. https://doi.org/10.1111/j.1445-5994.2007.01496.x
Vaile JH, Sullivan L, Connor D, Bleasel JFA (2013) Year of fractures: a snapshot analysis of the logistics, problems and outcomes of a hospital-based fracture liaison service. Osteoporos Int 24(10):2619–2625. https://doi.org/10.1007/s00198-013-2357-y
Van der Kallen J, Giles M, Cooper K, Gill K, Parker V, Tembo A, Major G, Ross L, Carter J (2014) A fracture prevention service reduces further fractures two years after incident minimal trauma fracture. Int J Rheum Dis 17(2):195–203. https://doi.org/10.1111/1756-185X.12101
Wong PK, Spencer DG, McElduff P, Manolios N, Larcos G, Howe G (2003) Secondary screening for osteoporosis in patients admitted with minimal-trauma fracture to a major teaching hospital. Intern Med J 33(11):505–510. https://doi.org/10.1046/j.1445-5994.2003.00468.x
Yates CJ, Chauchard MA, Liew D, Bucknill A, Wark JD (2015) Bridging the osteoporosis treatment gap: performance and cost-effectiveness of a fracture liaison service. J Clin Densitom 18(2):150–156. https://doi.org/10.1016/j.jocd.2015.01.003
Briot K (2017) Fracture Liaison Services. Curr Opin Rheumatol 29(4):416–21
Rozental TD, Makhni EC, Day CS, Bouxsein ML (2008) Improving evaluation and treatment for osteoporosis following distal radial fractures. A prospective randomized intervention. J Bone Joint Surg Am 90(5):953–61
Bessette L, Davison KS, Jean S, Roy S, Ste-Marie LG, Brown JP (2011) The impact of two educational interventions on osteoporosis diagnosis and treatment after fragility fracture: a population-based randomized controlled trial. Osteoporos Int 22(12):2963–72
Acknowledgments
The authors would like to thank Dr. Zhongyun Zhao for facilitating this research and author collaborations.
Funding
This work was supported by Amgen Inc. Writing and editorial assistance was provided by ApotheCom and funded by Amgen Inc. and grant from NCKUH (NCKUH-10609007, 10605021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Yin-Fan Chang, Chun-Feng Huang, Jawl-Shan Hwang, Jeng-Fu Kuo, Ko-Ming Lin, Hui-Cheng Huang, Ankita Kumar, Fang-Ping Chen, Chih-Hsing Wu declare that they have no conflict of interest.
Shalini Bagga has ownership or partnership in Complete HEOR Solutions LLC.
Electronic supplementary material
ESM 1
(DOCX 113 kb)
Rights and permissions
About this article
Cite this article
Chang, Y.F., Huang, C.F., Hwang, J.S. et al. Fracture liaison services for osteoporosis in the Asia-Pacific region: current unmet needs and systematic literature review. Osteoporos Int 29, 779–792 (2018). https://doi.org/10.1007/s00198-017-4347-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4347-y