Abstract
Post-fracture care (PFC) programs evaluate and manage patients with a minimal trauma or fragility fracture to prevent subsequent fractures. We conducted a literature review to understand current trends in PFC publications, evaluate key characteristics of PFC programs, and assess their clinical effectiveness, geographic variations, and cost-effectiveness. We performed a search for peer-reviewed articles published between January 2003 and December 2020 listed in PubMed or Google Scholar. We categorized identified articles into 4 non-mutually exclusive PFC subtopics based on keywords and abstract content: PFC Types, PFC Effectiveness/Success, PFC Geography, and PFC Economics. The literature search identified 784 eligible articles. Most articles fit into multiple PFC subtopics (PFC Types, 597; PFC Effectiveness/Success, 579; PFC Geography, 255; and PFC Economics, 98). The number of publications describing how PFC programs can improve osteoporosis treatment rates has markedly increased since 2003; however, publication gaps remain, including low numbers of publications from some countries with reported high rates of osteoporosis and/or hip fractures. Fracture liaison services and geriatric/orthogeriatric services were the most common models of PFC programs, and both were shown to be cost-effective. We identified a need to expand and refine PFC programs and to standardize patient identification and reporting on quality improvement measures. Although there is an increasing awareness of the importance of PFC programs, publication gaps remain in most countries. Improvements in established PFC programs and implementation of new PFC programs are still needed to enhance equitable patient care to prevent occurrence of subsequent fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by low bone density and structural deterioration of bone tissue that leads to fractures [1], even with low or minimal trauma experienced upon falling from a standing height or lesser impact. These fractures are commonly referred to as osteoporotic or fragility fractures [2, 3], and include hip, spine (clinical), wrist, humerus, tibia, and pelvic fractures. In 2000, an estimated 9 million fragility fractures occurred worldwide [4]. A more recent study that evaluated fractures at all sites and for all ages, using the framework of the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, reported an estimated 178 million fractures had occurred across 204 countries and territories in 2019, with most of the fractures occurring in the elderly [5]. Fragility fractures are associated with high rates of disability, loss of independence, reduced quality of life for patients and caregivers, and high costs to healthcare systems [3]. Despite the high associated morbidity and mortality, osteoporosis remains underdiagnosed and undertreated [6]. Individuals who experience one fragility fracture are at high risk of experiencing subsequent fractures. Post-fracture care (PFC) programs are systematic, coordinated care programs that identify, evaluate, and manage patients who have sustained a fragility fracture with the goal of preventing further fractures.
PFC programs exist in many forms including fracture liaison services (FLSs; also known as secondary fracture prevention [SFP]) programs [7], geriatric/orthogeriatric services (OGSs; also known as geriatric fracture centers [GFCs]) [8], and osteoporosis liaison services (OLSs) (Table 1). These programs vary in terms of personnel (lead or coordinator), fracture sites identified (hip vs. other fracture types), clinical setting (inpatient or outpatient), and scope of services offered (patient identification, investigation, or intervention) (Table 1). The two main models of PFC programs are outpatient FLSs and inpatient OGSs. The primary goal of FLSs is to prevent subsequent fragility fractures [7] and the primary goal of OGSs is to improve overall outcomes (morbidity, mortality, and/or physical function) for inpatients in the programs [8]. In general, FLSs and OGSs have some fundamental differences, such as outpatient and post-discharge care for FLSs vs. care for patients admitted to a hospital due to mostly hip fractures under OGSs (Table 1); however, these distinctions are not as clear cut in practice, with some programs incorporating elements of both models [9,10,11,12], though FLSs are more commonly applied to address outpatient care while in some situations, OGSs manage all inpatient care in addition to post-fracture care after patient discharge (Table 1). Also, in some countries, OGSs manage all hip fractures and FLSs manage secondary prevention for all other fragility fractures (Table 1).
Over the last few years, there has been a marked increase in the number of publications describing how PFC programs can improve identification, diagnosis, and treatment for patients with osteoporosis. In this article, we report results from a literature search and review we conducted to provide a cross-sectional snapshot of the global landscape of PFC programs. The key objectives were to understand trends in publications about PFC programs over the years; evaluate key characteristics of FLSs and OGSs; assess clinical effectiveness, geographic variations, and cost-effectiveness of PFC programs; and identify barriers and solutions to implementation of PFC programs.
Methods
Literature search parameters
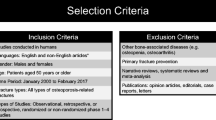
We performed a search for peer-reviewed articles published between January 2003 and December 2020 that are listed in PubMed or Google Scholar using the literature search terms shown in Table 2. Publications eligible for assessment in this analysis included original research articles, reviews, guidelines/recommendations, case studies, editorials, and letters to the editor published between January 2003 and December 2020; abstracts and congress proceedings were not eligible for assessment in this analysis. While most of the publications assessed were English language publications, a few articles written in other languages were included as long as an English language abstract was available. One author, in consultation with the other authors, assessed all retrieved articles for relevance to PFC programs. We included review articles, editorials, and letters to the editor in the assessment only if they contained new insights not covered in original research articles. Cases of ambiguity with regard to relevance to PFC programs were adjudicated through author discussions.
PFC program subtopics
We categorized the identified relevant articles into 1 of 4 pre-selected non-mutually exclusive PFC program subtopics based on assessment of keywords and abstract content. The selected subtopics were PFC Types, PFC Effectiveness/Success, PFC Geography, and PFC Economics (Table 3).
Outcomes
We reviewed articles that met the eligibility criteria for this analysis and evaluated trends in peer-reviewed articles on PFC programs between January 2003 and December 2020; identified and evaluated key characteristics of FLSs and OGSs; and assessed clinical effectiveness, geographic variations, and economics of PFC programs. We also highlighted barriers and solutions to implementation of PFC programs.
Results
Search results
Our search for peer-reviewed articles with relevance to PFC programs published between January 2003 and December 2020 and listed in PubMed or Google Scholar identified 784 unique articles that met the search criteria, with 746 of these articles listed in PubMed. The 784 articles included 638 original research articles, 81 reviews, 29 guidelines/recommendations, 22 case studies, 10 editorials, and 4 letters to the editor.
The number of publications per year increased from 2003 to 2020 (Fig. 1). Of the journals with ≥ 10 publications on PFC programs from January 2003 to December 2020, Osteoporosis International had the highest number with 152 articles (Online Resource Table 1). The most cited articles from January 2003 to December 2020 (Online Resource Table 2) reflect an interest in mostly hip fracture programs or OGSs; however, the most cited publications in the past 5 years (January 2015 to December 2020) reflect an interest in both FLSs and hip fracture/OGS programs (Online Resource Table 3).
Number of identified peer-reviewed articles with relevance to PFC programs published by publication year. Eligible articles were peer-reviewed original research articles, reviews, and commentaries of English language articles with relevance to PFC programs published between January 2003 and December 2020 and listed in PubMed or Google Scholar
Based on assessment of keywords and abstract content, most of the 784 articles were categorized into multiple PFC program subtopics (Fig. 2a, b), with 597 articles in PFC Types, 579 in PFC Effectiveness/Success, 255 in PFC Geography, and 98 in PFC Economics. Some articles fit into 1 subtopic only (Fig. 2b): 96 in PFC Types, 66 in PFC Effectiveness/Success, 20 in PFC Geography, and 7 in PFC Economics. However, 17 of the 784 articles did not fit into any of the pre-selected subtopics; most of these were descriptive studies.
Identified peer-reviewed articles with relevance to PFC programs published between January 2003 and December 2020 by selected PFC program subtopic (a) and fit into program subtopic (b). Articles were categorized into 1 of 4 pre-selected non-mutually exclusive PFC program subtopics as defined in Table 3 based on assessment of keywords and abstract content. Some articles fit into multiple subtopics; however, 17 of 784 articles did not fit into any of the subtopics (particularly articles on descriptive studies). FLS, fracture liaison service; OGS, orthogeriatric service; PFC, post-fracture care
Program types, scale, and target patient populations
Most articles were on FLSs and OGSs, which are the two primary models of PFC programs. FLSs have historically been focused on all types of fragility fractures (including hip, spine [clinical], wrist, and humerus) with the primary goal of preventing subsequent fragility fractures (Fig. 3a). OGSs mainly focus on hip fractures with the primary goal of improving overall patient outcomes, including peri-operative morbidity, mortality, and physical function (Fig. 3b). FLSs and OGSs have notable functional differences and similarities [7, 8] (Fig. 3). Patient identification in FLSs is mainly through chart review and electronic medical record (EMR) notifications for any fragility fracture type, generally in patients ≥ 50 years of age. Patient identification in OGSs is through hospital admission, often limited to patients with hip fractures, although patients with other fracture types may also be included. Because OGSs enroll hospitalized patients, they also offer pre-surgical management of patients, including patient assessment, comorbidity management, and coordination of consultations and testing to reduce time to surgery. Both FLSs and OGSs offer fracture risk assessment; this is part of routine evaluation in FLSs and part of post-surgical management in OGSs. The methods of fracture risk assessment are similar and include bone mineral density (BMD) testing, spine imaging, review of parental history of fractures, use of fracture risk assessment tools/algorithms, blood tests, and biomarker profiling. Most FLSs have an intervention step that includes prescribing osteoporosis medication, diet, exercise, and fall prevention education. OGSs have a rehabilitation step that includes inpatient or outpatient physical therapy and fall prevention education. Patient follow-up methods are similar for FLSs and OGSs and include clinic visits, virtual care (medical consultations through video calls, phone calls, emails, and text messaging), and visits to primary care practitioners.
Functions of PFC programs: FLS (a) and OGS (b). Blue font text denotes the common steps in both FLS and OGS programs. aMedical consultations through video calls, phone calls, emails, and text messaging. BMD, bone mineral density; EMR, electronic medical records, PCP, primary care physician; PT, physical therapy
PFC programs that lack the basic elements of FLSs and OGSs but still support improvements in patient care were also identified. These include independent fracture registries [13, 14]; software applications supporting FLS/OGS workflows and automated patient identification [15, 16]; remote education/mentoring of healthcare professionals (HCPs) [17]; EMR prompts for screening/treatment [18, 19]; education/targeted advice for HCPs only [20, 21]; and prompts to HCPs and patients with no targeted education or specific recommendations [22,23,24]. This article focuses on FLSs and OGSs only.
Publications on PFC programs by subtopic
PFC types
PFC-related publications continue to mention both FLSs and OGSs, with an increasing focus on treatment of elderly patients in recent years. We identified articles reporting on FLSs for the prevention of subsequent fragility fractures as well as diagnosis and management of vertebral fractures. We also identified articles on OGSs reporting peri-operative outcomes with limited reporting on osteoporosis management; however, there is a growing trend of PFC programs that combine elements of FLSs and OGSs [10,11,12, 25,26,27,28,29,30,31,32,33,34,35,36,37,38], resulting in increased rates of osteoporosis diagnosis and improved patient outcomes. We identified reports of FLS management of hip fractures [10, 32,33,34,35] and reports of orthogeriatric management of non-hip fractures [11, 31, 36]. With regard to diagnostic methods, additional screening and diagnostic tests for determining fracture risk and bone strength, including biomechanical computed tomography and determination of trabecular bone score, are being investigated for their utility in FLSs [39] and new scoring and risk identification systems are being incorporated to predict orthogeriatric outcomes [11, 30, 31].
FLSs can be classified by the intensity of care provided (Types A–D) or the number of interventions provided (0i–3i) [7, 40] (Table 4). Type A FLSs involve identification, intervention, and initiation of therapy; Type B involve identification and intervention; Type C involve identification with anticipation of primary care to intervene and initiate therapy; and Type D involve providing patient education only [40]. Type A and Type B FLSs typically involve a dedicated coordinator. A meta-analysis of data from reports published between 1996 and 2011 demonstrated that more intensive intervention types led to better outcomes in terms of investigation and treatment initiation [40, 41]. Most FLSs are Type A/Type B, and there is a general consensus that Type A FLSs are the most effective. Although Type A FLSs focus on treatment initiation, there were also Type A FLSs that reported on follow-up of patients and adherence to medications [42, 43] (Table 4). Very few Type C and Type D FLSs were identified (Table 4). Additionally, some virtual PFC/virtual care/cloud technologies have been developed and these vary from video conferencing to remote monitoring of patients with fragility fractures using sensors [15, 44,45,46,47] (Online Resource Table 4).
PFC effectiveness/success
Quality improvement measures for PFC programs
Reports on quality improvement measures for a variety of PFC programs were identified, with recent meta-analyses published [48, 49]. For the most part, program goals, patient populations, and resources often differ among PFC programs [50,51,52,53]. Additionally, the clinical or health outcomes used to assess the success or effectiveness of PFC programs vary according to intervention type and from program to program, even for similar interventions [50,51,52]. However, there are some indications that the field is moving toward harmonization of quality improvement measures [13, 51, 52, 54, 55]. These quality improvement measures vary widely with many involving identification and diagnosis, others involving process, and a few involving clinically relevant long-term outcomes including mortality and rates of readmission (Fig. 4). The recent article by Javaid et al 2020 [52] reported on 11 patient-level key performance indicators (KPIs) that could be evaluated in outpatient FLSs as identified by the International Osteoporosis Foundation (IOF)’s Capture the Fracture® Campaign together with the Fragility Fracture Network (FFN) and the Bone Health and Osteoporosis Foundation (BHOF, formerly known as the National Osteoporosis Foundation [NOF]) (Fig. 4). These KPIs have been incorporated into clinical standards across regions [56,57,58,59] that are being used together with other resources to enable real-time benchmarking of the performance of FLSs. Other PFC programs that reported on KPIs include the Medicare/Medicaid program [51], the American Orthopaedic Association’s (AOA’s) Own the Bone program [13], the hospital-based Dutch Hip Fracture Audit program [54], and the hospital-based orthogeriatric program [55] (Fig. 4).
Signals of harmonized quality improvement measures. BMD, bone mineral density; DXA, dual-energy X-ray absorptiometry; FFN, Fragile Fracture Network; HCP, healthcare professional; FLS, fracture liaison service; IOF, International Osteoporosis Foundation; BHOF, National Osteoporosis Foundation; PFC, post-fracture care
Of note, recent studies are now advocating the use of vertebral fracture assessments (VFAs) using spine X-ray or dual-energy X-ray absorptiometry (DXA) to identify patients with previously unidentified vertebral fractures [60,61,62]. The usefulness of systematic VFA was demonstrated in an FLS conducted in patients ≥ 50 years of age in which vertebral fractures that had been unknown before were identified by VFA in 21% of patients (24 of 114 patients) [60]. A total of 18 of the 24 patients had adaptation of osteoporosis medication (16 were initiated on osteoporosis medication and 2 had osteoporosis medications intensified) because of the VFA outcome vs. 6 patients who would have received osteoporosis medication in the absence of VFA (66.7 vs. 33.3%, P < 0.001) [60]. In another analysis, data from the Manitoba Bone Density Program database prospective observational cohort demonstrated that targeted VFA in postmenopausal women and older men substantially improved identification of patients at high risk for fracture and was strongly associated with subsequent use of fracture prevention medication [61, 62]. The BHOF [63] and International Society for Clinical Densitometry (ISCD) [64] have both issued guidelines recommending the targeted use of VFA at the time of bone densitometry to identify patients with clinically unrecognized vertebral fracture who can be considered candidates for osteoporosis medications to prevent subsequent fragility fractures. VFA can potentially be included as an additional quality improvement measure to increase identification and treatment of patients.
Other strategies to enhance quality improvement measures of PFC programs are also being considered. These include implementation of registries, educational programs for HCPs, and new osteoporosis guidance for different medical specialties such as orthopedic surgeons and non-physicians such as nurses, physiotherapists, and nutritionists.
Comparison of FLSs and OGSs
Few articles report direct comparisons between FLSs and OGSs. In a hip fracture study conducted from 2003 to 2013 at 11 hospitals in England with either FLSs or OGSs [65], both intervention types had similar reductions in 1-year mortality but no significant difference on time to a second hip fracture. In a comparison of an inpatient OGS with no outpatient follow-up vs. an inpatient OGS with an added FLS including outpatient follow-up [10], the proportion of patients on bisphosphonates was 8 vs. 10% at admission; 8 vs. 96% at discharge; and 15 vs. 75% at 6 months after discharge. Patients in the FLS could be followed-up after discharge to record adherence to treatment; most (77%) adhered to treatment at 6 months [10].
Combining FLS and OGS approaches
Combining FLS and OGS approaches into a new type of program model is an emerging trend, and such programs have reported a 2- to 5-fold improvement in outcomes, including an improvement in program enrollment, osteoporosis testing and diagnosis, and initiation of osteoporosis therapy for hip fracture patients in particular [10,11,12, 25, 27,28,29, 38]. Implementation of standard orders to enroll patients who were in a geriatric hip fracture program increased FLS participation from 75 to 85.6% [12]. FLS within a hip fracture program increased rate of osteoporosis evaluation during hospitalization (0.6 to 72.6%; P < 0.001) and initiation of osteoporosis therapy within 3 months of discharge (25.3 to 46.3%; P = 0.01) [38]. In addition, an FLS-like fracture prevention service identifying hip fracture patients while still in hospital increased BMD testing from 14.5 to 47.6% and osteoporosis therapy from 17.2 to 48.5% [29]. For patients admitted to a geriatric fracture center, FLS led to a high rate of specific recommendations for osteoporosis therapy (68.6%) [25]. FLS for hip fractures with the first visit occurring in hospital increased initiation of osteoporosis therapy from 20.9 to 59.6% [27]. Adding FLS functions to a hip fracture service increased osteoporosis therapy rate from 32 to 81% [28]. Integration of an FLS with an OGS hip fracture program increased initiation of osteoporosis therapy compared with standard of care (75 vs. 15%) [10]. Integration of FLS with OGS increased basic osteoporosis therapy to 65 vs. 18% before hospitalization [11].
Initiation of osteoporosis treatment
Although many hip fracture/OGS programs still do not prescribe osteoporosis therapies, those that do often prescribe the recommended osteoporosis medications for hospitalized elderly patients, including bisphosphonates (alendronate, ibandronate, risedronate, or zoledronic acid), denosumab, and teriparatide [26, 28, 66,67,68]. One study reported an FLS for hip fractures that started osteoporosis therapy in patients who were still hospitalized, with new initiations of osteoporosis therapy of 24.7% before FLS implementation increasing to 43.9% after FLS implementation (P < 0.001) [26]. Similarly, the use of an electronic order set on the day of hospital discharge improved rates of timely osteoporosis treatment following hip fracture (32 vs. 81%) [28]. A treatment algorithm for the management of osteoporosis in elderly patients during the post-operative stay in a trauma surgical ward has also been developed [66], calling for inpatient initiation of treatment with oral bisphosphonates, intravenous bisphosphonates, denosumab when bisphosphonates are contraindicated, or teriparatide if osteoporosis is severe (e.g., when vertebral body fractures occur while patient is on oral antiresorptives). Recent studies have investigated administration of zoledronic acid pre- or post-surgery in patients with vertebral compression or hip fractures [67, 68]. In general, orthogeriatric/geriatric inpatients often receive prescriptions for osteoporosis medications or FLS referrals at discharge; however, it is important to note that initiation of osteoporosis medication to inpatients may be contraindicated for several reasons, including comorbidities and vitamin D or calcium deficiency [66]. In addition, factors such as risk vs. benefit, patient adherence, and cost of medications need to be considered when making decisions for each medication [66].
Treatment adherence
In general, most articles reporting on PFC quality improvement measures still do not report data on treatment adherence to osteoporosis therapy. For those that do, there is evidence of heterogeneity in most reports with regard to patient populations, timepoints for assessments, sample sizes, and program designs when evaluating adherence (Table 5). Generally, there is lower adherence to osteoporosis therapy in orthogeriatric/geriatric fracture patients, with little or no adherence reporting for OGSs with no FLS functions. Most osteoporosis treatments show anti-fracture efficacy between 12 and 18 months for vertebral fractures. As such, monitoring adherence to osteoporosis therapy at 3, 6, or 9 months may best serve as an interim KPI for vertebral fractures but adherence at ≥ 12 months would be preferred.
Impact of COVID-19 on PFC
Thirteen articles reported on COVID-19 in the context of PFC programs with some articles reporting on process adaptations that could facilitate PFC during the pandemic, while others reported on the specific impact of COVID-19 on PFC delivery. Details of identified studies are provided in Online Resource 1, under the subheading of Studies on Impact of COVID-19 on PFC.
PFC geography
Adoption of PFC programs has been occurring in previously unserved regions and countries, and expansion of PFC availability has also been reported in regions and countries with established PFC programs (Table 6). There have been some reports of new PFC programs since 2019, with a recent trend toward more expansion of OGS. New reports have been published on hip fracture programs in several countries including mainland China, Israel, South Africa, and the USA; on FLSs in several countries including South Korea, Thailand, Canada, and Germany; and on treatment rates or disease burden in several countries including Japan, mainland China, Denmark, and the UK (Table 6). However, some countries with a high osteoporosis incidence produced few or no PFC publications over the period studied (Table 6). It is noteworthy to acknowledge that lack of publications may not necessarily reflect an ongoing global osteoporosis care gap; however, this might reflect the low awareness of the need for osteoporosis care programs even in developed countries with established PFC programs.
Open questions still remain in most geographic regions, especially with regard to the impact of healthcare system types that tend to vary from country to country (i.e., open or closed, public or private). Additionally, in countries with less developed healthcare infrastructure, long distances to a clinic or health facility may result in patients being lost to follow-up [69], hence diminishing the effectiveness of PFC care. More information on virtual care is required, especially with respect to the COVID-19 pandemic and its impact on rates of follow-up and treatment patterns.
PFC economics
There has been an increase in publications reporting on PFC economics since 2017. PFC programs are generally cost-effective, but there is a high degree of variability in cost-effectiveness given the heterogeneity in resourcing, PFC structures, and outcomes being measured. We identified reports that compared costs of FLSs with costs of standard of care [27, 70], costs between different FLSs [71], costs of OGS/hip fracture programs vs. standard of care [72], reimbursement related to PFC programs [72,73,74], and socioeconomic status and financial considerations [75, 76]. Details of the identified studies are provided in Online Results 1, under the subheading of Studies on PFC Economics.
Overall, most identified articles demonstrated that PFC programs were generally cost-effective and reduced the economic cost of subsequent fragility fractures for both the individual and the society. Of note, the identified publications reported economic outcomes differently. As such, comparisons may need to focus on cost savings per patient. Most articles factored in only direct costs in assessing the economic cost of subsequent fragility fractures; indirect costs such as lost productivity were not factored in cost assessments even though they can be quite substantial.
Barriers to PFC
A few articles have reported on challenges hindering provision of adequate care to patients to prevent subsequent fractures. Barriers include significant increase of workload to healthcare systems [77], inability by HCPs to identify patients at risk and follow-up with appropriate referrals [78], failure by patients to follow-up on scheduled tests such as DXA scans [79], and patients’ perspectives on the need for osteoporosis medications [80].
In our view, the main barrier to secondary fracture prevention is likely the lack of adequate information on the part of population healthcare decision-makers, HCPs, and patients on the nature of osteoporosis as an underlying chronic disease that puts patients at risk for fragility fractures and that can be costly to patients, to their caregivers, and to society at large. Population health decision-makers are often unaware of the impact of fragility fractures, and yet are usually involved in evaluating the business case for establishing PFC programs. HCPs may not assess, diagnose, and treat patients at risk for osteoporosis and fragility fracture due to numerous reasons including time constraints, insufficient knowledge, competing priorities, doubts about effectiveness of osteoporosis treatments, and fear of adverse events. At the service provider level, the lack of knowledge might be reflected in poor patient identification, lack of adequate provider communications regarding patient care, inadequate record keeping/data management/electronic notifications, and poor quality control. Therefore, HCPs may not recognize fragility fractures, assess osteoporosis risk, and prescribe treatment in situations that may warrant it. At the patient level, patients may not feel the need to follow-up with their HCPs regarding osteoporosis care following a primary fracture due to a lack of clarity around what actions to take or denial that occurrence of a primary fracture puts them at increased risk of subsequent fractures. Patients may also be unwilling or have limited ability to participate in PFC programs due to the time required for follow-up visits, out-of-pocket expenses, and frailty.
Facilitating adoption and implementation of PFC programs
Establishment of new PFC programs is required, including expansion to rural and remote areas, to enhance equity of care for patients with osteoporosis. Many medical societies offer educational resources and counsel to help providers establish PFC programs. These include the IOF Capture the Fracture, the IOF PFC resource center, BHOF FLS resources, BHOF FLS coding guide, AOA’s Own the Bone, American Geriatrics Society (AGS)’s CoCare model, and the FFN Clinical and Policy Toolkits. There is an opportunity to develop clinical guidelines that recommend specific actions and frameworks for different models of care and also provide education to HCPs, including e-learning. Another strategy is to motivate providers through cultivating local champions, providing financial incentives, and tracking and publishing performance data. An additional way is through coordination of efforts across fracture coordinators, including sharing of best practices through collaboration platforms such as the Extension for Community Healthcare Outcomes (ECHO), and cooperation among multiple specialties. For rural or remote regions with low population densities or limited resources, adoption of remote digital programs and models that require fewer staff might aid in the establishment of PFC programs.
Sustainability of programs, especially after a PFC provider champion departs, is a recognized challenge. Hence, PFC programs need to be an integral part of healthcare systems, with the PFC protocols or program framework deeply embedded into the hospital/clinic practice (e.g., updating EHR practices and establishing a protocol for ensuring connectivity across providers). This will help to make these programs champion independent, to ensure long-term sustainability.
Summary
There is an increasing awareness of the importance of PFC programs in overall patient care, with the number of PFC-related publications increasing yearly from 2003 to 2020. However, a publication gap still remains in several countries, including those countries with a reported high incidence of fragility and/or hip fractures. Factors contributing to the observed publication gap may be a reflection of priorities and/or limited resources of institutions and research groups. These factors are likely impacted by geography and socioeconomic status but further research is required to provide more information.
From our literature search and assessment of the available PFC-related publications, we found that continued implementation of FLS and OGS programs is important in managing osteoporosis, with programs that combine both FLS and OGS functions becoming more common [10,11,12, 25,26,27,28,29,30,31,32,33,34,35,36,37,38]. Combining FLS and OGS approaches appears to result in about 2- to 5-times improvement in outcome measures such as program enrollment, osteoporosis testing and diagnosis, and initiation of osteoporosis therapy [10,11,12, 25,26,27,28,29, 38]. Success of these programs requires ongoing research into quality improvement measures and best practices, new treatment approaches, and expansion of programs to include elderly patients, different fracture types, and patients with comorbidities. Articles on orthogeriatric and hip fracture care still have a stronger focus on survival and comorbidities rather than on refracture rates. It appears there is a trend toward the treatment of elderly patients and in the diagnosis and treatment of vertebral fractures [81]. Recent publications suggest that once PFC programs are established, there is a desire to expand and refine their practices as well as to optimize cost-effectiveness.
The success and effectiveness of PFC programs is well documented; however, areas for improvement still exist. In general, there is inconsistent reporting of clinical or health outcomes, even for similar interventions; program goals, patient populations, and resources are often different among PFC programs [50,51,52,53]. Patient adherence to osteoporosis medications varies, with interventions that include prescribing osteoporosis medications often showing improved patient outcomes but not to optimal levels. Inconsistent reporting of quality improvement measures is still a key challenge, but there is now evidence of some efforts at harmonizing quality improvement measures for PFC programs [13, 51, 52, 54, 55].
Other factors that could contribute to successful PFC programs have been identified including implementation of registries, educational programs, and continuous updates of osteoporosis guidance for HCPs. The AOA’s Own the Bone program [13] is a multicenter voluntary fragility US registry created in 2009 and functions as an externally validated cohort for studying fragility fractures in patients. The program has been used to define quality improvement measures [13] and is credited with successfully improving the behaviors of medical professionals with regard to osteoporosis treatment and managing patients with fragility fractures [82]. An independent registry [14] showed an increase in identification of patients with fractures who are ≥ 50 years from 0 to 74.5% as a result of registry implementation, with 33.9% of those identified patients proceeding to have screenings and follow-up visits. Additionally, the Hip Fracture Registry Toolbox [83] provides a distillation of information from existing national registries and practical advice on starting new registries.
For the educational programs, the Bone Health Extension for Community Healthcare Outcomes (TeleECHO) was established in the USA to use video conferencing technology to provide education on the care of patients with skeletal diseases to HCPs in communities, including those in rural and underserved areas [17]. The TeleECHO initiative has been used by US- and international-based HCPs and is a model that could be replicated to include the education of FLS coordinators and other HCPs to expand the pool of specialists who can provide bone healthcare to patients [17]. A number of organizations across the globe are now hosting Bone Health TeleECHO programs including the BHOF and the AOA.
For osteoporosis therapy, there is variability in treatment approaches across PFC programs; however, many emerging guidelines would consider individuals with a recent fracture or history of multiple fractures to be at very high risk for future fracture and appropriate for treatment with an anabolic agent [84,85,86,87]. Anabolic therapy should be followed by antiresorptive therapy to preserve BMD gains obtained while on an anabolic, and reassessment is recommended every 1 to 2 years [85] or after a fracture [86].
Reports have been published on the impact of COVID-19 on PFC delivery [88]. Of note, there is an opportunity to take lessons learned during the COVID-19 pandemic and implement them to patient care, particularly in rural or remote areas with limited access to patient care. This could include increased use of telemedicine and virtual technology.
With regard to geographic variation, there is evidence that PFC programs continue to expand into new and underserved regions and countries, and also to increase in countries with established PFC programs. The trend seems to be toward OGS programs. There is still a care gap even in developed countries with established PFC programs. Issues of consideration in different regions include the impact of healthcare system types and proximity to clinics or healthcare facilities, especially in countries with less developed healthcare infrastructure.
There has been an increase in reports on the economics of PFC programs since 2017, and these show that PFC programs are cost-effective [49, 70, 72]. High-intensity interventions such as Type A FLSs are more costly but are generally cost-effective or even cost-saving [27, 71]. There is evidence that reimbursement may be a bigger driver of funding decisions than quality of care [72, 73]; only 1 study from Japan showed no reduction in healthcare resource utilization linked to financial incentives for regionally coordinated hip care [74]. Data are available comparing PFC programs to standard of care [49, 70, 72], with only limited data comparing economics of FLSs and OGSs. New data on PFC implementation or maintenance costs are not readily available, limiting the ability to properly evaluate costs associated with these programs. There is still inconsistent reporting of economic outcomes. Not all studies report incremental cost-effectiveness ratios or quality-adjusted life-years, and it may be more helpful to focus on cost or cost savings per patient. In assessing the economic cost of subsequent fragility fractures, most articles do not factor in indirect costs such as lost productivity, even though these costs are generally considered substantial.
Lack of information is the main barrier to prevention of subsequent fracture, and this can be addressed by educating population healthcare decision-makers, HCPs, and patients to understand the personal and societal burden of osteoporosis. Adoption and implementation of PFC programs can be facilitated through various resources from key organizations including the IOF, BHOF, AOA, and AGS. Sustainability of PFC programs can be achieved by integrating processes into hospital and clinic practices.
Of all the information garnered from the literature search and assessment of publications on PFC programs, we believe combining FLS and OGS approaches together with development of fragility fracture registries to provide ongoing research to advance KPIs could improve the effects of PFC programs the most. Combining FLS and OGS approaches has been shown to result in improvement in outcome measures such as program enrollment, osteoporosis testing and diagnosis, and initiation of osteoporosis therapy. The ongoing research from the combined FLS/OGS programs and/or the fragility fracture registries could inform new strategies for improving quality improvement measures and best practices, incorporating new treatment approaches, and expanding programs to include elderly patients, different fracture types, and patients with comorbidities. Additionally, we believe that high-level policy change, requiring secondary fracture prevention to be an integral part of standard patient care, could facilitate financial support including reimbursement and personnel for implementation of more of these important programs.
The main strength of our literature search and assessment is that it provides a cross-sectional snapshot of the global landscape of PFC programs. However, a number of limitations should be considered. First, the main focus of PFC programs is patient care and most settings may not view publishing quality improvement measures of these programs as valuable; thus, findings from our literature search may not fully represent the available knowledge and progress on PFC programs to date. Second, since the literature search was based on relevance to PFC programs, there may be some bias in that all authors publishing may have already convinced their healthcare centers that fracture risk is an issue worth identifying, evaluating, and managing; however, a significant proportion of health centers may still not view fracture risk as an issue and may not allocate resources to fracture prevention, thus leaving patients at risk for new fractures. Third, to date, most FLSs and OGSs focus on the elderly in hospital settings; there is limited information on programs for younger patients with fractures or elderly patients in assisted-living facilities who experience fractures.
In conclusion, there has been a marked increase in the number of publications describing how PFC programs can improve investigation and treatment rates for osteoporosis. However, there is a publication gap in several countries including those countries with a reported high incidence of fragility and/or hip fractures. The most common models of PFC programs are FLSs and OGSs, and these have been shown to be cost-effective. Improvements in established PFC programs are still needed to standardize patient identification and outcomes reporting. Additionally, establishment of new PFC programs is required, including expansion to rural and remote areas, to enhance equity of care for patients with fracture and osteoporosis, to prevent occurrence of subsequent fractures.
Data availability
Qualified researchers may request data from Amgen clinical studies. Complete details are available at the following: https://wwwext.amgen.com/science/clinical-trials/clinical-data-transparency-practices/clinical-trial-data-sharing-request/.
Code availability
Not applicable.
References
International Osteoporosis Foundation. About osteoporosis. Available at: https://www.osteoporosis.foundation/health-professionals/about-osteoporosis. Accessed 24 January 2022.
National Institute of Health (2001) Osteoporosis prevention, diagnosis, and therapy. NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. JAMA 285:785–795
International Osteoporosis Foundation. Facts and statistics. Epidemiology of osteoporosis and fragility fractures. Available at: https://www.osteoporosis.foundation/facts-statistics/epidemiology-of-osteoporosis-and-fragility-fractures. Accessed 24 January 2022.
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
GBD 2019 Fracture Collaborators (2021) Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev 2:e580–e592
Lewiecki EM, Ortendahl JD, Vanderpuye-Orgle J, Grauer A, Arellano J, Lemay J, Harmon AL, Broder MS, Singer AJ (2019) Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR Plus 3:e10192
Ganda K, Mitchell PJ, Seibel MJ (2019) Models of secondary fracture prevention. In: Siebel MJ, Mitchell PJ (eds) Secondary fracture prevention: an international perspective. Academic Press, London, pp 33–62
Grigoryan KV, Javedan H, Rudolph JL (2014) Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28:e49–e55
Schweser KM, Crist BD, Nguyen VH (2017) Combined orthogeriatric and fracture liaison service for improved postfracture patient care. Osteoporos Sarcopenia 3:159
Naranjo A, Fernández-Conde S, Ojeda S, Torres-Hernández L, Hernández-Carballo C, Bernardos I, Rodríguez S, Laynez P (2017) Preventing future fractures: effectiveness of an orthogeriatric fracture liaison service compared to an outpatient fracture liaison service and the standard management in patients with hip fracture. Arch Osteoporos 12:112
Schray D, Neuerburg C, Stein J, Gosch M, Schieker M, Böcker W, Kammerlander C (2016) Value of a coordinated management of osteoporosis via fracture liaison service for the treatment of orthogeriatric patients. Eur J Trauma Emerg Surg 42:559–564
Borade A, Kempegowda H, Tawari A, Suk M, Horwitz DS (2016) Improvement in osteoporosis detection in a fracture liaison service with integration of a geriatric hip fracture care program. Injury 47:2755–2759
Carlson BC, Robinson WA, Wanderman NR, Nassr AN, Huddleston PM 3rd, Yaszemski MJ, Currier BL, Jeray KJ, Kirk KL, Bunta AD, Murphy S, Patel B, Watkins CM, Sietsema DL, Edwards BJ, Tosi LL, Anderson PA, Freedman BA (2018) The American Orthopaedic Association's Own the Bone® database: a national quality improvement project for the treatment of bone health in fragility fracture patients. Osteoporos Int 29:2101–2109
Mackey PA, Rosenthal LD, Mi L, Whitaker MD (2019) Subsequent fracture prevention in patients 50 years and older with fragility fractures: a quality improvement initiative. J Healthc Qual 41:17–22
Holzmueller CG, Karp S, Zeldow D, Lee DB, Thompson DA (2016) Development of a cloud-based application for the fracture liaison service model of care. Osteoporos Int 27:683–690
Gupta MJ, Shah S, Peterson S, Baim S (2018) Rush Fracture Liaison Service for capturing “missed opportunities” to treat osteoporosis in patients with fragility fractures. Osteoporos Int 29:1861–1874
Lewiecki EM, Rochelle R, Bouchonville MF 2nd, Chafey DH, Olenginski TP, Arora S (2017) Leveraging scarce resources with Bone Health TeleECHO to improve the care of osteoporosis. J Endocr Soc 1:1428–1434
Feldstein A, Elmer PJ, Smith DH, Herson M, Orwoll E, Chen C, Aickin M, Swain MC (2006) Electronic medical record reminder improves osteoporosis management after a fracture: a randomized, controlled trial. J Am Geriatr Soc 54:450–457
Baim S (2017) The future of fracture risk assessment in the management of osteoporosis. J Clin Densitom 20:451–457
Rothman MS, Olenginski TP, Stanciu I, Krohn K, Lewiecki EM (2019) Lessons learned with Bone Health TeleECHO: making treatment decisions when guidelines conflict. Osteoporos Int 30:2401–2406
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C, IOF Fracture Working Group (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Clark EM, Gould V, Morrison L, Ades AE, Dieppe P, Tobias JH (2012) Randomized controlled trial of a primary care-based screening program to identify older women with prevalent osteoporotic vertebral fractures: cohort for Skeletal Health in Bristol and Avon (COSHIBA). J Bone Miner Res 27:664–671
Edwards BJ, Bunta AD, Anderson J, Bobb A, Hahr A, O'Leary KJ, Agulnek A, Andruszyn L, Cameron KA, May M, Kazmers NH, Dillon N, Baker DW, Williams MV (2012) Development of an electronic medical record based intervention to improve medical care of osteoporosis. Osteoporos Int 23:2489–2498
O'Brien LK, Armstrong AD, Hassenbein SE, Fox EJ (2015) Evaluation of patients' response toward osteoporosis letter intervention versus phone call plus letter intervention. Geriatr Orthop Surg Rehabil 6:246–250
Gosch M, Bail H-J, Grueninger S, Stumpf U, Kammerlander C, Wicklein S (2020) What is a reasonable rate for specific osteoporosis drug therapy in older fragility fracture patients? Arch Osteoporos 15:20
Beaupre LA, Moradi F, Khong H, Smith C, Evens L, Hanson HM, Juby AG, Kivi P, Majumdar SR, STOP-Fracture Team (2020) Implementation of an in-patient hip fracture liaison services to improve initiation of osteoporosis medication use within 1-year of hip fracture: a population-based time series analysis using the RE-AIM framework. Arch Osteoporos 15:83
Beaupre LA, Lier D, Smith C, Evens L, Hanson HM, Juby AG, Kivi P, Majumdar SR, STOP-Fracture Team (2020) A 3i hip fracture liaison service with nurse and physician co-management is cost-effective when implemented as a standard clinical program. Arch Osteoporos 15:113
Kuiper BW, Graybill S, Tate JM, Kaufman N, Bersabe D (2018) After the fall: improving osteoporosis treatment following hip fracture. Osteoporos Int 29:1295–1301
Ruggiero C, Zampi E, Rinonapoli G, Baroni M, Serra R, Zengarini E, Baglioni G, Duranti G, Ercolani S, Conti F, Caraffa A, Mecocci P, Brandi ML (2015) Fracture prevention service to bridge the osteoporosis care gap. Clin Interv Aging 10:1035–1042
Abrahamsen C, Nørgaard B, Draborg E, Nielsen MF (2019) The impact of an orthogeriatric intervention in patients with fragility fractures: a cohort study. BMC Geriatr 19:268
Ong T, Sahota O, Gladman JRF (2020) The Nottingham Spinal Health (NoSH) Study: a cohort study of patients hospitalised with vertebral fragility fractures. Osteoporos Int 31:363–370
González-Quevedo D, Bautista-Enrique D, Pérez-del-Río V, Bravo-Bardají M, García-de-Quevedo D, Tamimi I (2020) Fracture liaison service and mortality in elderly hip fracture patients: a prospective cohort study. Osteoporos Int 31:77–84
Wozniak LA, Beaupre LA, Juby A, Kivi P, Majumdar SR, Hanson HM (2020) Successful implementation of a fracture liaison service through effective change management: a qualitative study. Arch Osteoporos 15:44
Naranjo A, Molina A, Sepúlveda C, Rubiño FJ, Martín N, Ojeda S (2020) The evolution of an FLS in search of excellence: the experience of Gran Canaria. Arch Osteoporos 15:108
Hoang-Kim A, Kanengisser D (2020) Developing registries and effective care models for the management of hip fractures: aligning political, organizational drivers with clinical outcomes. Curr Osteoporos Rep 18:180–188
Majumdar SR, Lier DA, Hanley DA, Juby AG, Beaupre LA (2017) Economic evaluation of a population-based osteoporosis intervention for outpatients with non-traumatic non-hip fractures: the “Catch a Break” 1i [type C] FLS. Osteoporos Int 28:1965–1977
Dirschl DR, Rustom H (2018) Practice patterns and performance in U.S. fracture liaison programs: an analysis of >32,000 patients from the Own the Bone program. J Bone Joint Surg Am 100:680–685
Stephens JR, Caraccio D, Mabry DR, Stepanek KV, Jones MS, Hemsey DF (1995) Moore CR (2021) Implementation of a fracture liaison service for patients with hip fracture cared for on a hospital medicine service. Hosp Pract 49:41–46
Vranken L, Wyers CE, van Rietbergen B, Driessen JHM, Geusens PPMM, Janzing HMJ, van der Velde RY, van den Bergh JPW (2019) The association between prevalent vertebral fractures and bone quality of the distal radius and distal tibia as measured with HR-pQCT in postmenopausal women with a recent non-vertebral fracture at the Fracture Liaison Service. Osteoporos Int 30:1789–1797
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24:393–406
Ganda K, Mitchell PJ, Seibel MJ (2019) Chapter 3 - models of secondary fracture prevention: systematic review and metaanalysis of outcomes. In: Seibel MJ, Mitchell PJ (eds) Secondary Fracture Prevention. Academic Press, London, pp 33–62
Senay A, Delisle J, Raynauld JP, Morin SN, Fernandes JC (2016) Agreement between physicians’ and nurses’ clinical decisions for the management of the fracture liaison service (4iFLS): the Lucky Bone™ program. Osteoporos Int 27:1569–1576
Hung W-C, Yang C-H, Cheng W-L, Wu C-H (2019) Revisit three “I” model: a novel five “I” model of fracture liaison service. Osteoporos Int 30:2361–2362
Palcu P, Munce S, Jaglal SB, Allin S, Chishtie JA, Silverstein A, Kim S (2020) Understanding patient experiences and challenges to osteoporosis care delivered virtually by telemedicine: a mixed methods study. Osteoporos Int 31:351–361
Paskins Z, Crawford-Manning F, Bullock L, Jinks C (2020) Identifying and managing osteoporosis before and after COVID-19: rise of the remote consultation? Osteoporos Int 31:1629–1632
Marschollek M, Becker M, Bauer JM, Bente P, Dasenbrock L, Elbers K, Hein A, Kolb G, Künemund H, Lammel-Polchau C, Meis M, Zu M, Schwabedissen H, Remmers H, Schulze M, Steen EE, Thoben W, Wang J, Wolf KH, Haux R (2014) Multimodal activity monitoring for home rehabilitation of geriatric fracture patients—feasibility and acceptance of sensor systems in the GAL-NATARS study. Inform Health Soc Care 39:262–271
Geerds MAJ, Nijmeijer WS, Hegeman JH, Vollenbroek-Hutten MMR (2020) Mobile app for monitoring 3-month postoperative functional outcome after hip fracture: usability study. JMIR Hum Factors 7:e16989
Martin J, Viprey M, Castagne B, Merle B, Giroudon C, Chapurlat R, Schott A-M (2020) Interventions to improve osteoporosis care: a systematic review and meta-analysis. Osteoporos Int 31:429–446
Wu C-H, Tu S-T, Chang Y-F, Chan D-C, Chien J-T, Lin C-H, Singh S, Dasari M, Chen J-F, Tsai K-S (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone 111:92–100
Senay A, Perreault S, Delisle J, Morin SN, Fernandes JC (2020) Performance of a fracture liaison service in an orthopaedic setting: a report of key indicators and improvement of longitudinal outcomes. J Bone Joint Surg Am 102:486–494
French S, Choden S, Schmajuk G (2019) Quality measures and quality improvement initiatives in osteoporosis—an update. Curr Osteoporos Rep 17:491–509
Javaid MK, Sami A, Lems W, Mitchell P, Thomas T, Singer A, Speerin R, Fujita M, Pierroz DD, Akesson K, Halbout P, Ferrari S, Cooper C (2020) A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos Int 31:1193–1204
Sale JEM, Beaton D, Posen J, Elliot-Gibson V, Bogoch E (2014) Key outcomes are usually not reported in published fracture secondary prevention programs: results of a systematic review. Arch Orthop Trauma Surg 134:283–289
Voeten SC, Arends AJ, Wouters MWJM, Blom BJ, Heetveld MJ, Slee-Valentijn MS, Krijnen P, Schipper IB, JHH H, Dutch Hip Fracture Audit Group (2019) The Dutch Hip Fracture Audit: evaluation of the quality of multidisciplinary hip fracture care in the Netherlands. Arch Osteoporos 14:28
Liem IS, Kammerlander C, Suhm N, Blauth M, Roth T, Gosch M, Hoang-Kim A, Mendelson D, Zuckerman J, Leung F, Burton J, Moran C, Parker M, Giusti A, Pioli G, Goldhahn J, Kates SL (2013) Identifying a standard set of outcome parameters for the evaluation of orthogeriatric co-management for hip fractures. Injury 44:1403–1412
International Osteoporosis Foundation. Capture the Fracture. Implementation strategies. Coordinator-based systems for secondary prevention in fragility fracture patients. Available at: https://www.capturethefracture.org/implementation-strategies. Accessed 24 January 2022.
Fergusson K, Gill C, Harris R, Kim D, Mitchell P, Ward N. Clinical standards for fracture liaison services in New Zealand. 2021 second edition. Available at: https://osteoporosis.org.nz/wp-content/uploads/ONZ-FLS-Clinical-Standards-Sept-2021-1.pdf. Accessed 24 January 2022.
Japan Osteoporosis Society and Fragility Fracture Network Japan. Clinical standards for fracture liaison services in Japan. Available at: http://ffn.or.jp/wordpress/wp-content/uploads/2019/08/bf2ea636831d1fcc8bded072714defda.pdf. Accessed 24 January 2022.
Royal Osteoporosis Society. Effective secondary prevention: clinical standards for fracture liaison services. Available at: https://theros.org.uk/healthcare-professionals/fracture-liaison-services/. Accessed 24 January 2022.
Aboudiab M, Grados F, Batteux B, Henry-Desailly I, Fardellone P, Goëb V (2020) Vertebral fracture assessment (VFA) in patients over 50 years of age with a non-severe peripheral fracture. Osteoporos Int 31:1477–1486
Schousboe JT, Lix LM, Morin SN, Derkatch S, Bryanton M, Alhrbi M, Leslie WD (2019) Vertebral fracture assessment increases use of pharmacologic therapy for fracture prevention in clinical practice. J Bone Miner Res 34:2205–2212
Schousboe JT, Lix LM, Morin SN, Derkatch S, Bryanton M, Alhrbi M, Leslie WD (2019) Prevalent vertebral fracture on bone density lateral spine (VFA) images in routine clinical practice predict incident fractures. Bone 121:72–79
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Rosen HN, Vokes TJ, Malabanan AO, Deal CL, Alele JD, Olenginski TP, Schousboe JT (2013) The official positions of the International Society for Clinical Densitometry: vertebral fracture assessment. J Clin Densitom 16:482–488
Hawley S, Javaid MK, Prieto-Alhambra D, Lippett J, Sheard S, Arden NK, Cooper C, Judge A, REFReSH Study Group (2016) Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age Ageing 45:236–242
Neuerburg C, Mittlmeier L, Schmidmaier R, Kammerlander C, Böcker W, Mutschler W, Stumpf U (2017) Investigation and management of osteoporosis in aged trauma patients: a treatment algorithm adapted to the German guidelines for osteoporosis. J Orthop Surg Res 12:86
Li H, Wang Y, Wang R, Yue L, Chen S, Li C (2020) Effects of rosuvastatin and zoledronic acid in combination on the recovery of senile osteoporotic vertebral compression fracture following percutaneous vertebroplasty. J Int Med Res 48:300060520925390
Liu Z, Li C-W, Mao Y-F, Liu K, Liang B-C, Wu L-G, Shi X-L (2019) Study on zoledronic acid reducing acute bone loss and fracture rates in elderly postoperative patients with intertrochanteric fractures. Orthop Surg 11:380–385
Jia KQ, Southerland L, Phieffer L, Stephens JA, Ing SW (2020) Incorporation of a patient navigator into a secondary fracture prevention program identifies barriers to patient care. Aging Clin Exp Res 32:2557–2564
Martin J, Viprey M, Castagne B, Barral M, Chapurlat R, Julien C, Serrier H, Schott A-M (2020) Cost-effectiveness analyses of interventions to improve osteoporosis care in France. Arch Osteoporos 15:42
Majumdar SR, Lier DA, McAlister FA, Johnson JA, Rowe BH, Beaupre LA (2019) Cost-effectiveness of osteoporosis interventions to improve quality of care after upper extremity fracture: results from a randomized trial (C-STOP Trial). J Bone Miner Res 34:1220–1228
Clement RC, Ahn J, Mehta S, Bernstein J (2013) Economic viability of geriatric hip fracture centers. Orthopedics 36:e1509–e1514
Metcalfe D, Zogg CK, Judge A, Perry DC, Gabbe B, Willett K, Costa ML (2019) Pay for performance and hip fracture outcomes: an interrupted time series and difference-in-differences analysis in England and Scotland. Bone Joint J 101-B:1015–1023
Nishi T, Maeda T, Babazono A (2018) Association between financial incentives for regional care coordination and health care resource utilization among older patients after femoral neck fracture surgery: a retrospective cohort study using a claims database. Popul Health Manag 21:331–337
Valentin G, Pedersen SE, Christensen R, Friis K, Nielsen CP, Bhimjiyani A, Gregson CL, Langdahl BL (2020) Socio-economic inequalities in fragility fracture outcomes: a systematic review and meta-analysis of prognostic observational studies. Osteoporos Int 31:31–42
Malik AT, Retchin S, Phillips FM, Xu W, Peters K, Yu E, Khan SN (2020) Declining trend in osteoporosis management and screening following vertebral compression fractures – a national analysis of commercial insurance and medicare advantage beneficiaries. Spine J 20:538–546
Ong T, Copeland R, Thiam CN, Cerda Mas G, Marshall L, Sahota O (2021) Integration of a vertebral fracture identification service into a fracture liaison service: a quality improvement project. Osteoporos Int 32:921–926
Howlett DC, Drinkwater KJ, Mahmood N, Illes J, Griffin J, Javaid K (2020) Radiology reporting of osteoporotic vertebral fragility fractures on computed tomography studies: results of a UK national audit. Eur Radiol 30:4713–4723
Toal M, McLoughlin C, Pierce N, Moss J, English S, Lindsay JR (2020) Detection of vertebral fracture in an acute hospital setting: an intervention to reduce future fracture risk through fracture liaison service intervention? Arch Osteoporos 15:160
Schousboe JT, Davison ML, Dowd B, Thiede Call K, Johnson P, Kane RL (2011) Predictors of patients’ perceived need for medication to prevent fracture. Med Care 49:273–280
Abbad N, Lemeunier L, Chantelot C, Puisieux F, Cortet B (2016) Secondary prevention program for osteoporotic fractures at Lille University Hospital. Presse Med 45:375–377
Bunta AD, Edwards BJ, Macaulay WB Jr, Jeray KJ, Tosi LL, Jones CB, Sietsema DL, Kaufman JD, Murphy SA, Song J, Goulet JA, Friedlaender GE, Swiontkowski MF, Dirschl DR (2016) Own the bone, a system-based intervention, improves osteoporosis care after fragility fractures. J Bone Joint Surg Am 98:e109
Asian Pacific Fragility Fracture Alliance. Hip Fracture Registry Toolbox. A collaboration between the APGGA Hip Fracture Registry Working Group and the FFN Hip Fracture Audit Special Interest Group. Available at: https://apfracturealliance.org/wp-content/uploads/2021/06/APFFA-FFN-Hip-Fracture-Registry-Toolbox-Interactive-v1.0-FINAL.pdf. Accessed 24 January 2022.
Kanis JA, Cooper C, Rizzoli R, Reginster J-Y (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, Harris ST, Hurley DL, Kelly J, Lewiecki EM, Pessah-Pollack R, McClung M, Wimalawansa SJ, Watts NB (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocr Pract 26:1–46
Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D (2019) Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab 104:1595–1622
Kanis JA, Harvey NC, McCloskey E, Bruyère O, Veronese N, Lorentzon M, Cooper C, Rizzoli R, Adib G, Al-Daghri N, Campusano C, Chandran M, Dawson-Hughes B, Javaid K, Jiwa F, Johansson H, Lee JK, Liu E, Messina D et al (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31:1–12
Chui K, Thakrar A, Shankar S (2020) Evaluating the efficacy of a two-site (‘COVID-19’ and ‘COVID-19-free’) trauma and orthopaedic service for the management of hip fractures during the COVID-19 pandemic in the UK. Bone Jt Open 1:190–197
Acknowledgements
Lisa A. Humphries, PhD, of Amgen Inc. and Martha Mutomba (on behalf of Amgen Inc.) provided medical writing support.
Funding
Open access funding provided by Lund University. Amgen Inc. funded this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
Kristina E. Åkesson is a consultant for Amgen, Renapharma, and UCB Pharma and is on the speakers’ bureau for Amgen. Kirtan Ganda has nothing to disclose. Cynthia Deignan is an employee and stockholder of Amgen. Mary K. Oates is an employee and stockholder of Amgen. Amy Volpert is an employee of BioScience Communications, which received funding from Amgen for this project. Keyla Brooks is an employee and stockholder of UCB Pharma. David Lee is a former employee and stockholder of Amgen and is currently an employee of Health Collaboration Partners LLC, a healthcare consulting firm. Douglas R. Dirschl is a consultant for Stryker, BONESUPPORT, SI-BONE, and Acumed. Andrea J. Singer has received research support from Radius and UCB Pharma; is a consultant for AgNovos, Amgen, Radius, and UCB Pharma; and is on the speakers’ bureau for Amgen and Radius.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 246 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Åkesson, K., Ganda, K., Deignan, C. et al. Post-fracture care programs for prevention of subsequent fragility fractures: a literature assessment of current trends. Osteoporos Int 33, 1659–1676 (2022). https://doi.org/10.1007/s00198-022-06358-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06358-2