Abstract
Summary
A successful therapy needs high level of adherence consisting in right drug intake in terms of persistence and compliance. Our study suggests adherence is higher if spot (less than 30 days) therapies are excluded; the analysis of spot therapy causes underlines the importance of the interpersonal aspects of medical practice.
Introduction
A successful therapy needs a high level of adherence consisting in right drug intake in terms of persistence and compliance. The aim of this study was to evaluate anti-osteoporotic therapies recorded in general practitioner databases in the area of Rome, which used the same computerized medical record management. The study focused on evaluating therapy adherence, any adherence changes excluding spot therapies (less than 30 days), and any cause of early therapy discontinuation in a subgroup of patients randomly selected.
Methods
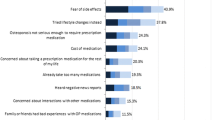
Thirty-one databases were evaluated, including a total of 6,390 anti-osteoporotic therapies: 5,853 were prescribed to women and 537 to men. The prescribed drugs were: vitamin D (13 %), calcium (8.7 %), vitamin D + calcium (40.1 %), raloxifene (3.3 %), alendronate (16.4 %), risedronate (7.7 %), clodronate (10.4 %), or other drugs (0.4 %). Spot therapies represented 53.7 % of the total prescriptions. The difference between adherence in the total group (24.64 %) and the group excluding spot therapies (43.38 %) is significant. The main factors influencing low adherence were side effects (27 %), misinformation given by the physician (17 %), insufficient motivation (9 %), difficult intake (9 %), and no perceived benefits (9 %).
Results
Our study suggests adherence is high and similar to other chronic diseases if spot therapies are excluded. The analysis of spot therapy causes suggests that an important role is played by the physician and the interpersonal aspects of medical practice, especially at the first prescriptions.
Conclusions
The physician should collaborate with patients in choosing a personalized medical treatment. Reducing spot therapy could be the real goal in order to improve anti-osteoporotic therapy adherence.




Similar content being viewed by others
References
Kanis JA, Cooper C, Hiligsmann M, Rabenda V, Reginster J-Y, Rizzoli R (2011) Partial adherence: a new perspective on health economic assessment in osteoporosis. Osteoporos Int 22:2565–2573
Mc Combs JS, Thiebaud P, McLaughlin-Miley C, Shi J (2004) Compliance with drug therapies for the treatment and prevention of osteoporosis. Maturitas 48(3):271–287
Cramer JA, Amonkar MM, Hebborn A, Altman R (2005) Compliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosis. Curr Med Res Opin 21(19):1453–1460
Penning-van Beest FJA, Erkens JA, Olson M, Herings RMC (2008) Loss of treatment benefit due to low compliance with bisphosphonate therapy. Osteoporos Int 19:511–517
Zambon A, Baio G, Merlino L, Mazzaglia G, Corrao G (2008) Dicontinuity and failures of therapy with bisphosphonates: joint assessment of predictors with multi-state models. Pharmacoepidem Dr S 17:260–269
Gallagher A, Rietbrock S, Olson M, Van Staa TP (2008) Fracture outcomes related to persistence and compliance with oral bisphosphonates. J Bone Miner Res 23:1569–1575
Siris ES, Harris ST, Rosen CJ, Barr CE, Abbot T (2006) Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc 81(8):1013–1022
Seeman E, Compston J, Adachi J, Brandi ML, Cooper C, Cramer JA (2007) Non-compliance: the Achilles’ heel of anti-fracture efficacy. Osteoporos Int 18:711–719
Sabaté E (ed) (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
DiMatteo MR (2004) Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care 42:200–209
Weycker D, Macarios D, Edelsberg J, Oster G (2006) Compliance with drug therapy for postmenopausal osteoporosis. Osteoporos Int 17:1645–1652
Rossini M, Bianchi G, Di Munno O, Giannini S, Adami S (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17(6):914–921
Rietbrock S, Olson M, vanStaa TP (2009) The potential effects on fracture outcomes of improvements in persistence and compliance with bisphosphonates. Q J Med 102:35–42
Segal E, Shalom S (2009) Two years adherence to anti-osteoporotic medications in postmenopausal Israeli women. Arch Gerontol Geriatr 49(3):360–363
Rossini M, Viapiana O, Gatti D, James G, Girardello S, Adami S (2005) The long term correction of vitamin D deficiency: comparison between different treatments with vitamin D in clinical practice. Minerva Med Apr 96(2 Suppl 2):1–7
Segal E, Tamir A, Shalom S (2003) Compliance of osteoporotic patients with different treatment regimens. IMAJ 5:859–862
Penning-van Beest FJA, Goettsch WG, Erkens JA, Herinhs RMC (2006) Determinants of persistence with bisphosphonates: a study in women with postmenopausal osteoporosis. Clin Ther 28(2):236–242
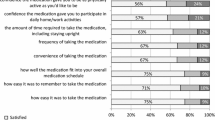
Carr AJ, Thompson PW, Cooper C (2006) Factors associated with adherence and persistence to bisphosphonate therapy in osteoporosis: a cross-sectional survey. Osteoporos Int 17:1638–1644
Hall JA, Roter DL, Katz NR (1988) Meta-analysis of correlates of provider behavior in medical encounters. Med Care 26:657–675
Stewart MA (1996) Effective physician–patient communication and health outcomes: a review. CMAJ 152:1423–1433
Roter DL, Hall JA, Aoki Y (2002) Physician gender effects in medical communication: a meta-analytic review. JAMA 288(6):756–764
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tafaro, L., Nati, G., Leoni, E. et al. Adherence to anti-osteoporotic therapies: role and determinants of “spot therapy”. Osteoporos Int 24, 2319–2323 (2013). https://doi.org/10.1007/s00198-013-2283-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2283-z