Abstract
Introduction
Poor adherence to prescribed treatments is widespread in clinical practice and this can lead to potentially life-threatening events. This problem is apparently very common for osteoporosis treatment but the causes of discontinuation and low compliance are complex and poorly defined.
Methods
Global adherence to osteoporosis treatment was specifically addressed in a nation-wide survey carried out in 9851 postmenopausal women referred to 141 Italian centres for osteoporosis management for a follow-up assessment, at least one year after having been prescribed a treatment with one of the following drugs: calcium±vitamin D supplements alone (CaVitD), hormone replacement therapy (HRT), raloxifene 60 mg (RLX), intramuscular clodronate 100 mg/7-14 days (CLOD), risedronate 5 mg/day (RIS) and alendronate 10mg/daily (ALN10) or 70 mg once weekly (ALN OW).
Results
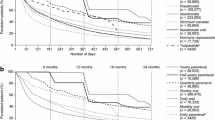
Overall 19.1% of the patients discontinued the prescribed drug before attending the bone mass re-evaluations, more than half of them within the first 6 months. The discontinuation rate was significantly different between the treatments. The medications most frequently interrupted within one year were CLOD (28.7%; p<0.01 versus any other treatment), while by far the least interrupted was ALN-OW (6.9%; p<0.001 versus any other treatment). The most frequent reasons for discontinuation were drug related side effects, insufficient motivation to treatment and fear of side effects. The prevalence of the reasons for discontinuation were different among treatments: safety concerns were very common for HRT, lack of motivation was the most common cause for CaVitD and CLOD, and drug related side effects for RIS, ALN and RLX. Persistence to treatment was significantly higher in patients with previous vertebral fractures, densitometric osteoporosis, on corticosteroid or anti-inflammatory treatments. A significantly increased risk of treatment interruption was found among patients on benzodiazepine or gastro-protective agents and in patients in whom a bone measurement was not readily available. The highest compliance to recommended dosing was observed with ALN OW and HRT (p<0.001 versus any other) and the lowest for CaVitD (p<0.01 versus any other). Poor treatment compliance (<50% drug taken) was significantly related to benzodiazepine and gastroprotective use, while a significantly better compliance was associated with recognized risk factors for osteoporosis: early menopause, low bone mass values values, previous vertebral fractures. The poorest adherence was observed when treatments were prescribed by General practitioners (GPs), and orthopaedic surgeons (p<0.01 versus global mean).
Conclusions
The results of this large survey of Italian osteoporotic women indicates that the most important determinant of both persistence and compliance to treatment is the type of drug prescribed with a definite advantage of ALN-OW. Treatment compliance is particularly poor for CaVitD and this emphasizes the need for new ways to supplement at least vitamin D. The main reasons for discontinuation are side effects and lack of motivation while the best treatment adherence was observed in patients with severe and well documented osteoporosis.


Similar content being viewed by others
References
Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N (1993) Medication compliance: a healthcare problem. Ann Pharmacother 27 [Suppl 9]:S1–S24
Miller NH (1997) Compliance with treatment regimens in chronic asymptomatic diseases. Am J Med 102:43–49
Sung JC, Nichol MB, Venturini F, Bailey KL, McCombs JS, Cody M (1998) Factors affecting patient compliance with antihyperlipidemic medications in an HMO population. Am J Manag Care 4:1421–1430
Coronary drug project (1980) Influence of adherence to treatment and response of cholesterol on mortality in the coronary drug project. N Engl J Med 303:1038–1041
Schweizer RT, Rovelli M, Palmeri D, Vossler E, Hull D, Bartus S (1990) Noncompliance in organ transplant recipients. Transplantation 49:374–377
Cramer JA, Glassman M, Rienzi V (2002) The relationship between poor medication compliance and seizures. Epilepsy Behav 3:338–342
Zygmunt A, Olfson M, Boyer CA, Mechanic D (2002) Interventions to improve medication adherence in schizophrenia. Am J Psychiatry 159:1653–1664
Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM, Pressman AR, Ettinger B(2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
Segal E, Tamir A, Ish-Shalom S (2003) Compliance of osteoporotic patients with different treatment regimens. Isr Med Assoc J 5:859–862
Turbi C, Herrero-Beaumont G, Acebes JC, Torrijos A, Grana J, Miguelez R, Sacristan JA, Marin F (2004) Compliance and satisfaction with raloxifene versus alendronate for the treatment of postmenopausal osteoporosis in clinical practice: an open-label, prospective, nonrandomized, observational study. Clin Ther 26:245–256
Lombas C, Hakim C, Zanchetta JR (2001) Compliance with alendronate treatment in an osteoporosis clinic. J Bone Miner Res 15[Suppl 1]:S529
McCombs JS, Thiebaud P, McLaughlin-Miley C, Shi J (2004) Compliance with drug therapies for the treatment and prevention of osteoporosis. Maturitas 48:271–287
Hamilton B, McCoy K, Taggart H (2003) Tolerability and compliance with risedronate in clinical practice. Ostoporos Int 14:259–262
Yood AR, Emani S, Reed JI, Edelman Lewis B, Charpentier M, Lydick E (2003) Compliance with pharmacologic therapy for osteoporosis. Osteoporos Int 14:965–968
Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15:1003–1008
Papaioannou A, Ioannidis G, Adachi JD, Sebaldt RJ, Ferko N, Puglia M, Brown J, Tenenhouse A, Olszynski WP, Boulos P, Hanley DA, Josse R, Murray TM, Petrie A, Goldsmith CH (2003) Adherence to bisphosphonates and hormone replacement therapy in a tertiary care setting of patients in the CANDOO database. Osteoporos Int 14:808–813
Kayser J, Ettinger B, Pressman A (2001) Postmenopausal hormonal support: discontinuation of raloxifene versus estrogen. Menopause 8:328–332
Ettinger B, Li DK, Klein R (1998) Alendronate use among 812 women: prevalence of gastrointestinal complaints, noncompliance with patient instructions, and discontinuation. J Manage Care Pharm 4:488–492
Kotzan JA, Martin BC, Wade WE (1999) Persistence with estrogen therapy in a postmenopausal Medicaid Population. Pharmacotherapy 19:363–369
Recker RR, Gallagher R, MacCosbe PE (2005) Effect of dosing frequency on bisphosphonate medication adherence in a large longitudinal cohort of women. Majo Clin Proc 80:856–861
Faulkner DL, Young C, Hutchins D, McCollam JS (1998) Patient noncompliance with hormone replacement therapy: a nationwide estimate using a large prescription claims database. Menopause 5:226–229
Cole RP, Palushock S, Haboubi A (1999) Osteoporosis management: physician’s reccomendations and women’s compliance following osteoporosis testing. Women Health 29:101–115
Claxton AJ, Cramer J, Pierce C (2001) A systematic review of the associations between dose regimens and medication compliance. Clin Ther 23:1296–1310
Simon JA, Lewiecki EM, Smith ME, Petruschke RA, Wang L, Palmisano JJ (2002) Patient preference for once-weekly alendronate 70 mg versus once-daily alendronate 10 mg: a multicenter, randomized, open-label, crossover study. Clin Ther 24:1871–1886
Kendler D, Kung AWC, Fuleihan GE et al (2004) Patients with osteoporosis prefer once weekly to once daily dosing with alendronate. Maturitas 48:243–251
Weiss M, Vered I, Foldes AJ, Cohen YC, Shamir-Elron Y, Ish-Shaloms S (2005) Treatment preference and tolerability with alendronate once weekly over a 3-month period: an Israeli multi-center study. Aging Clin Exp Res 17:143–149
Lemay A (2002) The relevance of the Women’s Health Initiative results on combined hormone replacement therapy in clinical practice. J Obstet Gynaecol Can 24:711–715
Pressman A, Forsyth B, Ettinger B, Tosteson A (2001) Initiation of osteoporosis treatment after bone mineral density testing. Osteoporos Int 12:337–342
Pickney Cs, Arnason JA (2005) Correlation between patient recall of bone densitometry results and subsequent treatment adherence. Osteoporos Int 16:1156–1160
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors’ study for the “Treatment of Osteoporosis in clinical Practice” (T.O.P.) Study Group, see Appendix.
Appendix
Appendix
“Treatment of Osteoporosis in clinical Practice” (T.O.P.) Study Group (names and Italian towns of the study site):
Adami S, Verona; Agnello RI, Palermo; Armellini F, Vicenza; Astazzi P, Frosinone; Aversa A, Milano; Badagliacca V, Palermo; Baldoncini A, Arezzo; Barbagallo M, Palermo; Bardoscia A, Bari; Bartorelli, Roma; Bernini L, Pisa; Bertolucci D, Lucca; Bevilacqua M, Milano; Bianchi G, Genova; Biondi M, Forlì; Bonali C, Bari; Brandi M L, Firenze; Broggini M, Varese; Bruni G, Teramo; Bruno A, Lecce; Cacace E, Cagliari; Calabretto C, Brescia; Calitro M, Bari; Caminiti M, Reggio Calabria; Caputo G, Lecce; Carruba M, Caltanissetta; Castellitto D, Frosinone; Cataldi U, Roma; Caudarella R, Bologna; Cazzola M, Varese; Cecchetti R, Pisa; Ciaschini R, Pesaro; Cirillo F, Siracusa; Coaccioli S, Terni; Colonna M, Torino; Combi F, Milano; Conati GF, Belluno; Confalonieri N, Milano; Cutolo M, Genova; Dalle Carbonare L, Padova; Dalmonte E, Ravenna; D’Amore M, Bari; D’Avola G, Catania; De Gennaro N, Napoli; De Michele F, Taranto; De Ferrari, Milano; Del Vino PG, Torino; Di Domenica F, Milano; Di Monaco M, Torino; Di Munno O, Pisa; Di Virgilio R, Treviso; Dominguez LJ, Palermo; Fabbri G, Modena; Fasani M, Roma; Fidotti E, Roma; Fiore E, Catania; Forlenza A, Potenza; Frediani B, Siena; Frisina N, Messina; Galeri S, Brescia; Galfo G, Ragusa; Gandolini G, Milano; Gatti G, Roma; Gatto G, Napoli; Gemignani G, Lucca; Ghiazza F, Alessandria; Gipponi C, Brescia; Giustina A, Brescia; Grassi S, Napoli; Grimaldi G, Salerno; Guanziroli C, Como; Guzzo G, Cosenza; Isaia GC, Torino; Latte VM, Napoli; Laurenza F, Roma; Lo Cascio V, Verona; Lovato R, Vicenza; Lovero R, Bari; Lucchesi R, Latina; Lunetta M, Caltanissetta; Lusenti T, Reggio Emilia; Maggiolini FR, Roma; Mannarino E, Perugia; Mantero M, Genova; Marcocci C, Pisa; Marcon G, Venezia; Mastaglio C, Como; Matina A, Palermo; Mattu G, Latina; Maugeri D, Catania; Milini C, Brescia; Minisola S, Roma; Minozzi M, Roma; Molea N, Livorno; Moro L, Gorizia; Mosconi S, Bergamo; Mottino G, Alessandria; Muia E, Lecce; Muratore M, Lecce; Napoli C, Catania; Napolitano C, Latina; Noviello A, Bari; Nuti R, Siena; Occhipinti G, Livorno; Ortolani S, Milano; Ortore V, Roma; Osella G, Torino; Padula S, Napoli; Palummeri E, Genova; Pangrazio MT, Bari; Pedicino C, Campobasso; Pedrazzoni M, Parma; Pellerito R, Torino; Perrone G, Roma; Petricca A, Chieti; Policicchio D, Avellino; Pozone M, L’Aquila; Quattrocchi G,Messina; Reina G, Catania; Resmini G, Bergamo; Rigliano V, Brindisi; Rini GB, Palermo; Rollo V, Lecce; Rondena M, Milano; Rossini M, Verona; Rubinacci A, Milano; Russo V, Messina; Sabetta S, Salerno; Salmaggi P, Roma; Savoca S, Catania; Schinella D, Pordenone; Sdanganelli F, Taranto; Senin U, Perugina; Sfrappini M, Ascoli Piceno; Silveri F, Ancona; Sinigaglia L, Milano; Spangaro F, Trieste; Spezio L, Napoli; Spinazzè R, Treviso; Stisi S, Benevento; Tartarelli G, Massa; Tenca A, Cremona; Trevisan C, Milano; Trotta F, Ferrara; Ulivieri FM, Milano; Valentini G, Napoli; Ventura L, Mantova; Zanatta A, Verona.
Rights and permissions
About this article
Cite this article
Rossini, M., Bianchi, G., Di Munno, O. et al. Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17, 914–921 (2006). https://doi.org/10.1007/s00198-006-0073-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0073-6