Abstract
Summary
The Women's Health Initiative (WHI) double-blind, placebo-controlled clinical trial randomly assigned 36,282 postmenopausal women in the U.S. to 1,000 mg elemental calcium carbonate plus 400 IU of vitamin D3 daily or placebo, with average intervention period of 7.0 years. The trial was designed to test whether calcium plus vitamin D supplementation in a population in which the use of these supplements was widespread would reduce hip fracture, and secondarily, total fracture and colorectal cancer.
Introduction
This study further examines the health benefits and risks of calcium and vitamin D supplementation using WHI data, with emphasis on fractures, cardiovascular disease, cancer, and total mortality.
Methods
WHI calcium and vitamin D randomized clinical trial (CT) data through the end of the intervention period were further analyzed with emphasis on treatment effects in relation to duration of supplementation, and these data were contrasted and combined with corresponding data from the WHI prospective observational study (OS).
Results
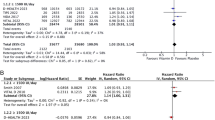
Among women not taking personal calcium or vitamin D supplements at baseline, the hazard ratio [HR] for hip fracture occurrence in the CT following 5 or more years of calcium and vitamin D supplementation versus placebo was 0.62 (95 % confidence interval (CI), 0.38–1.00). In combined analyses of CT and OS data, the corresponding HR was 0.65 (95 % CI, 0.44–0.98). Supplementation effects were not apparent on the risks of myocardial infarction, coronary heart disease, total heart disease, stroke, overall cardiovascular disease, colorectal cancer, or total mortality, while evidence for a reduction in breast cancer risk and total invasive cancer risk among calcium plus vitamin D users was only suggestive.
Conclusion
Though based primarily on a subset analysis, long-term use of calcium and vitamin D appears to confer a reduction that may be substantial in the risk of hip fracture among postmenopausal women. Other health benefits and risks of supplementation at doses considered, including an elevation in urinary tract stone formation, appear to be modest and approximately balanced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Women's Health Initiative (WHI) double-blind, placebo-controlled clinical trial (CT) randomly assigned 36,282 postmenopausal women in the U.S. to 1,000 mg elemental calcium carbonate plus 400 IU of vitamin D3 daily or placebo, with average intervention period of 7.0 years. The trial was designed to test whether calcium plus vitamin D (CaD) supplementation in a population in which the use of these supplements was widespread would reduce hip fracture, and secondarily, total fracture and colorectal cancer. Even though CaD led to a significantly higher hip and total body bone mineral density than placebo (P < 0.01), there was no compelling evidence for hip or total fracture risk reduction [1]. Among women who adhered to study medications, however, there was a lower hip fracture incidence in the intervention group [1], though this type of adherence-adjusted analysis involves additional modeling assumptions and lacks the reliability of the corresponding intention-to-treat analysis. Additional analyses led to reports of no clear evidence of benefit or harm for colorectal cancer [2], breast cancer [3], or other invasive cancer [4], though the possibility of a breast cancer risk reduction among women using little or no personal calcium supplements was noted [3]. Additional reports noted no clear evidence of influence on coronary heart disease (CHD) risk, defined in WHI and here as nonfatal myocardial infarction (MI) or CHD death [5], and to the possibility of a reduction in total mortality [6]. A modest elevation in urinary tract stone occurrence in the intervention group was also observed [1, 7].
The WHI trial has been criticized in that participating women were allowed to continue their personal use of calcium and/or vitamin D, in addition to taking study pills [8]. Our perspective, as WHI investigators, is that the question of health risks and benefits associated with CaD supplementation, beyond the use of personal supplements, is of direct importance to postmenopausal women in the general population. We agree, however, that subset analyses restricted to women not taking personal supplements are of considerable interest from both etiologic and public health perspectives.
Bolland et al. [8] reanalyzed WHI CaD trial data and reported an interaction (P = 0.04) in hazard ratio (HR) for “clinical MI” according to whether or not women were not using personal calcium supplements at baseline. A similar interaction was reported for combined clinical MI and stroke. These authors summarize that WHI trial data do not provide “definitive evidence” of an adverse effect of calcium and vitamin D on cardiovascular events, but they argue that data from other trials of calcium and vitamin D, or of calcium alone, in conjunction with WHI data, lead to the conclusion that calcium supplements with or without vitamin D increase the risk of cardiovascular events.
Essentially the same investigator group reanalyzed the WHI trial data further and reported [9] an HR interaction for total cancer and invasive breast cancer, but not for hip or total fractures or total mortality, this time according to whether participating women were using personal supplements of either calcium or vitamin D at baseline. They interpreted these data as providing evidence of benefit for breast cancer and total cancer among women not taking personal supplements. Chlebowski et al. [10] pointed out the need for a cautious interpretation in these subgroup analyses and described lack of support for a breast cancer risk reduction from other WHI data sources.
Here, we use WHI data resources to examine these topics further, with emphasis on the experience of women in the CT who were not using calcium or vitamin D supplements at baseline, as well as on the experience of the overall trial cohort. We include comparative analyses from the WHI Observational Study (OS), a prospective cohort study among 93,676 postmenopausal women drawn from the same catchment areas, for independent assessment of calcium and vitamin D health risks and benefits in WHI populations. Since OS women may have used these supplements for some years prior to WHI enrollment, these data have potential to augment trial information on the health effects of longer-term supplementation (e.g., 5 or more years). In fact, there have been several observational study reports of calcium supplementation in relation to cardiovascular disease [11–15]. While most of these report null or non-significant associations, the most recent of these reported a noteworthy increase in MI, but not stroke, incidence among the 3.6 % of an EPIC-Heidelberg cohort enrollees who were identified as calcium supplement users [15].
These types of observational analyses can be difficult to interpret since nutritional supplement users tend to have quite different characteristics from non-users [e.g., 16], typically leaving uncertainty as to how completely confounding has been controlled. Also, common reasons for taking nutritional supplements include the belief that these preparations may prevent chronic diseases, such as cardiovascular disease, osteoporosis, and cancer [16, 17], raising the specter of “confounding by indication”, which may tend to offset any “healthy supplement user” bias. Here, as in our earlier WHI combined CT and OS analyses of postmenopausal hormone therapy [18–23], our analyses allow for outcome-specific residual confounding in the OS. In effect, these combined CT and OS analyses allow an entirely separate overall HR from the OS versus the CT, so that OS data are used very conservatively to strengthen analysis of temporal HR variation patterns. The OS data also permit some examination of disease outcome associations for calcium and vitamin D supplementation separately.
Analyses presented here examine a range of clinical outcomes including fractures, invasive cancers, cardiovascular diseases, and total mortality. In each case, beyond overall supplementation effects, temporal associations of the HR with duration of supplementation, and the agreement of patterns between clinical trial and observational study, are examined. Urinary tract stone occurrence analyses in the CT, by personal supplement use category, are also presented to facilitate health benefit versus risk consideration.
Methods
Study populations and calcium and vitamin D supplementation
A total of 36,282 postmenopausal women 50–79 years of age were randomized at 40 clinical sites to 1,000 mg calcium plus 400 IU vitamin D3 daily, given in two equal doses, versus placebo in the WHI CaD trial during 1994–99. Concurrent calcium supplementation was permitted, as was vitamin D supplementation up to 600 IU daily (later increased to 1,000 IU daily). Details of the study design [24] and baseline characteristics [1, 2, 25] have been presented. All participating women provided written informed consent.
No personal use of calcium or vitamin D supplements at baseline was reported by 42.2 % (15,302) of trial enrollees, whereas 43.5 % (15,796), 9.4 % (3,419), and 2.9 % (1,060) reported use of calcium plus vitamin D, calcium only, and vitamin D only, respectively, while baseline supplementation information was not available for 1.9 % (705) of women. Both single supplement and multivitamin/multimineral supplements were included in assessing personal use.
The companion WHI prospective Observational Study (OS) enrolled 93,676 postmenopausal women 50–79 years of age from the same catchment population during 1994–98. Baseline characteristics have been presented [26]. To align with CT exclusionary criteria, we excluded 5,145 women with a baseline history of breast cancer, 15,511 women with no mammogram within 2 years prior to OS enrollment, 1,108 daily corticosteroid users, and 5,675 women who reported urinary tract stones at baseline, leaving 68,719 OS women. Of these, 34.3 % (23,561) reported no baseline supplementation with calcium or vitamin D, 49.9 % (34,257) reported use of both calcium and vitamin D, 12.5 % (8,576) reported calcium only, and 3.4 % (2,325) reported vitamin D only. Among the 42,833 baseline calcium users, the 5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles for daily dosage (milligrams per day) were 57, 143, 200, 571, 1,000, 1,305, and 1,640, respectively. We defined baseline calcium users in the OS as those taking ≥500 mg/day and excluded those consuming a lower dosage from our analysis. This cutpoint gives a user group having average daily dose similar to the 1,000 mg/day used in the WHI trial. Similarly, the corresponding percentiles for vitamin D (IU/day) were 125, 171, 400, 400, 400, 600, and 800 with 58 % of users reporting 400 IU/day. We defined vitamin D users in the OS as those taking ≥400 IU/day and excluded those taking a lower dosage from analysis. Following these exclusions, there were 15,476 calcium plus vitamin D users, 5,941 calcium-only users, and 1,914 vitamin D-only users at baseline in the OS which along with the previously mentioned 23,561 non-users of either supplement entails 46,892 OS women.
Data collection, follow-up, and outcome ascertainment
Clinical outcomes were self-reported semiannually in the CT and annually in the OS [27]. Medical record documentation of these reports was obtained and diagnoses were confirmed at WHI clinical centers by physician adjudicators who were blinded to clinical trial randomization assignments. All clinical outcomes considered here, except certain fractures in the OS, were locally confirmed in this manner. Additionally, cases of coronary heart disease (CHD), stroke, and death were further adjudicated by a central committee in the CT, as were a fraction of such cases in the OS. Also, locally confirmed cases of breast cancer, colorectal cancer, and hip fracture in both the CT and OS were centrally reviewed and classified at the WHI clinical coordinating center. Fractures other than hip fractures were also adjudicated in the CT, as was the case for a small fraction of other fractures in the OS. Otherwise, self-report of fracture was relied on in the OS.
Information on adherence to assigned study pills was obtained semiannually in the CT through unused pill counts. Dietary supplement data were collected in both the CT and OS during in-person clinic visits. Women brought supplement bottles to the baseline clinic visit and to annual visits thereafter in the CT and to the baseline and 3-year clinic visit in the OS. A standardized interviewer-administered four-page form was used to collect information on single vitamin and mineral supplements and on multivitamin/multimineral use. Staff members directly transcribed the ingredients for each supplement and asked participants about the frequency (pills/week) and duration (months and years) of use for each supplement [28, 29].
The CaD trial ended as planned in March 2005 after an average intervention period of 7.0 years. Follow-up data from the OS are included here through 12/16/2004 to provide a comparable average follow-up period of 7.2 years. More recent health risk and benefit follow-up data from the trial are currently being consolidated for a separate presentation.
Standard procedures were used in the CT and OS to collect data on age, race/ethnicity, reproductive/gynecologic history, education, physical activity, medical history, family or personal history of cancer or coronary heart disease, diabetes mellitus, current health status, tobacco and alcohol use, and self-administered food frequency questionnaire. The WHI food frequency questionnaire (FFQ), in English or Spanish, involved 122 foods or food groups, 19 adjustment questions, 4 summary questions, and was designed to assess typical intakes over the preceding 3 months [30]. Medication inventories were obtained at clinic visits, in the same manner as dietary supplements.
Statistical analysis
Principal data analyses focus on the estimation of hazard ratios corresponding to calcium and vitamin D supplementation, combined and separately, for each of the following clinical outcomes: hip fracture, total fracture, invasive colorectal cancer, invasive breast cancer, total invasive cancer (excluding non-melanoma skin cancer), total mortality, MI, CHD, total heart disease (CHD, revascularization, angina pectoris, congestive heart failure) , stroke (combined ischemic and hemorrhagic), and total cardiovascular disease (CVD) (total heart disease, stroke, carotid artery disease, peripheral vascular disease).
For each clinical outcome, the baseline hazard rate in the Cox regression model is stratified on cohort (CT versus OS), baseline age (5-year categories), and current use of postmenopausal estrogens or estrogens plus progestin defined as randomized to treatment if in the WHI hormone therapy trials [24] and as current hormone therapy use at baseline otherwise. Prior use of estrogens or estrogens plus progestin, duration of any such prior use, and FFQ estimates of usual calcium and vitamin D consumption were also included as a modeled regression variables in the Cox model, in both the CT and the OS. Time from WHI enrollment is the “basic time variable” in these analyses. Hazard ratios were calculated separately for <2, 2–5, and ≥5 years from initiation of supplementation to assess the temporal relationship between supplementation and any effects on clinical outcome. In the CT, time from supplement initiation is defined as time from randomization, whereas in the OS time from initiation of supplement use is defined as the sum of duration of use at baseline plus time from OS enrollment. Duration of use was defined as the longer of the two durations for women using both calcium and vitamin D supplements at baseline.
To further control confounding in the OS the hazard ratio regression model included an outcome-specific list of potential baseline confounding factors as is shown in Supplementary Table 1. For each outcome, this list included a linear term in age, an indicator of non-white ethnicity, body mass index (BMI) categorized variables for 25–29.9, for 30–34.9, and for ≥35.0 along with a linear term in BMI, and indicator variables for current or past cigarette smoking, in addition to other listed outcome-specific variables.
Analyses for each clinical outcome category were carried out using the entire CT enrollment, and also in the subsets of women who were not taking personal calcium or vitamin D supplements at baseline (“No personal supplements” subset) or were doing so (“Personal supplements” subset), and HR equality between these subsets was tested. For each analysis hazard ratios (HRs) and estimated 95 % confidence intervals (CIs) are presented according to years from supplement initiation (<2, 2–5, and >5) as a time-varying covariate. Significance levels (P values) are presented for a test of trend across the three time from initiation categories, coded as 0, 1, or 2, respectively. In addition, corresponding HR estimates from combined trial and observational data sets are given. These analyses allow for a residual confounding in the OS, by including a product term in the regression model between the OS versus CT indicator variable and the CaD user indicator variable. This variable allows the HR for CaD supplementation to differ by an overall multiplicative factor in the OS compared to the CaD trial, so that the OS data contribute to HR patterns with time from initiation but not to the absolute HR assessments in these combined analyses. With this modeling approach, overall HRs from combined CT and OS analyses are identical to those from the CT alone; but HR trend tests, which combine contributions from each cohort, may be strengthened by inclusion of the OS data. HRs and 95 % CIs for the entire follow-up period were calculated also, separately for the CT and OS.
Additional HR analyses in the CT censor the follow-up for women 6 months after a change from baseline in supplementation category, allowing the HRs to be interpreted in terms of duration of supplement use among adherent women, with continuing adherence defined as taking 80 % or more of assigned study medications in the preceding year. These adherence-adjusted analyses were conducted with and without inverse probability weighting in the Cox model, with weighting by estimated adherence probability, and with adherence probabilities estimated in a time-varying fashion using logistic regression models that include the Supplementary Table 1 variables.
Analyses were also conducted separately according to decade of baseline age and according to prior history of CVD.
Nominal 95 % CIs are presented for HR parameters, and all P values presented are 2-sided.
Results
Table 1 shows number of cases for each clinical outcome and age-adjusted incidence rates for both cohorts according to randomization assignment in the CT and according to baseline use of calcium and vitamin D supplements in the OS. Incidence rates for most outcomes differed little between randomized groups in the CT.
Table 2 provides HR estimates for fracture, and death according to years from CaD initiation, both for the CT as a whole and for the trial subset not using personal calcium or vitamin D at baseline; for the OS with outcome-specific confounding control; and for the combined CT and OS, with CT component including either the entire trial cohort or the subset not using personal supplements.
In women not taking supplements at baseline, the HR for hip fracture in the CT following 5 or more years of CaD supplementation versus placebo was 0.62 (95 % CI, 0.38 to 1.00). In combined analyses of CT and OS data (with residual confounding provision in the OS), the corresponding HR was 0.65 (95 % CI, 0.44 to 0.98) with evidence (P = 0.02) of HR trend with time from calcium and vitamin D initiation. Thus, there was evidence for lower hip fracture rates following some years of calcium plus vitamin D use in the subset of women not taking personal calcium or vitamin D supplements. This risk reduction was suggestive, but not clearly evident in the trial cohort as a whole (HR 0.82; 95 % CI, 0.61 to 1.12), or in combined trial and OS analyses. These combined overall CT and OS analyses provide some evidence for hip fracture benefit in the 5 or more years category (HR 0.78; 95 % CI, 0.59 to 1.03). Total fracture showed little evidence for association with CaD supplementation, with HRs from the OS tending to be larger than those from the CT.
To help interpret the hip fracture HRs, it can be noted that the FFQ 5th, 25th, 50th, 75th, and 95th percentiles for dietary calcium (milligram per day) were 291, 512, 738, 1,043, and 1,650, and for dietary vitamin D (IU/day), and were 47, 96, 149, 221, and 397 in the CT. Corresponding percentiles in the OS were 291, 571, 748, 1,074, and 1,693 for calcium, and 43, 93, 147, 225, and 407 for vitamin D, very similar to those in the CT. It is evident that personal supplement use of 500 mg/day or more calcium and 400 IU/day or more of vitamin D contributes a substantial fraction to the total consumption of these nutrients in study cohorts.
Table 2 also shows that total mortality was somewhat reduced in the first 2 years from randomization among women assigned to active treatment in the CT. This pattern was not evident in later years of follow-up, in corresponding OS analyses, or in combined CT and OS analyses.
Table 3 provides corresponding analyses for cardiovascular diseases. There was little evidence for an adverse influence of CaD supplementation on the risk for MI, CHD, total heart disease, stroke, or total cardiovascular disease, from either the CT or OS, or from their combined analysis. In fact, the OS data alone suggest a reduction in total heart disease risk and total cardiovascular disease risk among supplement users.
Table 4 presents corresponding analyses for invasive cancer. Among women with no personal supplements at baseline, there was some evidence for a reduction in breast cancer risk (HR 0.80; 95 % CI, 0.66 to 0.96, P = 0.02) and total cancer risk (HR 0.88, 95 % CI, 0.78 to 0.98, P = 0.03), with little suggestion of HR time trend and with no support from OS data. These patterns were similar in the trial cohort as a whole, but far from significant.
Table 5 presents HRs from the OS for calcium-only and for vitamin D-only supplementation. HRs for calcium plus vitamin D are also repeated from earlier tables for comparative purposes. As mentioned previously, these HRs are subject to residual confounding and other biases, but comparative HRs across supplement types presumably less so. Significant associations were not found for hip fracture or for total fracture for either supplement alone or combined. No associations of calcium or vitamin D with incidence for the specific cancer sites considered or for total invasive cancer were suggested by these Table 5 analyses. A non-significant early elevation in MI incidence with vitamin D is not precisely estimated and is not apparent with the combination of calcium and vitamin D. HR estimates were below one (P < 0.05) for calcium alone in relation to MI and CHD, and as previously mentioned, for CaD in relation to total heart disease.
Data on adherence to assigned supplement category is important for the interpretation of Table 5 analyses. Following the baseline assessment, data on supplement use in the OS was collected only in conjunction with a clinic visit 3 years later. Of the OS women using calcium plus vitamin D at baseline, a substantial 80.9 % reported continued use 3 years later, with 10.9 % stopping use of both of these supplements, 6.9 % moving to calcium-only, and 1.4 % moving to vitamin D-only supplements. In contrast among baseline calcium-only users, a remarkable 57.1 % had moved to CaD preparations by 3 years later, with only 23.7 % still using calcium only, and 17.6 % had stopped using either supplement. Similarly 56.5 % of baseline vitamin D users had moved to CaD by 3 years later, with only 16.4 % still using vitamin D only. Equally impressive, only 49.9 % of baseline non-users of these supplements retained that status 3 years later, with 38.7 % becoming CaD users. It is evident that the contrasts presented in Table 5 primarily pertain to CaD use, and even then the non-user control group evidently becomes quite contaminated over the follow-up period.
Table 6 shows HR estimates from the CT using follow-up data from each participating woman only during the period of time that she remained adherent to her assigned active CaD or placebo pills. Among adherent women, hip fracture risk was lower in the active treatment group both in the overall trial cohort (P = 0.05), and in the subset of women without personal supplements (P = 0.04). The HR (95 % CI) among adherent women not using personal supplements was an impressive 0.24 (0.07, 0.84) following 5 or more years of use among women not using personal supplements. The myocardial infarction HR (95 % CI) was a non-significant 1.18 (0.88, 1.59) among women not using personal calcium or vitamin D. In contrast, breast and total invasive cancer risks were reduced (both P = 0.01) among women adherent to CaD in these analyses. Analyses that incorporated inverse adherence probability weights were similar with overall test P values among women not using personal supplements of 0.02 for hip fracture, 0.98 for MI, 0.06 for invasive breast cancer, and 0.01 for total invasive cancer.
For completeness, corresponding analyses were also carried out for the complementary subset of 20,275 CT women who reported taking personal supplements of calcium or vitamin D, or both, at the time of WHI enrollment. Overall, HRs (95 % CI) in this subset were as follows: hip fracture 0.90 (0.69,1.17), total fracture 0.95 (0.87,1.02), MI 0.97 (0.80,1.17), CHD 1.01 (0.85,1.20), total heart disease 1.04 (0.94,1.16), stroke 0.83 (0.67,1.01), total cardiovascular disease 0.99 (0.90,1.08), colorectal cancer 1.32 (0.98, 1.79), breast cancer 1.09 (0.93,1.28), total invasive cancer 1.04 (0.94,1.15), and death 0.91 (0.79,1.04). None of these HRs differ significantly from unity, though for some outcomes, there is a significant HR difference between the personal supplements and no personal supplements subsets, including stroke (P = 0.04), colorectal cancer (P = 0.04), breast cancer (P = 0.01), and total invasive cancer (P = 0.03).
Among women who were adherent to study pills, the overall HRs (95 % CIs) in the personal supplements user subset were as follows: hip fracture 0.85 (0.58,1.24), total fracture 0.97 (0.87,1.07), MI 0.96 (0.74,1.26), CHD 1.00 (0.79,1.28), total heart disease 1.05 (0.91,1.21), stroke 0.81 (0.60,1.08), total cardiovascular disease 1.01 (0.89,1.14), colorectal cancer 1.17 (0.78,1.73), breast cancer 1.04 (0.85,1.29), total invasive cancer 1.02 (0.90,1.17), and death 0.91 (0.74,1.11). There was significant adherent HR variation between the personal supplements and no personal supplements subsets only for breast cancer (P = 0.03) and total invasive cancer (P = 0.03) in these adherence-adjusted analyses.
Concerning urinary tract stones, as previously reported [1, 7] 449 women (0.35 %) in the group randomized to CaD and 381 women (0.30 %) in the placebo group developed urinary tract stones during the trial intervention period, leading to an HR (95 % CI) of 1.17 (1.02, 1.34). Among adherent women, the HR (95 % CI) was 1.21 (0.98, 1.50). These analyses were repeated here, separately for the no personal supplements and personal supplements groups.
In the no personal supplements subset, the HR (95 % CI) was 1.08 (0.88,1.32) based on 199 women developing urinary tract stones in the active treatment group and 180 in the placebo group. The corresponding HR (95 % CI) in the personal supplements subset was 1.23 (1.01, 1.48) based on 239 and 197 women with stones in the active and placebo groups. The HRs did not differ significantly (P = 0.39) between the two subsets. Among adherent women, the HR (95 % CI) was 1.21 (0.87, 1.69) in the no personal supplements group and 1.19 (0.89, 1.58) in the personal supplements group, with no evidence (P = 0.87) for difference between the HRs for adherent women between the two subsets.
Subset analyses by age group or by prior CVD history were generally similar to those for the overall cohorts for the various outcomes considered above and are not shown.
Discussion
Our further analyses of WHI calcium and vitamin D trial data, through the end of the intervention period, along with corresponding and combined analyses using the WHI observational study, yields few clear clinical effects for daily 1,000 mg calcium plus 400 IU of vitamin D.
The strongest evidence for benefit is for hip fracture where calcium and vitamin D supplementation yielded a noteworthy reduction after 5 years of treatment among women not taking personal supplements, with HR (95 % CI) of 0.62 (0.38, 1.00). It is important to note that hip fracture was the sole primary outcome in the CaD trial, reducing multiple testing limitations. Nevertheless, a cautious interpretation is needed since this is a finding in the no personal supplements subset, while the corresponding overall trial result (HR of 0.82, 95 % CI of 0.61 to 1.12) is not significant. However, the likelihood of a hip fracture risk reduction is enhanced by a significant (P = 0.02) trend of reducing HR with duration of supplementation in the no personal supplements group and by nominally significant risk reductions over the entire follow-up period among adherent women, both in the overall trial cohort and in the no personal supplements subset (Table 6). For example, these adherence-adjusted analyses yield an HR (95 % CI) of 0.24 (0.07, 0.84) following 5 or more years of use among women in the no personal supplements group, suggesting that the public health implications of supplementation could be substantial. Moreover, the biological plausibility of this finding is also supported by higher (P < 0.01) hip bone mineral density (BMD) in the active treatment versus placebo group at 2, 5, and 8 years of follow-up [1]. Supplementary Figure 1 shows average hip, spine, and whole body BMD at baseline, and at 2, 5, and 8 years later, by randomization group, overall, and in the subset of women not using personal supplements, with and without restriction to women adhering to assigned study pills. A larger hip BMD in the intervention group is evident overall, and among women not taking personal supplements, and the difference is enhanced among adherent women.
WHI data provide little support for an influence of calcium and vitamin D supplementation on coronary heart disease risk or cardiovascular disease risk more generally. Women randomized to CaD do not have a significantly elevated risk of MI, CHD, total heart disease, stroke or total cardiovascular disease, either overall or in the subset not using supplements at baseline. Furthermore, any suggestion of an early MI elevation is dampened by multiple testing considerations, since none of the several cardiovascular disease categories considered were among the designated primary or secondary trial outcome and any such suggestion was not enhanced by restriction to women who adhered to study medications. Also, there was no suggested MI elevation in the OS. Moreover, in the analyses of 754 women in the CaD trial who underwent cardiac CT scans for assessment of coronary artery calcium (CAC) scores at trial completion, no association between CaD supplementation and CAC was observed, irrespective of baseline intake of calcium and/or vitamin D [31]. However, given concern about an elevation in MI with calcium use based on other data sources [8], one should keep in mind the possibility of an early MI elevation, but this hypothesis derives little support from WHI data.
The analyses of CaD trial data suggest possible reductions for invasive cancer with supplementation [3, 8]. Such HR reductions are nominally significant for invasive breast cancer (P = 0.02) and for total invasive cancer (P = 0.03) among women not using personal supplements, and these reductions persisted following restriction to adherent women. However, corresponding HR reductions were not significant for the trial cohort as a whole. The fact that HRs for both breast cancer and total cancer differed significantly between the personal supplements and no personal supplements groups could reflect HRs that are below unity at lower calcium and vitamin D doses, and that flatten out at larger doses so that women using personal supplements may have already achieved any cancer risk reduction from supplementation, with little or no further benefit from further supplementation. While this possibility is intriguing, and potentially of public health importance, breast and total cancer were not among the designated primary or secondary outcomes for the CaD, so multiple testing considerations, in conjunction with subset analysis and other [3] considerations cause us to take a cautious interpretation of these analyses. Hence, we regard the WHI data as merely suggestive of invasive breast and total invasive cancer risk reduction with available data.
Consistent with our previous report [7], we find no statistically significant association between CaD supplementation and death in the CaD trial overall or in the subgroup not using personal supplements. There was no evidence in either the CaD trial or the OS that long-term (≥5 years) CaD supplementation reduced the risk of death. Specifically, the CaD intervention did not affect death from coronary heart disease where the hazard ratio was 0.99 (95 % CI, 0.71, 1.38) [7].
With this background, the only documented risk associated with the randomized intervention in the CaD trial is a modest elevation (HR of 1.17, 95 % CI from 1.02 to 1.34) in urinary tract stone occurrence that did not differ significantly between the personal supplements and no personal supplements subsets.
Observational data have several limitations in addressing these types of research questions. For outcomes, such as hip fractures and heart disease, where calcium and/or vitamin D from foods or supplements may have developed a reputation as potential disease preventatives, observational studies not only need to control for standard confounding factors, but also for factors related to confounding by indication since persons at elevated risk for these diseases may self-select, or preferentially be prescribed, these supplements. On the other hand, women using dietary supplements are typically health conscious and may have favorable risk factor profiles for some study diseases. The extent to which confounding control efforts are adequate in such challenging settings is usually unknown. In fact, we see evidence of differing HRs for calcium plus vitamin D from the CaD trial and the OS in Tables 2, 3, and 4 (i.e., HR in OS/HR in CT differs from unity) for several outcomes including total fracture, total heart disease, total cardiovascular disease, and breast cancer. Even though some of these differences may arise from differential adherence to supplementation, they reinforce the need for a cautious approach to interpreting observational associations of this type. Here, inclusion of the OS data did not lead to any new findings but did contribute to evidence for a hip fracture reduction, via our conservative combined clinical trial and observational study data analyses.
Even though there is intense interest in the health effects of supplementation using higher doses than 400 IU/day of vitamin D, the WHI cohorts simply do not have enough women using higher doses to attempt any meaningful analyses.
In summary, WHI clinical trial data are mostly null or inconclusive concerning the health effects of calcium and vitamin D supplementation. Compared to previous WHI reports, the analyses presented here include a focus on whether or not women were using personal supplements at the time of WHI enrollment and a focus on temporal HR patterns across the trial intervention period, leading to more compelling evidence for a hip fracture risk reduction benefit that is somewhat offset by a previously reported elevation in urinary tract stones. Ultimate health benefits versus risks assessment for this intervention could be favorably affected by a reduction in invasive cancer, though evidence is only suggestive at present, while data from other sources suggesting adverse cardiovascular effects of calcium supplementation do not receive support from WHI data. Decisions concerning supplementation with this combination may depend on many factors, including age and sex, and importantly, risk for outcomes affected by CaD. Given the widespread use of these supplements in the USA and elsewhere, it will be important to continue to acquire data to refine estimates of health benefits and risks among postmenopausal women, and other societal groups, and to extend results to other supplementation doses.
References
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, Bonds DE, Brunner RL, Brzyski RG, Caan B, Cauley JA, Chlebowski RT, Cummings SR, Granek I, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Johnson KC, Judd H, Kotchen JM, Kuller LH, Langer RD, Lasser NL, Limacher MC, Ludlam S, Manson JE, Margolis KL, McGowan J, Ockene JK, O'Sullivan MJ, Phillips L, Prentice RL, Sarto GE, Stefanick ML, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson GL, Assaf AR, Barad D, Investigators W's H I (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354:669–683
Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O'Sullivan MJ, Margolis KL, Ockene JK, Phillips L, Pottern L, Prentice RL, Robbins J, Rohan TE, Sarto GE, Sharma S, Stefanick ML, Van Horn L, Wallace RB, Whitlock E, Bassford T, Beresford SA, Black HR, Bonds DE, Brzyski RG, Caan B, Chlebowski RT, Cochrane B, Garland C, Gass M, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Jackson RD, Johnson KC, Judd H, Kooperberg CL, Kuller LH, LaCroix AZ, Lane DS, Langer RD, Lasser NL, Lewis CE, Limacher MC, Manson JE, Investigators W's H I (2006) Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med 354:684–696
Chlebowski RT, Johnson KC, Kooperberg C, Pettinger M, Wactawski-Wende J, Rohan T, Rossouw J, Lane D, O'Sullivan MJ, Yasmeen S, Hiatt RA, Shikany JM, Vitolins M, Khandekar J, Hubbell FA, Investigators W’s H I (2008) Calcium and vitamin D supplementation and the risk of breast cancer. J Natl Cancer Inst 100:1581–1591
Brunner RL, Wactawski-Wende J, Caan BJ, Cochrane BB, Chlebowski RT, Gass ML, Jacobs ET, LaCroix AZ, Lane D, Larson J, Margolis KL, Millen AE, Sarto GE, Vitolins MZ, Wallace RB (2011) The effect of calcium plus vitamin D on risk for invasive cancer: results of the Women's Health Initiative (WHI) calcium plus vitamin D randomized clinical trial. Nutr Cancer 63:827–841
Hsia J, Heiss G, Ren H, Allison M, Dolan NC, Greenland P, Heckbert SR, Johnson KC, Manson JE, Sidney S, Trevisan M, for the Women's Health Initiative Investigators (2007) Calcium/vitamin D supplementation and cardiovascular disease in women. Circulation 115:846–854
LaCroix AZ, Kotchen J, Anderson G, Brzyski R, Cauley JA, Cummings SR, Gass M, Johnson KC, Ko M, Larson J, Manson JE, Stefanick ML, Wactawski-Wende J (2009) Calcium plus vitamin D supplementation and mortality in postmenopausal women: the Women's Health Initiative calcium-vitamin D randomized controlled trial. J Gerontol A Biol Sci Med Sci 64:559–567
Wallace RB, Wactawski-Wende J, O’Sullivan MJ, Larson JC, Cochrane B, Gass M, Masaki K (2011) Urinary tract stone occurrence in the Women's Health Initiative randomized controlled trial of calcium and vitamin D supplements. Am J Clin Nutr 94:270–277
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR (2011) Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited dataset and meta-analysis. BMJ 342:d2040. doi:10.1136/bmj.d2040
Bolland MJ, Grey A, Gamble GD, Reid IR (2011) Calcium and vitamin D supplements and health outcomes: a reanalysis of the Women's Health Initiative (WHI) limited-access dataset. Am J Clin Nutr 94:1144–1149
Chlebowski RT, Pettinger M, Kooperberg C (2011) Caution in reinterpreting the Women's Health Initiative (WHI) calcium and vitamin D trial breast cancer results. Am J Clin Nutr. doi:3945/ajcn.111.027664
Iso H, Stampfer MJ, Manson JE, Rexrode K, Hennekens CH, Colditz GA, Speizer FE, Willett WC (1999) Prospective study of calcium, potassium and magnesium intake and risk of stroke in women. Stroke 30:1772–1779
Bostick RM, Kushi LH, Wu Y, Meyer KA, Sellers TA, Folsom AR (1999) Relation of calcium, vitamin D and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am J Epidemiol 149:151–161
Al-Delaimy WK, Rimm E, Willett WC, Stampfer MJ, Hu FB (2003) A prospective study of calcium intake from diet and supplements and risk of ishemic heart disease among men. Am J Clin Nutr 77:814–818
Ascherio A, Rimm EB, Hernán MA, Giovannucci EL, Kawachi I, Stampfer MJ, Willett WC (1998) Intake of potassium, magnesium, calcium and fiber and risk of stroke among US men. Circulation 98:1198–1204
Kuanrong L, Kaaks R, Linseisen J, Rohrmann S (2011) Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart 98:920–925
Neuhouser ML (2003) Dietary supplement use by American women: challenges in assessing patterns of use, motives and costs. J Nutr 133:1992S–1996S
Neuhouser ML, Patterson RE, Levy L (1999) Motivations for using vitamin and mineral supplements. J Am Diet Assoc 99:851–854
Prentice RL, Langer R, Stefanick M, Howard B, Pettinger M, Anderson G, Barad D, Curb D, Kotchen J, Kuller L, Limacher M, Wactawski-Wende J, for the Women's Health Initiative Investigators (2005) Combined postmenopausal hormone therapy and cardiovascular disease: toward resolving the discrepancy between Women's Health Initiative Clinical Trial and Observational Study Results. Am J Epidemiol 162:404–414
Prentice RL, Langer R, Stefanick ML, Howard BV, Pettinger M, Anderson G, Barad D, Curb JD, Kotchen J, Kuller L, Limacher M, Wactawski-Wende J, for the Women's Health Initiative Investigators (2006) Combined analysis of Women's Health Initiative observational and clinical trial data on postmenopausal hormone treatment and cardiovascular disease. Am J Epidemiol 163:589–599
Prentice RL, Chlebowski RT, Stefanick ML, Manson JE, Langer RD, Pettinger M, Hendrix SL, Hubbell FA, Kooperberg C, Kuller LH, Lane DS, McTiernan A, O'Sullivan MJ, Rossouw JE, Anderson GL (2008) Conjugated equine estrogens and breast cancer risk in the Women's Health Initiative clinical trial and observational study. Am J Epidemiol 167:1407–1415
Prentice RL, Chlebowski RT, Stefanick ML, Manson JE, Pettinger M, Hendrix SL, Hubbell FA, Kooperberg C, Kuller LH, Lane DS, McTiernan A, O’Sullivan MJ, Rossouw JE, Anderson GL (2008) Estrogen plus progestin therapy and breast cancer in recently postmenopausal women. Am J Epidemiol 167:1207–1216
Prentice RL, Pettinger M, Beresford SA, Wactawski-Wende J, Hubbell FA, Stefanick ML, Chlebowski RT (2009) Colorectal cancer in relation to postmenopausal estrogen and estrogen plus progestin in the Women's Health Initiative clinical trial and observational study. Cancer Epidemiol Biomarkers Prev 18:1531–1537
Prentice RL, Manson JE, Langer RD, Anderson GL, Pettinger M, Jackson RD, Johnson KC, Kuller LH, Lane DS, Wactawski-Wende J, Brzyski R, Allison M, Ockene J, Sarto G, Rossouw JE (2009) Benefits and risks of postmenopausal hormone therapy when it is initiated soon after menopause. Am J Epidemiol 170:12–23
Women’s Health Initiative Study Group (1998) Design of the Women's Health Initiative Clinical Trial and Observational Study. Control Clin Trials 19:61–109
Jackson RD, LaCroix AZ, Cauley JA, McGowan J (2003) The Women's Health Initiative calcium-vitamin D trial: overview and baseline characteristics of participants. Ann Epidemiol 13:S98–S106
Langer RD, White E, Lewis CE, Kotchen JM, Hendrix SL, Trevisan M (2003) The Women's Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol 13:S107–S121
Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, Johnson KC, Proulx-Burns L, Pastore L, Criqui M, Daugherty S, Morbidity WHI, Committee M (2003) Outcomes ascertainment and adjudication methods in the Women's Health Initiative. Ann Epidemiol 13:S122–S128
Patterson RE, Levy L, Tinker LF, Kristal AR (1999) Evaluation of a simplified vitamin supplement inventory developed for the Women's Health Initiative. Public Health Nutr 2:273–276
Patterson RE, Kristal AR, Levy L, McLerran D, White E (1998) Validity of methods used to assess vitamin and mineral supplement use. Am J Epidemiol 148:643–649
Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T (1999) Measurement characteristics of the Women's Health Initiative food frequency questionnaire. Ann Epidemiol 9:178–187
Manson JE, Allison MA, Carr JJ, Langer RD, Cochrane BB, Hendrix SL, Hsia J, Hunt JR, Lewis CE, Margolis KL, Robinson JG, Rodabough RJ, Thomas AM (2010) Calcium/vitamin D supplementation and coronary artery calcification. Menopause 17:683–691
Acknowledgments
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller
Clinical Coordinating Center: Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg
Investigators and Academic Centers: (Brigham and Women's Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
Women's Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
For a list of all the investigators who have contributed to WHI science, please visit: https://cleo.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
Funding/Support
This work was partially supported by a grant from the National Osteoporosis Foundation. This sponsor was not involved in decisions concerning data analyses to be conducted, their interpretation, or in manuscript development. The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts N01WH22110, 24152, 32100–2, 32105–6, 32108–9, 32111–13, 32115, 32118–32119, 32122, 42107–26, 42129–32, and 44221. Related data analytic methodology work was supported by NIH grant CA53996.
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
Modeled regression variables by clinical outcome included in WHI Observational Study component of analyses. Additionally, in both the Clinical Trial and Observational Study, baseline Cox model hazard rates are stratified on cohort (CT versus OS), baseline age (5-year categories), and current use of postmenopausal estrogens and of estrogens plus progestins. Additional modeled regression variables in both the CT and OS included prior use of estrogens and of estrogens plus progestins, duration of any such prior use, and FFQ estimates of usual dietary consumption of calcium and vitamin D. (DOCX 20 kb)
Supplementary Figure 1
Bone mineral density averages and 95 % confidence intervals by randomization group in the WHI Calcium and Vitamin D trial: Averages are presented at baseline (Clinical Trial Year 1) and 2, 5, and 8 years later (DOCX 856 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Prentice, R.L., Pettinger, M.B., Jackson, R.D. et al. Health risks and benefits from calcium and vitamin D supplementation: Women's Health Initiative clinical trial and cohort study. Osteoporos Int 24, 567–580 (2013). https://doi.org/10.1007/s00198-012-2224-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2224-2