Abstract
Summary
In vivo hr-pQCT precision was determined in 42 postmenopausal women using double baseline measurements from a multicenter trial of odanacatib. Errors, e.g., at the radius below 1.3% for BMD and below 6.3% for trabecular structure, were comparable to single-center results. Motion artifacts remain a challenge, particularly at the forearm.
Introduction
The short-term in vivo precision of BMD, trabecular bone structure, cortical thickness and porosity of the forearm and tibia was measured by hr-pQCT. Also the effect of image quality on precision was evaluated.
Methods
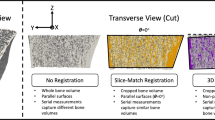
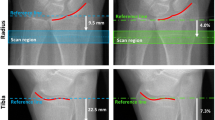
In 42 postmenopausal women (age 64.4 ± 6.8 years) out of 214 subjects enrolled in a multi center advanced imaging phase III study of odanacatib (DXA spine or hip T-scores between −1.5 and −3.5), double baseline hr-pQCT (XtremeCT) measurements with repositioning were performed. The standard ultradistal location and a second, more proximally located VOI were measured at the radius and tibia to better assess cortical thickness and porosity. Image analysis and quality grading (grades: perfect, slight artifacts, pronounced artifacts, unacceptable) were performed centrally.
Results
At the radius RMS%CV values varied from 0.7% to 1.3% for BMD and BV/TV and from 5.6% to 6.3% for Tb.Sp, Tb.Th, Tb.N, and cortical porosity. Numerically at the tibia, precision errors were approx. 0.5% lower for BMD and 1% to 2% lower for structural parameters although most differences were insignificant. In the radius but not in the tibia, precision errors for cortical thickness were smaller at the distal compared to the ultradistal location (1% versus 2%).
Conclusions
BMD precision errors were lower than those for trabecular architecture and cortical porosity. Motion artifacts remain a challenge, particularly at the forearm. Quality grading remains subjective, and more objective evaluation methods are needed. Precision in the context of a multicenter clinical trial, with centralized training and scan analysis, was comparable to single-center results previously reported.



Similar content being viewed by others
References
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90(12):6508–6515
Laib A, Hauselmann HJ, Ruegsegger P (1998) In vivo high resolution 3D-QCT of the human forearm. Technol Health Care 6(5–6):329–337
Müller R, Hildebrand T, Häuselmann HJ, Rüegsegger P (1996) In vivo reproducibility of noninvasive bone biopsies using 3d-pQCT. J Bone Miner Res 11:1745–1750
Burghardt AJ, Buie HR, Laib A, Majumdar S, Boyd SK (2010) Reproducibility of direct quantitative measures of cortical bone microarchitecture of the distal radius and tibia by HR-pQCT. Bone 47(3):519–528
Buie HR, Campbell GM, Klinck RJ, MacNeil JA, Boyd SK (2007) Automatic segmentation of cortical and trabecular compartments based on a dual threshold technique for in vivo micro-CT bone analysis. Bone 41(4):505–515
Burghardt AJ, Kazakia GJ, Majumdar S (2007) A local adaptive threshold strategy for high resolution peripheral quantitative computed tomography of trabecular bone. Ann Biomed Eng 35(10):1678–1686
MacNeil JA, Boyd SK (2007) Accuracy of high-resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys 29(10):1096–1105
XtremeCT User’s Guide, Revision 5.05 (2005) SCANCO MEDICAL AG, Bassersdorf Switzerland
Mueller TL, Stauber M, Kohler T, Eckstein F, Muller R, van Lenthe GH (2009) Non-invasive bone competence analysis by high-resolution pQCT: an in vitro reproducibility study on structural and mechanical properties at the human radius. Bone 44(2):364–371
MacNeil JA, Boyd SK (2008) Improved reproducibility of high-resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys 30(6):792–799
Kazakia GJ, Hyun B, Burghardt AJ, Krug R, Newitt DC, de Papp AE, Link TM, Majumdar S (2008) In vivo determination of bone structure in postmenopausal women: a comparison of HR-pQCT and high-field MR imaging. J Bone Miner Res 23(4):463–474
Swinford RR, Warden SJ (2010) Factors affecting short-term precision of musculoskeletal measures using peripheral quantitative computed tomography (pQCT). Osteoporos Int 21(11):1863–1870
Grampp S, Lang P, Jergas M, Gluer CC, Mathur A, Engelke K, Genant HK (1995) Assessment of the skeletal status by peripheral quantitative computed tomography of the forearm: short-term precision in vivo and comparison to dual X-ray absorptiometry. J Bone Miner Res 10(10):1566–1576
Koenig C, Wey H, Binkley T (2008) Precision of the XCT 3000 and comparison of densitometric measurements in distal radius scans between XCT 3000 and XCT 2000 peripheral quantitative computed tomography scanners. J Clin Densitom 11(4):575–580
Engelke K, Libanati C, Liu Y, Wang H, Austin M, Fuerst T, Stampa B, Timm W, Genant HK (2009) Quantitative computed tomography (QCT) of the forearm using general purpose spiral whole-body CT scanners: accuracy, precision and comparison with dual-energy X-ray absorptiometry (DXA). Bone 45(1):110–118
Eisa F, Museyko O, Hess A, Kalender WA, Engelke K (2010) Comparison of anatomic coordinate systems with rigid multi-resolution 3D registration for the reproducible positioning of analysis volumes of interest in QCT. Phys Med Biol 55(5):1429–1439
Sode M, Burghardt AJ, Pialat JB, Link TM, Majumdar S (2011) Quantitative characterization of subject motion in HR-pQCT images of the distal radius and tibia. Bone 48(6):1291–1297
Fuerst T, Engelke K, Mc Cracken P, Stampa B, Timm W, Dardzinski B, Genant HK, De Papp A (2010) Short term in vivo precision of BMD and parameters of trabecular architecture at the distal forearm and tibia. In 32th Annual Meeting of the American Society for Bone and Mineral Research. Toronto, Canada: JBMR
Acknowledgments
This study was sponsored by Merck & Co., centralized quality control and analysis were performed by Synarc Inc. The following investigators provided data for this study: K. Brixen, Odense University Hospital, Denmark; R. Charpurlat, University of Lyon, France; A. Cheung, University of Toronto, Canada; D. Felsenberg, Charité Berlin, Germany; D. Hanley, University of Calgary, Canada; S. Majumdar, University of California at San Francisco, USA; T. Thomas, University of St. Etienne, France; D. Übelhardt, University Hospital Zürich, Switzerland; and M-C de Vernejoul, Hôpital Lariboisière Paris, France. Preliminary results have been presented at the ASBMR 2010 [18].
Conflicts of interest
Apart from being employees of Synarc (BS, WT, KE, TF) or of Merck (BD, AP), the authors have no conflicts of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Engelke, K., Stampa, B., Timm, W. et al. Short-term in vivo precision of BMD and parameters of trabecular architecture at the distal forearm and tibia. Osteoporos Int 23, 2151–2158 (2012). https://doi.org/10.1007/s00198-011-1829-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1829-1