Abstract
Introduction and hypothesis
Lower urinary tract symptoms (LUTS) are common among adolescent girls. Physical activity (PA) has been implicated as both a risk (high-impact PA) and protective factor (low-impact, moderate to vigorous intensity PA) for LUTS in adult women, but its role in adolescent girls is unclear. This study investigated the prospective association between physical activity and LUTS risk in adolescent girls.
Methods
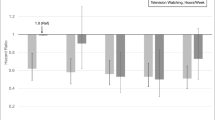
The sample comprised 3,484 female participants in the Avon Longitudinal Study of Parents and Children. Multivariate logistic regression models were used to examine daily minutes of moderate to vigorous PA (MVPA) at ages 11 and 15 years in relation to LUTS at ages 14 and 19 respectively. MVPA was assessed by 7-day accelerometer data. LUTS were assessed by questionnaire. MVPA were analyzed as continuous (minutes/day) and categorical variables (<10th percentile, 10–89th percentile, ≥90th percentile).
Results
Prevalence of LUTS ranged from 2.0% for bedwetting to 9.5% for nocturia at age 14 and from 2.0% for straining to urinate to 35.5% for interrupted urine flow at age 19. Physical activity was not associated with LUTS at either time-point.
Conclusions
Given the prevalence of LUTS in female adolescent populations, although this study did not find an association with accelerometer-measured MVPA, other aspects of PA that may serve as risk or protective factors deserve investigation.
Similar content being viewed by others
Data Availability
The informed consent obtained from ALSPAC participants does not allow the data to be made freely available through any third party maintained public repository. However, data used for this submission can be made available on request to the ALSPAC Executive. The ALSPAC data management plan describes in detail the policy regarding data sharing, which is through a system of managed open access. Full instructions for applying for data access can be found here: http://www.bristol.ac.uk/alspac/researchers/access/. The ALSPAC study website contains details of all the data that are available (http://www.bristol.ac.uk/alspac/researchers/our-data/).
References
Kyrklund K, Taskinen S, Rintala RJ, Pakarinen MP. Lower urinary tract symptoms from childhood to adulthood: a population based study of 594 Finnish individuals 4 to 26 years old. J Urol. 2012;188(2):588–93.
Tam YH, Ng CF, Wong YS, . Population-based survey of the prevalence of lower urinary tract symptoms in adolescents with and without psychotropic substance abuse. Hong Kong Med J. 2016;22(5):454–63.
Serdinsek T, Sobocan M, But S, Spilak-Gomboc M, But I. Lower urinary tract symptoms in adolescent girls: a questionnaire-based study. Eur J Obstet Gynecol Reprod Biol. 2021;258:452–6.
Heron J, Grzeda MT, von Gontard A, Wright A, Joinson C. Trajectories of urinary incontinence in childhood and bladder and bowel symptoms in adolescence: prospective cohort study. BMJ Open. 2017;7(3): e014238.
Alnaif B, Drutz HP. The prevalence of urinary and fecal incontinence in Canadian secondary school teenage girls: questionnaire study and review of the literature. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(2):134–7; discussion 138.
Luo Y, Zou P, Wang K, Cui Z, Li X, Wang J. Prevalence and associated factors of urinary incontinence among Chinese adolescents in Henan province: a cross-sectional survey. Int J Environ Res Public Health. 2020;17(17):6106.
Schwartz B, Wyman JF, Thomas W, Schwarzenberg SJ. Urinary incontinence in obese adolescent girls. J Pediatr Urol. 2009;5(6):445–50.
Camenga DR, Wang Z, Chu H, et al. Sexual health behaviors by age 17 and lower urinary tract symptoms at age 19: Plus research consortium analysis of ALSPAC data. J Adolesc Health. 2023;72(5):737–45.
Alhababi N, Magnus MC, Joinson C, Fraser A. A prospective study of the association between physical activity and lower urinary tract symptoms in parous middle-aged women: results from the Avon Longitudinal Study of Parents and Children. J Urol. 2019;202(4):779–86.
Rebullido TR, Gomez-Tomas C, Faigenbaum AD, Chulvi-Medrano I. The prevalence of urinary incontinence among adolescent female athletes: a systematic review. J Funct Morphol Kinesiol. 2021;6(1):12.
Carls C. The prevalence of stress urinary incontinence in high school and college-age female athletes in the midwest: Implications for education and prevention. Urol Nurs. 2007;27(1):21–4, 39.
Nygaard IE, Thompson FL, Svengalis SL, Albright JP. Urinary incontinence in elite nulliparous athletes. Obstet Gynecol. 1994;84(2):183–7.
Nygaard IE, Shaw JM. Physical activity and the pelvic floor. Am J Obstet Gynecol. 2016;214(2):164–71.
De Mattos Lourenco TR, Matsuoka PK, Baracat EC, Haddad JM. Urinary incontinence in female athletes: a systematic review. Int Urogynecol J. 2018;29(12):1757–63.
Kandola A, Lewis G, Osborn DPJ, Stubbs B, Hayes JF. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: a prospective cohort study. Lancet Psychiatry. 2020;7(3):262–71.
Ng QX, Ho CYX, Chan HW, Yong BZJ, Yeo WS. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: a systematic review. Complement Ther Med. 2017;34:123–8.
Boyd A, Golding J, Macleod J, et al. Cohort profile: the "children of the 90s"–the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42(1):111–27.
Fraser A, Macdonald-Wallis C, Tilling K, et al. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2013;42(1):97–110.
Northstone K, Lewcock M, Groom A, et al. The Avon Longitudinal Study of Parents and Children (ALSPAC): an update on the enrolled sample of index children in 2019. Wellcome Open Res. 2019;4:51.
Tobias JH, Steer CD, Mattocks CG, Riddoch C, Ness AR. Habitual levels of physical activity influence bone mass in 11-year-old children from the United Kingdom: findings from a large population-based cohort. J Bone Miner Res. 2007;22(1):101–9.
Mattocks C, Ness A, Leary S, et al. Use of accelerometers in a large field-based study of children: protocols, design issues, and effects on precision. J Phys Act Health. 2008;5(Suppl 1):S98–111.
Shoham DA, Wang Z, Lindberg S, et al. School toileting environment, bullying, and lower urinary tract symptoms in a population of adolescent and young adult girls: preventing lower urinary tract symptoms consortium analysis of Avon Longitudinal Study of Parents and Children. Urology. 2021;151:86–93.
Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. 2004;191(1):73–82.
Swithinbank LV, Heron J, von Gontard A, Abrams P. The natural history of daytime urinary incontinence in children: a large British cohort. Acta Paediatr. 2010;99(7):1031–6.
Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed. Lippincott Williams & Williams; 2008. p. 139.
Brady SS, Berry A, Camenga DR, et al. Applying concepts of life course theory and life course epidemiology to the study of bladder health and lower urinary tract symptoms among girls and women. Neurourol Urodyn. 2020;39(4):1185–202.
Bo K, Sundgot-Borgen J. Are former female elite athletes more likely to experience urinary incontinence later in life than non-athletes? Scand J Med Sci Sports. 2010;20(1):100–4.
Van Hecke L, Loyen A, Verloigne M, et al. Variation in population levels of physical activity in European children and adolescents according to cross-European studies: a systematic literature review within DEDIPAC. Int J Behav Nutr Phys Act. 2016;13:70.
Guinhouya BC, Samouda H, de Beaufort C. Level of physical activity among children and adolescents in Europe: a review of physical activity assessed objectively by accelerometry. Public Health. 2013;127(4):301–11.
Steene-Johannessen J, Hansen BH, Dalene KE, et al. Variations in accelerometry measured physical activity and sedentary time across Europe—harmonized analyses of 47,497 children and adolescents. Int J Behav Nutr Phys Act. 2020;17(1):38.
Acknowledgements
We are extremely grateful to all the families who took part in the ALSPAC study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. Prevention of Lower Urinary Tract Symptoms (PLUS) Research Consortium Research Centers and Investigators: Loyola University Chicago, Maywood, IL, USA (U01DK106898); multi-principal investigators: Linda Brubaker, Elizabeth R. Mueller; investigators: Marian Acevedo-Alvarez, Colleen M. Fitzgerald, Cecilia T. Hardacker, Jeni Hebert-Beirne. Northwestern University—Chicago, IL, USA (U01DK126045): multi-principal investigators: James W. Griffith, Kimberly Sue Kenton, Melissa Simon; investigator: Oluwateniola Brown, Julia Geynisman-Tan, Margaret Mueller. University of Alabama at Birmingham, Birmingham, AL, USA (U01DK106858): principal investigators: Alayne D. Markland, Camille P. Vaughan; investigators: Tamera Coyne-Beasley, Kathryn L. Burgio, Cora E. Lewis, Beverly Rosa Williams. University of California San Diego, La Jolla, CA, USA (U01DK106827): principal investigator: Emily S. Lukacz; investigators: Sheila Gahagan, D. Yvette LaCoursiere, Jesse Nodora. University of Michigan—Ann Arbor, MI, USA (U01DK106893): principal investigator: Lisa Kane Low; investigators: Janis M. Miller, Abby Smith. University of Minnesota (Scientific and Data Coordinating Center), Minneapolis, MN, USA (U24DK106786): multi-principal investigators: Gerald McGwin, Jr., Kyle D. Rudser; investigators: Sonya S. Brady, Haitao Chu, Cynthia S. Fok, Bernard L. Harlow, Peter Scal, Todd Rockwood. University of Pennsylvania, Philadelphia, PA, USA (U01DK106892): multi-principal investigators: Diane K. Newman, Ariana L. Smith; investigators: Amanda Berry, Andrea Bilger, Terri H. Lipman, Heather Klusaritz, Ann E. Stapleton, Jean F. Wyman. Washington University in St. Louis, Saint Louis, MO, USA (U01DK106853): principal investigator: Siobhan Sutcliffe; investigators: Aimee S. James, Jerry L. Lowder, Melanie R. Meister. Yale University, New Haven, CT, USA (U01DK106908): principal investigator: Leslie M. Rickey: investigators: Deepa R. Camenga, Shayna D. Cunningham. Steering Committee Chair: Linda Brubaker, UCSD, San Diego, CA, USA (January 2021–). NIH Program Office: National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urologic, and Hematologic Diseases, Bethesda, MD, USA. NIH Project Scientist: Julia Barthold
Funding
Funding for the ALSPAC study was provided by the UK Medical Research Council and the Wellcome Trust (grant ref: 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. A comprehensive list of grants funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf). This publication is the work of the authors and the authors will serve as guarantors for the contents of this paper. This work was also supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) at the National Institutes of Health (NIH) by cooperative agreements (grants U24DK106786, U01 DK106853, U01 DK106858, U01 DK106898, U01 DK106893, U01 DK106827, U01 DK106908, U01 DK106892, U01 DK126045). Additional funding from: National Institute on Aging, NIH Office of Research on Women’s Health. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Contributions
C.M. Fitzgerald: project development, interpretation of findings, manuscript writing, manuscript editing; S.D. Cunningham: interpretation of findings, manuscript writing, manuscript editing; A. Berry: interpretation of findings, manuscript writing, manuscript editing; S. Gahagan: interpretation of findings, manuscript writing, manuscript editing; C. Joinson: interpretation of findings, manuscript editing. S. Lindberg: data analysis, manuscript writing, manuscript editing; D.K. Newman: interpretation of findings, manuscript writing, manuscript editing; K.H. Schmitz: interpretation of findings, manuscript editing. A.L. Smith: project development, interpretation of findings, manuscript editing; S. Sutcliffe: project development; interpretation of findings, manuscript editing; D.A. Shoham: project development, data analysis, interpretation of findings, manuscript writing, manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
C.M. Fitzgerald: Royalties from UpToDate and Expert Witness. The other authors have no conflicts of interest to the subject matter of the manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fitzgerald, C.M., Cunningham, S.D., Berry, A. et al. Is there an association between physical activity and lower urinary tract symptoms in adolescent girls? Results from the Avon Longitudinal Study of Parents and Children. Int Urogynecol J 34, 2995–3003 (2023). https://doi.org/10.1007/s00192-023-05639-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05639-6