Abstract
Introduction and hypothesis
Following vaginal hysterectomy (VH), fixation of the vaginal vault is needed to prevent post-operative recurrence/exacerbation of vault prolapse. The effectiveness of McCall culdoplasty in cases of advanced prolapse is unclear. We aimed to compare the effectiveness of McCall culdoplasty following VH in patients with mild versus advanced stages of uterine prolapse.
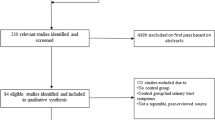
Methods
In this retrospective study, the Pelvic Floor Distress Inventory (PFDI-20) was utilized to compare the subjective results of vaginal hysterectomy plus McCall culdoplasty between women with mild uterine prolapse stage 2 (mild prolapse group) and advanced uterine prolapse stages 3–4 (advanced prolapse group). The primary outcome, the subjective awareness of prolapse, was analyzed as well as all other aspects of PFDI-20. A sample size of 130 was calculated.
Results
The mild prolapse group consisted of 26 (19.3%) patients and the advanced prolapse group consisted of 109 (80.7%) patients. There were no differences between the groups in demographic and clinical characteristics. The rates of concomitant prolapse and incontinence surgeries, performed at the time of VH and post-operative complications. were the same between groups. The mean follow-up was more than 5 years in both groups. Awareness of prolapse was similar between the groups (11.5% in the mild prolapse group and 5.5% in the advanced prolapse group, p = 0.374). There was no significant correlation between the stage of apical prolapse before surgery and awareness of prolapse after the surgery (r = 0.0132, p = 0.879). All aspects of the PFDI-20 questionnaire were similar in the two groups.
Conclusion
McCall culdoplasty was found to have an equal subjective effectiveness following VH in both mild and advanced stages of uterine prolapse.
Similar content being viewed by others
References
Practice Bulletin No. 185: Pelvic organ prolapse. Obstet Gynecol. 2017;130(5):e234–50. https://doi.org/10.1097/aog.0000000000002399.
Mouritsen L, Larsen JP. Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(2):122–7. https://doi.org/10.1007/s00192-002-1024-1.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079. https://doi.org/10.1002/14651858.Cd012079.
Committee Opinion No 701: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2017;129(6):e155–9. https://doi.org/10.1097/aog.0000000000002112.
Blandon RE, Bharucha AE, Melton LJ 3rd, Schleck CD, Babalola EO, Zinsmeister AR, et al. Incidence of pelvic floor repair after hysterectomy: a population-based cohort study. Am J Obstet Gynecol. 2007;197(6):664.e1–7. https://doi.org/10.1016/j.ajog.2007.08.064.
Eilber KS, Alperin M, Khan A, Wu N, Pashos CL, Clemens JQ, et al. Outcomes of vaginal prolapse surgery among female Medicare beneficiaries: the role of apical support. Obstet Gynecol. 2013;122(5):981–7. https://doi.org/10.1097/AOG.0b013e3182a8a5e4.
Kong MK, Bai SW. Surgical treatments for vaginal apical prolapse. Obstet Gynecol Sci. 2016;59(4):253–60. https://doi.org/10.5468/ogs.2016.59.4.253.
Alas A, Chandrasekaran N, Devakumar H, Martin L, Hurtado E, Davila GW. Advanced uterovaginal prolapse: is vaginal hysterectomy with McCall culdoplasty as effective as in lesser degrees of prolapse? Int Urogynecol J. 2018;29(1):139–44. https://doi.org/10.1007/s00192-017-3436-y.
McCall ML. Posterior culdeplasty; surgical correction of enterocele during vaginal hysterectomy; a preliminary report. Obstet Gynecol. 1957;10(6):595–602.
Niblock K, Bailie E, McCracken G, Johnston K. Vaginal McCall culdoplasty versus laparoscopic uterosacral plication to prophylactically address vaginal vault prolapse. Gynecol Surg. 2017;14(1):3. https://doi.org/10.1186/s10397-017-1006-4.
Colombo M, Milani R. Sacrospinous ligament fixation and modified McCall culdoplasty during vaginal hysterectomy for advanced uterovaginal prolapse. Am J Obstet Gynecol. 1998;179(1):13–20.
Chene G, Tardieu AS, Savary D, Krief M, Boda C, Anton-Bousquet MC, et al. Anatomical and functional results of McCall culdoplasty in the prevention of enteroceles and vaginal vault prolapse after vaginal hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(7):1007–11. https://doi.org/10.1007/s00192-007-0549-8.
Madhu C, Swift S, Moloney-Geany S, Drake MJ. How to use the Pelvic Organ Prolapse Quantification (POP-Q) system? Neurourol Urodyn. 2018;37(S6):S39–s43. https://doi.org/10.1002/nau.23740.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Lowenstein L, Levy G, Chen KO, Ginath S, Condrea A, Padoa A. Validation of Hebrew versions of the pelvic floor distress inventory, pelvic organ prolapse/urinary incontinence sexual function questionnaire, and the urgency, severity and impact questionnaire. Female Pelvic Med Reconstr Surg. 2012;18(6):329–31. https://doi.org/10.1097/SPV.0b013e31827268fa.
Sipos AG, Kozma B, Poka R, Larson K, Takacs P. The effect of fractional CO2 laser treatment on the symptoms of pelvic floor dysfunctions: Pelvic Floor Distress Inventory-20 questionnaire. Lasers Surg Med. 2019;51(10):882–6. https://doi.org/10.1002/lsm.23126.
Ho MH, Lin LL, Haessler AL, Bhatia NN. Tension-free transobturator tape procedure for stress urinary incontinence. Curr Opin Obstet Gynecol. 2006;18(5):567–74. https://doi.org/10.1097/01.gco.0000242962.48114.6b.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Alas A, Chandrasekaran N, Devakumar H, Martin L, Hurtado E, Davila GW. Advanced uterovaginal prolapse: is vaginal hysterectomy with McCall culdoplasty as effective as in lesser degrees of prolapse? Int Urogynecol J. 2017;29(1):139–44. https://doi.org/10.1007/s00192-017-3436-y.
Parisi S, Novelli A, Olearo E, Basile A, Puppo A. Traditional McCall culdoplasty compared to a modified McCall technique with double ligament suspension: anatomical and clinical outcomes. Int Urogynecol J. 2020;31(10):2147–53. https://doi.org/10.1007/s00192-020-04403-4.
Barber MD, Brubaker L, Nygaard I, Wheeler TL 2nd, Schaffer J, Chen Z, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9. https://doi.org/10.1097/AOG.0b013e3181b2b1ae.
Contributions
E. Barber: project development, data collection, Manuscript writing; I. Kleiner: data collection; D. Tairy: data collection; J. Bar: project development; S. Ginath: project development, data collection, manuscript writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Authors E. Barber, I. Kleiner, D. Tairy, J. Bar, S. Ginath declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barber, E., Kleiner, I., Tairy, D. et al. The effectiveness of McCall culdoplasty following vaginal hysterectomy in advanced stages of uterine prolapse. Int Urogynecol J 32, 2143–2148 (2021). https://doi.org/10.1007/s00192-021-04890-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04890-z