Abstract
Introduction and hypothesis
This study compared anatomical and clinical outcomes of traditional McCall culdoplasty versus a modified McCall technique with double ligament suspension (DLS).
Methods
This retrospective study presents outcomes of 68 patients who underwent vaginal hysterectomy and vaginal suspension for apical prolapse ≥ stage II according to the POP-Q score system, at, between January 2016 and February 2018. In 34 women vaginal cuff suspension was obtained with traditional McCall culdoplasty (McCall group), while in 34 women we performed a modified McCall, which consists of a double ligament suspension (DLS group), suspending the vaginal cuff to uterosacral ligaments and also to adnexal peduncles. Primary outcome was prolapse recurrence ≥ stage II according to the POP-Q system. Fisher’s, Mann-Whitney U and Student’s t tests were used for statistical analysis.
Results
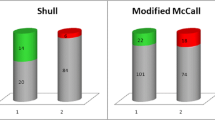
There were no statistical differences among patients’ preoperative characteristics, operative time, blood loss or postoperative complications. Follow-up mean duration was 23.2 ± 6.7 and 22.4 ± 8.7 months in the McCall and DLS group, respectively. Prolapse recurrence occurred in 11 (32.3%) women in the McCall group versus 2 (5.9%) women in the DLS group (p < 0.05): among them, 2 patients (5.9%) in the McCall group and 1 (2.9%) in the DLS group required further treatment. Total vaginal length was 6.1 ± 0.9 cm in the McCall group versus 6.9 ± 0.7 cm in the DLS group (p < 0.001). No statistical difference in quality of life assessment was observed.
Conclusions
DLS group patients had better anatomical outcomes and lower recurrence rates than McCall group patients, without increasing operative time or complications. A prospective study with more cases is needed to confirm our data.


Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Khunda A, Vashisht A, Cutner A. New procedures for uterine prolapse. Best Pract Res Clin Obstet Gynaecol. 2013;27(3):363–79.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6.
Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:437–40.
Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS. Cost of pel- Vic organ prolapse surgery in the United States. Obstet Gynecol. 2001;98:646–51.
Oversand SH, Staff AC, Spydslaug AE, Svennings S, Borstad E. Long-term follow-up after native tissue repair for pelvic organ prolapse. Int Urgynecol J. 2014;25:81–9.
Price N, Slack A, Jwarah E, Jackson S. The incidence of reoperation for surgically treated pelvic organ prolapse: an 11-year experience. Menopause Int. 2008;14(4):145–8.
Jha S, Moran P. The UK national prolapse survey: 5 years on. Int Urogynecol J. 2011;22(5):517–28.
Vanspauwen R, Seman E, Dwyer P. Survey of current management of prolapse in Australia and New Zealand. Aust N Z J Obstet Gynaecol. 2010;50(3):262–7.
Cheon C, Maher C. Economics of pelvic organ prolapse surgery. Int Urogynecol J. 2013;24(11):1873–6.
Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. BJOG. 2005;112:107–11.
Julian TM. The efficacy of Marlex mesh in the repair of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol. 1996;186:1472–5.
Novara L, Sgro LG, Pecchio S, Ottino L, Tomatis V. Biglia N. Transvaginal high uterosacral ligament suspension: an alternative to McCall culdoplasty in the treatment of pelvic organ prolapse. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2019;240:278–81. https://doi.org/10.1016/j.ejogrb.2019.07.007.
Margulies RU, Rogers MA, Morgan DM. Outcomes of transvaginal uterosacral ligament suspension: systematic review and metaanalysis. Am J Obstet Gynecol. 2010 Feb;202(2):124–34. https://doi.org/10.1016/j.ajog.2009.07.052.
Spelzini F, Frigerio M, Manodoro S, Interdonato ML, Cesana MC, Verri D, et al. Modified McCall culdoplasty versus Shull suspension in pelvic prolapse primary repair: a retrospective study. Int Urogynecol J. 2017;28(1):65–71.
Schiavi MC, Savone D, Di Mascio D, Di Tucci C, Perniola G, Zullo MA, et al. Long-term experience of vaginal vault prolapse prevention at hysterectomy time by modified McCall culdoplasty or Shull suspension: clinical, sexual and quality of life assessment after surgical intervention. Eur J Obstet Gynecol Reprod Biol. 2018;223:113–8. https://doi.org/10.1016/j.ejogrb.2018.02.025.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
McCall ML. Posterior culdeplasty; surgical correction of enterocele during vaginal hysterectomy; a preliminary report. Obstet Gynecol. 1957;10:595–602.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193:103–13.
Yazdany T, Bhatia N. Uterosacral ligament vaginal vault suspension: anatomy, outcome and surgical considerations. Curr Opin Obstet Gynecol. 2008;20(5):484–8.
Silva WA, Pauls RN, Segal JL, et al. Uterosacral ligament vault suspension: five-year outcomes. Obstet Gynecol. 2006;108:255–63.
Baden WF, Walker T. Surgical repair of vaginal defects. Philadelphia: The Lippincott Company Ed.; 1992.
Cosma S, Petruzzelli P, Chiadò Fiorio Tin M, Parisi S, Olearo E, Fassio F, Zizzo R, Danese S, Benedetto C. Simplified laparoscopic sacropexy avoiding deep vaginal dissection. Int J Gynaecol Obstet 2018;143(2):239–245. https://doi.org/10.1002/ijgo.12632.
Deo G, Bernasconi DP, Cola A, Palmieri S, Spelzini F, Milani R, et al. Long-term outcomes and five-year recurrence-free survival curves after native-tissue prolapse repair. Int J Gynaecol Obstet. 2019;147:238–45.
Manodoro S, Frigerio M, Milani R, Spelzini F. Tips and tricks for uterosacral ligament suspension: how to avoid ureteral injury. Int Urogynecol J. 2018;29:161–3.
Schulten SFM, Detollenaere RJ, Stekelenburg J, IntHout J, Kluivers KB, van Eijndhoven HWF. Sacrospinous hysteropexy versus vaginal hysterectomy with uterosacral ligament suspension in women with uterine prolapse stage 2 or higher: observational follow-up of a multicentre randomised trial. BMJ. 2019;366:l5149. https://doi.org/10.1136/bmj.l5149.
Morgan DM, Rogers MA, Huebner M, Wei JT, Delancey JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Obstet Gynecol. 2007;109:1424–33.
Acknowledgements
All authors thank Dimitra Barla for her English language editing service in the final revision of the article.
Author information
Authors and Affiliations
Contributions
Silvia Parisi: manuscript writing, data collection and statistical analysis; Antonia Novelli: project development and manuscript writing; Elena Olearo: reviewing and editing the manuscript; Alessandro Basile: data collection; Andrea Puppo: supervision and validation.
Corresponding author
Ethics declarations
Declaration of interest
The authors report no conflicts of interest.
Consent
Written informed consent was obtained from the patient for the publication of Fig. 1.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parisi, S., Novelli, A., Olearo, E. et al. Traditional McCall culdoplasty compared to a modified McCall technique with double ligament suspension: anatomical and clinical outcomes. Int Urogynecol J 31, 2147–2153 (2020). https://doi.org/10.1007/s00192-020-04403-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04403-4