Abstract
Introduction and hypothesis
To analyze the immunochemical and urodynamic outcomes after partial versus complete excision of transvaginal polypropylene mesh (PPM) from pelvic walls of rats.
Methods
Forty-eight female Sprague-Dawley (SD) rats were randomly distributed into seven groups: control, mesh total removal 60 days (M-T 60D), mesh total removal 180 days (M-T 180D), mesh partial removal 60 days (M-H 60D), mesh partial removal 180 days (M-H 180D), sham 60 days (Sham 60D), and sham 180 days (Sham 180D). In the mesh groups, PPM was inserted and partially (0.3 × 0.3 cm) or completely removed 30 days later. In the Sham group, the space between the vagina and bladder was dissected without placing or removing the synthetic mesh at day 1 and day 30 later. Urodynamic studies, immunochemical analysis, and Western blot were done at days 60 and 180.
Results
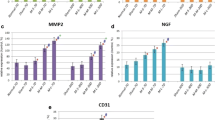
The M-T 60D voiding pressure was significantly decreased compared to the Sham 60D and M-H 60D. The voiding interval of M-T 60D was significantly shorter than that of M-H 60D. In the M-T 60D and M-T 180D groups, the leak point pressure was significantly less than in their corresponding sham groups. IL-1 and TNF-α were significantly more intense in M-T 60D compared to M-H 60D and Sham 60D. NGF was significantly greater in M-T 60D compared to Sham 60D. There were no significant differences in MMP-2 and CD-31s throughout the group.
Conclusion
Total mesh excision incites a host inflammatory response and transitory lower urinary tract dysfunction. Despite the good outcomes after total excision, the invasiveness and surgical risk associated with repeated procedures should not be underestimateded.



Similar content being viewed by others
References
Abbott S, Unger CA, Evans JM, Jallad K, Mishra K, Karram MM, et al. Evaluation and management of complications from synthetic mesh after pelvic reconstructive surgery: a multicenter study. Am J Obstet Gynecol. 2014;210(2):163 e1-8.
Lo TS, Al-Kharabsheh AM, Tan YL, Pue LB, Hsieh WC, Uy-Patrimonio MC. Single incision anterior apical mesh and sacrospinous ligament fixation in pelvic prolapse surgery at 36 months follow-up. Taiwan J Obstet Gynecol. 2017;56(6):793–800.
Lo TS, Pue LB, Tan YL, Wu PY. Long-term outcomes of synthetic transobturator nonabsorbable anterior mesh versus anterior colporrhaphy in symptomatic, advanced pelvic organ prolapse surgery. Int Urogynecol J. 2014;25(2):257–64.
Wolff GF, Winters JC, Krlin RM. Mesh excision: is total mesh excision necessary? Curr Urol Rep. 2016;17(4):34.
Administration USFD. Urogynecologic Surgical Mesh Implants 2019 [Available from: https://www.fda.gov/medical-devices/implants-and-prosthetics/urogynecologic-surgical-mesh-implants.
Warembourg S, Labaki M, de Tayrac R, Costa P, Fatton B. Reoperations for mesh-related complications after pelvic organ prolapse repair: 8-year experience at a tertiary referral center. Int Urogynecol J. 2017;28(8):1139–51.
Viereck V, Rautenberg O, Kociszewski J, Grothey S, Welter J, Eberhard J. Midurethral sling incision: indications and outcomes. Int Urogynecol J. 2013;24(4):645–53.
Marcus-Braun N, von Theobald P. Mesh removal following transvaginal mesh placement: a case series of 104 operations. Int Urogynecol J. 2010;21(4):423–30.
Lo TS, Tan YL, Cortes EF, Wu PY, Pue LB, Al-Kharabsheh A. Clinical outcomes of mesh exposure/extrusion: presentation, timing and management. Aust N Z J Obstet Gynaecol. 2015;55(3):284–90.
Lo TS, Lin YH, Chu HC, Cortes EF, Pue LB, Tan YL, et al. Association of urodynamics and lower urogenital tract nerve growth factor after synthetic vaginal mesh implantation on a rat model. J Obstet Gynaecol Res. 2017;43(1):173–8.
Lo TS, Lin YH, Uy-Patrimonio MC, Chu HC, Hsieh WC, Chua S. Dissecting of the paravesical space associated with lower urinary tract dysfunction—a rat model. Sci Rep. 2020;10(1):1718.
Lo TS, Lin YH, Yusoff FM, Chu HC, Hsieh WC, Uy-Patrimonio MC. The immunohistochemical and urodynamic evaluation towards the collagen-coated and non-coated polypropylene meshes implanted in the pelvic wall of the rats. Sci Rep. 2016;6:38960.
Elmer C, Blomgren B, Falconer C, Zhang A, Altman D. Histological inflammatory response to transvaginal polypropylene mesh for pelvic reconstructive surgery. J Urol. 2009;181(3):1189–95.
Lin YH, Liu G, Daneshgari F. A mouse model of simulated birth trauma induced stress urinary incontinence. Neurourol Urodyn. 2008;27(4):353–8.
Lin YH, Liu G, Kavran M, Altuntas CZ, Gasbarro G, Tuohy VK, et al. Lower urinary tract phenotype of experimental autoimmune cystitis in mouse: a potential animal model for interstitial cystitis. BJU Int. 2008;102(11):1724–30.
Velnar TBT, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanism. J Inter Med Res. 2009;37(5):1528–42.
La Fleur M, Underwood JL, Rappolee DA, Werb Z. Basement membrane and repair of injury to peripheral nerve: defining a potential role for macrophages, matrix metalloproteinases, and tissue inhibitor of metalloproteinases-1. J Exp Med. 1996;184(6):2311–26.
Hill AJ, Unger CA, Solomon ER, Brainard JA, Barber MD. Histopathology of excised midurethral sling mesh. Int Urogynecol J. 2015;26(4):591–5.
Li L, Wang X, Park JY, Chen H, Wang Y, Zheng W. Pathological findings in explanted vaginal mesh. Hum Pathol. 2017;69:46–54.
Lee R, Kermani P, Teng KK, Hempstead BL. Regulation of cell survival by secreted proneurotrophins. Science. 2001;294(5548):1945–8.
Coelho A, Wolf-Johnston AS, Shinde S, Cruz CD, Cruz F, Avelino A, et al. Urinary bladder inflammation induces changes in urothelial nerve growth factor and TRPV1 channels. Br J Pharmacol. 2015;172(7):1691–9.
Feiner B, Maher C. Vaginal mesh contraction: definition, clinical presentation, and management. Obstet Gynecol. 2010;115(2 Pt 1):325–30.
Crosby EC, Abernethy M, Berger MB, DeLancey JO, Fenner DE, Morgan DM. Symptom resolution after operative management of complications from transvaginal mesh. Obstet Gynecol. 2014;123(1):134–9.
Tijdink MM, Vierhout ME, Heesakkers JP, Withagen MI. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Int Urogynecol J. 2011;22(11):1395–404.
Marks BK, Goldman HB. Controversies in the management of mesh-based complications: a urology perspective. Urol Clin North Am. 2012;39(3):419–28.
Rac G, Greiman A, Rabley A, Tipton TJ, Chiles LR, Freilich DA, et al. Analysis of complications of pelvic mesh excision surgery using the Clavien-Dindo classification system. J Urol. 2017;198(3):638–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclaimer
This study was supported by Chang Gung University Hospital research grant CMRPG2H0281.
Conflict of interest
The authors claim no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lo, TS., Lin, YH., Huang, TX. et al. Immunochemical and urodynamic outcomes after polypropylene mesh explant from the pelvic wall of rats. Int Urogynecol J 33, 1839–1848 (2022). https://doi.org/10.1007/s00192-021-04842-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04842-7