Abstract
Introduction and hypothesis
The objective was to overview the literature on the existing pelvic floor procedure registries and databases and to identify patient demographic, clinical and/or patient-reported data items for inclusion in the Australasian Pelvic Floor Procedure Registry (APFPR) Minimum Data Set (MDS).
Methods
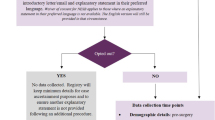
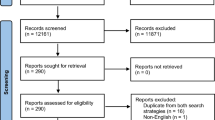
We conducted a literature search on the MEDLINE, Embase, CINAHL and PsycINFO databases in addition to Google Scholar and grey literature to identify studies in the period January 2008 to January 2020. All were English studies of registries and databases on female adults undergoing surgery for pelvic floor disorders including stress urinary incontinence (SUI) and pelvic organ prolapse (POP). Studies were assessed on demographic and clinical patient characteristics, procedure or treatment type, health-related quality of life, adverse events and safety outcomes, captured by pelvic floor procedure registries or databases that have been established to date.
Results
From 1662 studies, 29 publications describing 22 different pelvic floor registries and databases were included for analysis, 12 (55%) of which were multicentre. Six (27%) registries and databases involved solely SUI, eight (36%) were regarding POP, and the remaining eight (36%) focussed on both conditions. The majority of registries and databases captured similar details on patient characteristics, comorbidities and other clinical features, procedure or treatment type, health-related quality of life, adverse events, safety and efficacy.
Conclusion
The findings of this scoping review will assist in determining the MDS for the APFPR, an initiative of the Australian government, to improve health and quality of life outcomes of women who undergo pelvic floor reconstructive procedures.

Similar content being viewed by others
References
Australian Government response to the Senate Community Affairs References Committee report: The number of women in Australia who have had transvaginal mesh implants and related matters. 28 March 2018. © Commonwealth of Australia 2018. ISBN 978-1-76010-701-7 https://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/MeshImplants/Report.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. https://doi.org/10.1002/nau.20798.
Weber AM, Walters MD, Piedmonte MR, Ballard LA. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185(6):1299–304; discussion 1304-1296. https://doi.org/10.1067/mob.2001.119081.
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn. 2011;30(1):2–12. https://doi.org/10.1002/nau.21036.
Daly J, Ahern S, Herkes R, O'Connell H. The Australasian pelvic floor procedure registry: not before time. Aust N Z J Obstet Gynaecol. 2019;59:473–6.
Bjelic-Radisic V, Aigmueller T, Preyer O, Ralph G, Geiss I, Muller G, et al. Vaginal prolapse surgery with transvaginal mesh: results of the Austrian registry. Int Urogynecol J. 2014;25(8):1047–52. https://doi.org/10.1007/s00192-014-2333-x.
Bradley CS, Visco AG, Weber LeBrun EE, Barber MD. The pelvic floor disorders registry: purpose and development. Female Pelvic Med Reconstr Surg. 2016;22(2):77–82. https://doi.org/10.1097/SPV.0000000000000254.
Hansen MF, Lose G, Kesmodel US, Gradel KO. Repeat surgery after failed midurethral slings: a nationwide cohort study, 1998-2007. Intl Urogynecol J. 2016;27(7):1013–9. https://doi.org/10.1007/s00192-015-2925-0.
Weber LeBrun E, Adam RA, Barber MD, Boyles SH, Iglesia CB, Lukacz ES, et al. Pelvic floor disorders registry: study design and outcome measures. Female Pelvic Med Reconstr Surg. 2016;22(2):70–6. https://doi.org/10.1097/SPV.0000000000000237.
Wilcox N, McNeil JJ. Clinical quality registries have the potential to drive improvements in the appropriateness of care. Med J Aust. 2016;205(10):S27–s29.
Evans SM, Bohensky M, Cameron PA, McNeil J. A survey of Australian clinical registries: can quality of care be measured? Intern Med J. 2011;41(1a):42–8. https://doi.org/10.1111/j.1445-5994.2009.02068.x.
Md Emdadul Hoque D, Ruseckaite R, Lorgelly P, McNeil JJ, Evans SM. Cross-sectional study of characteristics of clinical registries in Australia: a resource for clinicians and policy makers. Int J Qual Health Care. 2018;30(3):192–9. https://doi.org/10.1093/intqhc/mzx196.
Australian Parliament, Senate, Community Affairs References Committee, Siewert R. Number of women in Australia who have had transvaginal mesh implants and related matters, 2018. https://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/MeshImplants.
Håkonsen SJ, Pedersen PU, Bygholm A, Peters MD, Bjerrum M. Speaking the same language: development of a nutrition minimum data set for healthcare professionals in primary healthcare. Health Informatics J. 2020;26(1):248–63. https://doi.org/10.1177/1460458218824707.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/m18-0850.
Costantini E, Zucchi A, Lazzeri M, Del Zingaro M, Vianello A, Porena M. Managing mesh erosion after abdominal pelvic organ prolapse repair: ten years' experience in a single center. Urol Int. 2011;86(4):419–23. https://doi.org/10.1159/000324243.
Moran P, Foon R, Assassa P. The BSUG national database: concept, design, implementation and beyond. Obstet Gynaecol. 2013;15:120–7.
Patil A, Moran P, Duckett J, British Society of Urogynaecology Audit C. How do urogynaecologists treat failed suburethral slings? Experience from the British Society of Urogynaecology database and literature review. J Obstet Gynaecol. 2011;31(6):514–7. https://doi.org/10.3109/01443615.2011.581319.
Trochez RD, Lane S, Duckett J. The use of synthetic mesh for vaginal prolapse in the UK: a review of cases submitted to the British Society of Urogynaecology database. Intl Urogynecol J. 2018;29(6):899–904. https://doi.org/10.1007/s00192-018-3595-5.
Dyrkorn OA, Kulseng-Hanssen S, Sandvik L. TVT compared with TVT-O and TOT: results from the Norwegian National Incontinence Registry. Int Urogynecol J. 2010;21(11):1321–6. https://doi.org/10.1007/s00192-010-1195-0.
Moe K, Schiotz HA, Kulseng-Hanssen S. Outcome of TVT operations in women with low maximum urethral closure pressure. Neurourol Urodynam. 2017;36(5):1320–4. https://doi.org/10.1002/nau.23044.
Moksnes LR, Svenningsen R, Schiotz HA, Moe K, Staff AC, Kulseng-Hanssen S. Sling mobilization in the management of urinary retention after mid-urethral sling surgery. Neurourol Urodynam. 2017;36(4):1091–6. https://doi.org/10.1002/nau.23046.
Carter-Brooks CM, Lowder JL, Du AL, Lavelle ES, Giugale LE, Shepherd JP. Restoring genital Hiatus to normative values after apical suspension alone versus with level 3 support procedures. Female Pelvic Med Reconstr Surg. 2019;25(3):226–30. https://doi.org/10.1097/SPV.0000000000000528.
Cashman S, Biers S, Greenwell T, Harding C, Morley R, Cooper D, et al. Results of the British Association of Urological Surgeons female stress urinary incontinence procedures outcomes audit 2014-2017. BJU Intl. 2019;123(1):149–59. https://doi.org/10.1111/bju.14541.
Le Brun EW, Adam RA, Barber MD, Boyles SH, Iglesia CB, Lukacz ES, et al. Pelvic floor disorders registry: study design and outcome measures. Female Pelvic Med Reconstr Surg. 2016;22(2):70–6. https://doi.org/10.1097/SPV.0000000000000237.
Guldberg R, Brostrom S, Hansen JK, Kaerlev L, Gradel KO, Norgard BM, et al. The Danish urogynaecological database: establishment, completeness and validity. Intl Urogynecol J Pelvic Floor Dysfunct. 2013;24(6):983–90. https://doi.org/10.1007/s00192-012-1968-8.
Barski D, Gerullis H, Ecke T, Kranz J, Schneidewind L, Leistner N, et al. Registry of implants for the reconstruction of pelvic floor in males and females: a feasibility case series. Intl J Surg. 2017;42:27–33. https://doi.org/10.1016/j.ijsu.2017.04.028.
Bohlin KS, Ankardal M, Nussler E, Lindkvist H, Milsom I. Factors influencing the outcome of surgery for pelvic organ prolapse. Intl Urogynecol J. 2018;29(1):81–9. https://doi.org/10.1007/s00192-017-3446-9.
Cantrell AB, Rothschild J, Durbin-Johnson B, Gonzalez R, Kurzrock EA. Surgical trends in the correction of female stress urinary incontinence in academic centers within the United States. Neurourol Urodynam. 2017;36(2):394–8. https://doi.org/10.1002/nau.22940.
Gupta P, Gaines N, Bartley J, Ehlert M, Gilleran J, Fischer M, Killinger KA, Sirls LT (2016) Stress urinary incontinence after robotic assisted prolapse repair. Neurourol Urodynam 1):S102-S103. https://doi.org/10.1002/nau.22967
Karmakar D, Hayward L, Smalldridge J, Lin S. Vaginal mesh for prolapse: a long-term prospective study of 218 mesh kits from a single Centre. Intl Urogynecol J Pelvic Floor Dysfunct. 2015;26(8):1161–70. https://doi.org/10.1007/s00192-015-2658-0.
Simon M, Debodinance P (2011) Vaginal prolapse repair using the Prolifttm kit: A registry of 100 successive cases. Intl Urogynecol J Pelvic Floor Dysfunct 3):S1894. https://doi.org/10.1007/s00192-011-1521-1
Moskowitz D, Gioia KT, Wolff EM, Massman JD, Lucioni A, Kobashi KC, et al. Analysis of the completely dry rate over time after mid-urethral sling in a real-world clinical setting. Urology. 2019;126:65–9. https://doi.org/10.1016/j.urology.2018.12.036.
Tincello D, Lucente V, Khandwala S, Botha T, Grier D, Urquhart C, et al. One year results from a world-wide registry of TVT-SECURTM in women with stress urinary incontinence (SUI). Neurourol Urodynam. 2010;29(6):1033–4. https://doi.org/10.1002/nau.20973.
Lavelle RS, Christie AL, Alhalabi F, Zimmern PE. Risk of prolapse recurrence after native tissue anterior vaginal suspension procedure with intermediate to long-term Followup. J Urol. 2016;195(4):1014–20. https://doi.org/10.1016/j.juro.2015.10.138.
de Landsheere L, Smajda S, Oberweis D, Keuller H, Dehon S, Smets M, et al. Management of pelvic organ prolapse in French-speaking Belgium: the EPILAPSUS study. Gynecol Surg. 2016;13(3):165–72. https://doi.org/10.1007/s10397-016-0948-2.
Carter EJ, Pallin DJ, Mandel L, Sinnette C, Schuur JD. Emergency department catheter-associated urinary tract infection prevention: multisite qualitative study of perceived risks and implemented strategies. Infect Control Hosp Epidemiol. 2016;37(2):156–62. https://doi.org/10.1017/ice.2015.267.
Barski D, Arndt C, Gerullis H, Yang J, Boros M, Otto T, et al. Transvaginal PVDF-mesh for cystocele repair: a cohort study. Intl J Surg. 2017;39:249–54. https://doi.org/10.1016/j.ijsu.2017.02.006.
Karmakar D, Mostafa A, Abdel-Fattah M (2015) A new validated score for detecting patient-reported success on postoperative ICIQ-SF: A novel two-stage analysis from two large RCT cohorts. International Urogynecology Journal and Pelvic Floor Dysfunction 1):S81-S82. https://doi.org/10.1007/s00192-015-2713-x
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Barski D, Gerullis H, Georgas E, Bar A, Lammers B, Ramon A, et al. Coating of mesh grafts for prolapse and urinary incontinence repair with autologous plasma: exploration stage of a surgical innovation. BioMed Res Intl. 2014;2014:296498. https://doi.org/10.1155/2014/296498.
Collinet P, Ciofu C, Costa P, Cosson M, Deval B, Grise P, et al. The safety of the inside-out transobturator approach for transvaginal tape (TVT-O) treatment in stress urinary incontinence: French registry data on 984 women. Intl Urogynecol J. 2008;19(5):711–5. https://doi.org/10.1007/s00192-007-0514-6.
Rawlings T, Lavelle RS, Coskun B, Alhalabi F, Zimmern PE. Prolapse recurrence after transvaginal mesh removal. J Urol. 2015;194(5):1342–7. https://doi.org/10.1016/j.juro.2015.06.080.
Singla N, Aggarwal H, Foster J, Alhalabi F, Lemack GE, Zimmern PE. Management of urinary incontinence following suburethral sling removal. J Urol. 2017;198(3):644–9. https://doi.org/10.1016/j.juro.2017.02.3341.
Lavelle RS, Christie AL, Alhalabi F, Zimmern PE. Risk of prolapse recurrence after native tissue anterior vaginal suspension procedure with intermediate to long-term Followup. J Urol. 2016;195(4 Pt 1):1014–20. https://doi.org/10.1016/j.juro.2015.10.138.
Rawlings T, Christie A, Zimmern PE (2015) Cost analysis of the anterior vaginal wall suspension procedure in the repair of stress urinary incontinence with early grade anterior compartment prolapse. Neurourology and Urodynamics 1):S73. https://doi.org/10.1002/nau.22738
Madbouly KM, Youssef M. Laparoscopic ventral Rectopexy versus laparoscopic Wells Rectopexy for complete rectal prolapse: long-term results. J Laparoendosc Adv Surg Tech. 2018;28(1):1–6. https://doi.org/10.1089/lap.2017.0012.
Oversand SH, Staff AC, Spydslaug AE, Svenningsen R, Borstad E. Long-term follow-up after pelvic organ prolapse operations: results and need for reoperation. Neurourol Urodynam. 2012;31(6):853–5. https://doi.org/10.1002/nau.22287.
Simon M, Debodinance P. Vaginal prolapse repair using the Prolift™; kit: a registry of 100 successive cases. Eur J Obstet Gynecol Reproduct Biol. 2011;158(1):104–9. https://doi.org/10.1016/j.ejogrb.2011.04.027.
Withagen MI, Vierhout ME, Hendriks JC, Kluivers KB, Milani AL. Risk factors for exposure, pain, and dyspareunia after tension-free vaginal mesh procedure. Obstet Gynecol. 2011;118(3):629–36. https://doi.org/10.1097/AOG.0b013e31822ada95.
McKenna JB, Parkin K, Cheng Y, Moore KH. Objective efficacy of the tension-free vaginal tape in obese/morbidly obese women versus non-obese women, at median five year follow up. Aust N Z J Obstet Gynaecol. 2016;56(6):628–32. https://doi.org/10.1111/ajo.12516.
ABS (Australian Bureau of Statistics) 2017. Private hospitals A, 2015–16. ABS cat. no. 4390.0. Canberra: ABS. https://www.abs.gov.au/statistics/health/health-services/private-hospitals-australia/latest-release.
Kowalik CR, Lakeman MME, de Kraker AT, Roovers J. Effects of mesh-related complications in vaginal surgery on quality of life. Int Urogynecol J. 2019;30(7):1083–9. https://doi.org/10.1007/s00192-018-3680-9.
Hill AM, Pauls RN, Kleeman SD, Shatkin-Margolis A, Crisp CC (2018) National practice patterns regarding apical support procedures at time of hysterectomy for pelvic organ prolapse: A nsqipanalysis. Female Pelvic Medicine and Reconstructive Surgery 24 (5 Supplement 1):S102. https://doi.org/10.1097/SPV.0000000000000625
Hill B, Fletcher S, Blume J, Adam R, Ward R. Volume at first leak is associated with sling failure among women with stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2019;25(4):294–7. https://doi.org/10.1097/SPV.0000000000000549.
Funding
This work is supported by the Australian Department of Health.
Author information
Authors and Affiliations
Contributions
R Ruseckaite: Protocol development, Data collection/extraction, Manuscript writing.
JO Daly: Protocol development, Manuscript editing.
J Dean: Manuscript editing.
S Ahern: Manuscript editing.
Corresponding author
Ethics declarations
Financial disclaimer/conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruseckaite, R., Daly, J.O., Dean, J. et al. Outcomes collected in female pelvic floor surgical procedure registries and databases: a scoping review. Int Urogynecol J 32, 3113–3130 (2021). https://doi.org/10.1007/s00192-021-04839-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04839-2