Abstract
Introduction and hypothesis
We aimed to demonstrate that laparoscopic sacrocolpopexy/cervicopexy (LSC-Cx) versus anterior vaginal mesh (AVM) results in a longer vaginal length without impacting sexual activity or function.
Methods
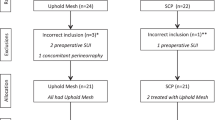
We performed a secondary analysis of sexual outcomes of a previous randomized control trial comparing LSC-Cx and AVM in 120 women (60/group) with symptomatic POP stage ≥ 3. We evaluated sexually active (SA) and non-sexually active women (NSA) using the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire-IUGA-Revised (PISQ-IR) preoperatively and 1 year postoperatively. Multivariate logistic and linear regression models were built to assess the impact of different variables on sexual activity and function, respectively.
Results
Among 120 women included, no statistically significant differences were found between vaginal length and preoperative dyspareunia (20.7% AVM vs. 22,8% LSC-Cx) comparing SA to NSA women and LSC-Cx to AVM. Vaginal length was significantly longer after LSC-Cx versus AVM (p < 0.001). The postoperative dyspareunia rate was 17.2% AVM versus 10.5% LSC-Cx. Partnered women were significantly more likely to be SA than unpartnered women before (OR = 19.04; p = 0.006) and after surgery (OR = 36.28; p = 0.002). Only dyspareunia was independently associated with sexual function pre- (B = −0.431; p = 0.017) and postoperatively (B = −0.3 96; p = 0.007).
Conclusions
Vaginal length was greater following LSC-Cx compared to AVM. While vaginal length has no impact on female sexuality pre- and postoperatively, the most important factors were “having a partner” for sexual activity and dyspareunia for sexual function. Persistence of dyspareunia was higher after AVM. LSC-Cx should be considered in women with POP undergoing mesh surgery with future sexual expectations.

Similar content being viewed by others
References
Glazener CM, Breeman S, Elders A, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet. 2016;389(10067):381–92. https://doi.org/10.1016/S0140-6736(16)31596-3.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. The Cochrane data base of systematic reviews. 2016;2:CD012079. https://doi.org/10.1002/14651858.CD012079.
Bataller E, Ros C, Anglès S, et al. Anatomical outcomes 1 year after pelvic organ prolapse surgery in patients with and without a uterus at a high risk of recurrence: a randomised controlled trial comparing laparoscopic sacrocolpopexy/cervicopexy and anterior vaginal mesh. Int Urogynecol J. 2019;30:545. https://doi.org/10.1007/s00192-018-3702-7.
Lucot JP, Cosson M, Bader G, et al. Safety of Vaginal vaginal mesh surgery versus laparoscopic mesh sacropexy for cystocele repair: results of the Prosthetic Pelvic Floor Repair (PROSPERE) Randomized Controlled Trial. Eur Urol. 2018;74(2):167–76. https://doi.org/10.1016/j.eururo.2018.01.044.
Gutman RE, Rardin CR, Sokol E, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38.e1–38.e11. https://doi.org/10.1016/j.ajog.2016.08.035.
Zhang CY, Sun ZJ, Yang J, Xu T, Zhu L, Lang JH. Sacrocolpopexy compared with transvaginal mesh surgery: a systematic review and meta-analysis. BJOG. 2020. https://doi.org/10.1111/1471-0528.16324.
Anglès-Acedo S, Ros-Cerro C, Escura-Sancho S, Palau-Pascual MJ, Bataller-Sánchez E, Espuña-Pons M, et al. Sexual activity and function in women with advanced stages of pelvic organ prolapse, before and after laparoscopic or vaginal mesh surgery. Int Urogynecol J. 2020. https://doi.org/10.1007/s00192-020-04406-1.
Mestre M, Lleberia J, Pubill J, Espuna-Pons M. Spanish version of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire IUGA-Revised (PISQ-IR): Transcultural validation. Int Urogynecol J. 2017;28:1865–73. https://doi.org/10.1007/s00192-017-3312-9.
Constantine ML, Pauls RN, Rogers RR, Rockwood TH. Validation of a single summary score for the prolapse/Incontinence sexual questionnaire–IUGA revised (PISQ-IR). Int Urogynecol J. 2017;28(12):1901–7. https://doi.org/10.1007/s00192-017-3373-9.
Sanchez-Sanchez B, Torres-Lacomba M, Yuste-Sanchez MJ, et al. Cultural adaptation and validation of the Pelvic Floor Distress Inventory short form (PFDI-20) and Pelvic Floor Impact Questionnaire short form (PFIQ-7) Spanish versions. Eur J ObstetGynecolReprodBiol. 2013;170:281–5. https://doi.org/10.1016/j.ejogrb.2013.07.006.
De La Cruz JF, Myers EM, Geller EJ. Vaginal versus robotic hysterectomy and concomitant pelvic support surgery: a comparison of postoperative vaginal length and sexual function. J Minim Invasive Gynecol. 2014;21:1010–4.
Uçar MG, et al. Sexual functioning before and after vaginal hysterectomy to treat pelvic organ prolapse and the effects of vaginal cuff closure techniques: a prospective randomised study. Eur J Obstetrics Gynecol Reprod Biol. 206:1–5.
Weber AM, Walters MD, Piedmonte MR. Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2000;182:1610–5.
Edenfield AL, Levin PJ, Dieter AA, Amundsen CL, Siddiqui NY. Sexual activity and vaginal topography in women with symptomatic pelvic floor disorders. J Sex Med. 2015;12:416–23.
Siff LN, Barber MD, Zyczynski HM, Rardin CR, Jakus-Waldman S, Rahn DD, et al. NICHD pelvic floor disorders network immediate postoperative pelvic organ prolapse quantification measures and 2-year risk of prolapse recurrence. Obstet Gynecol. 2020;136(4):792–801. https://doi.org/10.1097/AOG.0000000000004043.
Ellibeş Kaya A, Doğan O, Yassa M, Başbuğ A, Özcan C, Çalışkan E. Do external female genital measurements affect genital perception and sexual function and orgasm? Turk J Obstet Gynecol. 2020;17(3):175–81. https://doi.org/10.4274/tjod.galenos.2020.89896.
Lowenstein L, Gamble T, Sanses TV, van Raalte H, Carberry C, Jakus S, et al. Sexual function is related to body image perception in women with pelvic organ prolapse. J Sex Med. 2009;6:2286–91.
Sung VW, Rogers RG, Barber MD, Clark MA. Conceptual framework for patient-important treatment outcomes for pelvic organ prolapse. Neurourol Urodyn. 2014;33(4):414–9. https://doi.org/10.1002/nau.22397.
Lowenstein L, Gamble T, Sanses TV, van Raalte H, Carberry C, Jakus S, Pham T, Nguyen A, Hoskey K, Kenton K; Fellow’s pelvic research network. Changes in sexual function after treatment for prolapse are related to the improvement in body image perception. J Sex Med 2010;7(2 Pt 2):1023-1028. https://doi.org/10.1111/j.1743-6109.2009.01586.x
Lowder JL, Ghetti C, Moalli P, Zyczynski H, Cash TF. Body image in women before and after reconstructive surgery for pelvic organ prolapse. Int Urogynecol J. 2010;21(8):919–25. https://doi.org/10.1007/s00192-010-1141-1.
Antosh DD, Kim-Fine S, Meriwether KV, Kanter G, Dieter AA, Mamik MM, et al. Changes in sexual activity and function after pelvic organ prolapse surgery: a systematic review. Obstet Gynecol. 2020;136(5):922–31. https://doi.org/10.1097/AOG.0000000000004125.
Gupta P, Payne J, Killinger KA, et al. Analysis of changes in sexual function in women undergoing pelvic organ prolapse repair with abdominal or vaginal approaches. Int Urogynecol J. 2016;27:1919. https://doi.org/10.1007/s00192-016-3066-9.
Maher C, Baessler K, Barber M, Cheon C, Consten E, Cooper K, et al (2016) Pelvic organ prolapse surgery. In: Incontinence Abrams P, Cardozo L, Wagg A, Wein A, editors. International consultation on Incontinence, 6th edition, Tokyo; pp. 1855-1991. ISBN: 978-0-9569607-3-3.
Acknowledgements
We thank Dr. Emilia Sánchez for her contribution to the statistical analyses.
Funding
The Elevate® Anterior and Apical kits were donated by AMS as a grant for the study without any other support or supervision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bataller was a consultant for AMS (Astora Women’s Health). The remaining authors claim no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anglès-Acedo, S., Ros-Cerro, C., Escura-Sancho, S. et al. Female sexuality before and after sacrocolpopexy or vaginal mesh: is vaginal length one of the key factors?. Int Urogynecol J 33, 143–152 (2022). https://doi.org/10.1007/s00192-021-04697-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04697-y