Abstract
Introduction and hypothesis
Many women with pelvic floor dysfunction are unable to perform pelvic floor muscle (PFM) contraction. We aimed to assess the ability to contract the PFM and to evaluate the association with muscle function in Brazilian women with urinary incontinence.
Methods
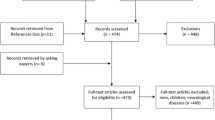
We conducted a retrospective cross-sectional study including incontinent women over the age of 18. The assessment of PFM contraction was carried out by bidigital palpation via the PERFECT scheme. We categorized our population as: group absent: women not able to contract the PFM with verbal instructions; group 1 (1st command): women able to contract their PFM after verbal instructions; group 2 (2nd command): women who needed additional training on PFM anatomy and functioning to contract them. We compared the groups regarding their PFM functionality. We used ANOVA for demographic data and Mann-Whitney test for association analyses and P value < 0.05 for statistical significance.
Results
Among 139 women included, 21 (15.1%) were not able to perform the contraction of the PFM. Sixty-five (46.7%) contracted their PFM voluntarily at the first command and 53 (38.1%) at the second command. There was a significant reduction in the PFM function in group 2 in terms of power (p < 0.001), endurance (p < 0.001) and fast contraction (p < 0.001) compared to group 1.
Conclusion
A high percentage (53.2%) of women were not able to contract their PFM voluntarily without training in PFM anatomy and functioning. Those women had impaired muscle function compared to women able to perform PFM after receiving exclusively oral instructions.


Similar content being viewed by others
Abbreviations
- ANOVA:
-
analysis of variance model
- BMI:
-
body mass index
- ES:
-
electrical stimulation
- ICS:
-
International Continence Society
- IUGA:
-
International Urogynecological Association
- MUI:
-
mixed urinary incontinence
- OAB:
-
Overactive bladder
- PFM:
-
pelvic floor muscle
- PFMT:
-
pelvic floor muscle training
- PT:
-
physical therapist
- SUI:
-
stress urinary incontinence
- UUI:
-
urgency urinary incontinence
References
Fultz NH, Herzog AR. Epidemiology of urinary symptoms in the geriatric population. Urol Clin North Am. 1996;23(01):1–10. https://doi.org/10.1016/s0094-0143(05)70288-3.
O’Neill AT, Hockey J, O’Brien P, et al. Knowledge of pelvic floor problems: a study of third trimester, primiparous women. Int Urogynecol J. 2017;28:125–9. https://doi.org/10.1007/s00192-016-3087-4.
Neels H, Wyndaele JJ, Tjalma WA, De Wachter S, Wyndaele M, Vermandel A. Knowledge of the pelvic floor in nulliparous women. J Phys Ther Sci. 2016;28:1524–33. https://doi.org/10.1589/jpts.28.1524.
Neels H, Tjalma WA, Wyndaele JJ, De Wachter S, Wyndaele M, Vermandel A. Knowledge of the pelvic floor in menopausal women and in peripartum women. J Phys Ther Sci. 2016;28(11):3020–9. https://doi.org/10.1589/jpts.28.3020.
Fante JF, Silva TD, Mateus-Vasconcelos ECL, Ferreira CHJ, Brito LGO. Do women have adequate knowledge about pelvic floor dysfunctions? A systematic review. Rev Bras Ginecol Obstet. 2019;41:508–19. https://doi.org/10.1055/s-0039-1695002.
Freitas LM, Bø K, Fernandes ACNL, Uechi N, Duarte TB, Ferreira CHJ. Pelvic floor muscle knowledge and relationship with muscle strength in Brazilian women: a cross-sectional study. Int Urogynecol J. 2019;30(11):1903–9. https://doi.org/10.1007/s00192-018-3824-y.
Berzuk K, Shay B. Effect of increasing awareness of pelvic floor muscle function on pelvic floor dysfunction: a randomized controlled trial. Int Urogynecol J. 2015;26:837–44. https://doi.org/10.1007/s00192-014-2599-z.
Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654. https://doi.org/10.1002/14651858.CD005654.pub4.
Kegel AH. Stress incontinence and genital relaxation. Clin Symp. 1952;4(2):35–51.
Talasz H, Himmer-Perschak G, Marth E, Fischer-Colbrie J, Hoefner E, Lechleitner M. Evaluation of pelvic floor muscle function in a random group of adult women in Austria. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(1):131–5. https://doi.org/10.1007/s00192-007-0404-y.
Talasz H, Gosch M, Enzelsberger H, Rhomberg HP. Female geriatric patients with urinary incontinence symptoms and their control over pelvic floor muscles. Z Gerontol Geriatr. 2005;38(6):424–30. https://doi.org/10.1007/s00391-005-0301-2.
Bø K, Mørkved S. Motor learning. In: Bø K, Berghmans B, Mørkved S, Van Kampen M, editors. Evidence-based physical therapy for the pelvic floor. Edinburgh: Elsevier; 2015. p. 111–7.
Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001;87(12):631–42. https://doi.org/10.1016/S0031-9406(05)61108-X.
Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn. 2005;24(4):374–80. https://doi.org/10.1002/nau.20144.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Peschers UM, Voduŝek DB, Fanger G, Schaer GN, DeLancey JO, Schuessler B. Pelvic muscle activity in nulliparous volunteers. Neurourol Urodyn. 2001;20(3):269–75. https://doi.org/10.1002/nau.1004.
Devreese A, Staes F, Weerdt W, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190–7. https://doi.org/10.1002/nau.20018.
Constantinou CE, Hvistendahl G, Ryhammer A, et al. Determining the displacement of the pelvic floor and pelvic organs during voluntary contractions using magnetic resonance imaging in younger and older women. BJU Int. 2002;90:408–14. https://doi.org/10.1046/j.1464-410x.2002.02907.x.
Bump RC, Hurt WG, Fantl JA, Wyman JF. Assessment of Kegel pelvic muscle exercise performance after brief verbal instruction. Am J Obstet Gynecol. 1991;165(2):322–7. https://doi.org/10.1016/0002-9378(91)90085-6.
Faulkner JA, Larkin LM, Claflin DR, Brooks SV. Age-related changes in the structure and function of skeletal muscles. Clin Exp Pharmacol Physiol. 2007;34(11):1091–6. https://doi.org/10.1111/j.1440-1681.2007.04752.x.
Koelbl H, Strassegger H, Riss PA, et al. Morphologic and functional aspects of pelvic floor muscles in patients with pelvic relaxation and genuine stress incontinence. Obstet Gynecol. 1989;74(5):789–95.
Smith AR, Hosker GL, Warrell DW. The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine. A neurophysiological study. Br J Obstet Gynaecol. 1989;96(1):24–8. https://doi.org/10.1111/j.1471-0528.1989.tb01571.x.
Bø K, Larsen S, Oseid S, et al. Knowledge about and ability to correct pelvic floor muscle exercises in women with stress urinary incontinence. Neurourol Urodyn. 1988;7(3):261–2.
Dietz HP, Wilson PD, Clarke B. The use of perineal ultrasound to quantify levator activity and teach pelvic floor muscle exercises. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(3):166–8. https://doi.org/10.1007/s001920170059.
Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Assessment of voluntary pelvic floor muscle contraction in continent and incontinent women using transperineal ultrasound, manual muscle testing and vaginal squeeze pressure measurements. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(6):624–30. https://doi.org/10.1007/s00192-006-0081-2.
Fall M, Lindström S. Electrical stimulation: a physiologic approach to the treatment of urinary incontinence. Urol Clin North Am. 1991;18:393–407.
Stewart F, Berghmans B, Bø K, Glazener CMA. Electrical stimulation with non-implanted devices for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;12(12):CD012390. https://doi.org/10.1002/14651858.CD012390.pub2.
Wilson PD, Al Samarrai T, Deakin M, Kolbe E, Brown AD. An objective assessment of physiotherapy for female genuine stress incontinence. Br J Obstet Gynaecol. 1987;94(6):575–82. https://doi.org/10.1111/j.1471-0528.1987.tb03153.x.
Author information
Authors and Affiliations
Contributions
Fátima Faní Fitz: Concept idea, research design, article writing, data collection, project management.
Letícia Missen Paladini: Concept idea, research design, article writing, data collection.
Letícia de Azevedo Ferreira: Concept idea, research design, data analysis, article writing.
Márcia Maria Gimenez: Concept idea, research design, article writing.
Maria Augusta Tezelli Bortolini: Concept idea, research design, article writing, manuscript review.
Rodrigo Aquino Castro: Concept idea, research design, article writing, manuscript review.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Review Board Committee of this institution, paper no. 3.762.856.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fitz, F.F., Paladini, L.M., Ferreira, L.d. et al. Ability to contract the pelvic floor muscles and association with muscle function in incontinent women. Int Urogynecol J 31, 2337–2344 (2020). https://doi.org/10.1007/s00192-020-04469-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04469-0