Abstract
Introduction and hypothesis
Patient safety data including rates of obstetric anal sphincter injury (OASI) are often derived from hospital discharge codes. With the transition to electronic medical records (EMRs), we hypothesized that electronic provider-entered delivery data would more accurately document obstetric perineal injury than traditional billing/diagnostic codes.
Methods
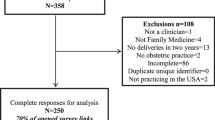
We evaluated the accuracy of perineal laceration diagnoses after singleton vaginal deliveries during one calendar year at an American tertiary academic medical center. We reviewed the entire hospital chart to determine the most likely laceration diagnosis and compared that expert review diagnosis (ExpRD) with documentation in the EMR delivery summary (EDS) and ICD-9 diagnostic codes (IDCs).
Results
We retrospectively selected 354 total delivery records. OASI complicated 56 of those. 303 records (86%) were coded identically by the EDS and IDCs. Diagnoses from the IDCs and the EDS were mostly correct compared with ExpRD (sensitivity = 96%, specificity = 100%). There was no systematic over- or under-diagnosis of OASI for either the EDS (p = 0.070) or the IDCs (p = 0.447). When considering all laceration types the EDS was correct for 21 (5.9%) lacerations that were incorrect according to the IDCs. Overall, the EDS was more accurate (p < 0.05) owing to errors in IDC minor laceration diagnoses.
Conclusions
Electronic medical record delivery summary data and EMR-derived diagnostic codes similarly characterize OASI. The EDS does not improve OASI reporting, but may be more accurate when considering all perineal lacerations. This assumes that providers have correctly identified and categorized the lacerations that they record in the EMR.

Similar content being viewed by others
References
Waldman R. ACOG practice bulletin no. 198: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2019;133(1):185.
Chisholm P, Sellner A, Kilpatrick CC, Swaim LS, Orejuela FJ. Improving documentation of obstetric anal sphincter injuries (OASIS) using a standardized electronic template at two university-affiliated institutions. South Med J. 2019;112(3):185–9.
Hines AL, Jiang HJ. Rates of obstetric trauma, 2009. HCUP statistical brief #129. Rockville: Agency for Healthcare Research and Quality; 2012.
Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, Kenton K, Gossett DR. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125(5):1088–93.
Marsh F, Rogerson L, Landon C, Wright A. Obstetric anal sphincter injury in the UK and its effect on bowel, bladder and sexual function. Eur J Obstet Gynecol Reprod Biol. 2011;154(2):223–7.
Orlovic M, Carter AW, Marti J, Mossialos E. Estimating the incidence and the economic burden of third and fourth-degree obstetric tears in the English NHS: an observational study using propensity score matching. BMJ Open. 2017;7(6):e015463.
Patient Safety Indicators™ v2019 ICD-10-CM/PCS Benchmark Data Tables. 2019; Available from: https://www.qualityindicators.ahrq.gov/Downloads/Modules/PSI/V2019/Version_2019_Benchmark_Tables_PSI.pdf. Accessed 15 April 2020.
Blondel B, Alexander S, Bjarnadóttir RI, et al. Variations in rates of severe perineal tears and episiotomies in 20 European countries: a study based on routine national data in Euro-Peristat project. Acta Obstet Gynecol Scand. 2016;95(7):746–54.
National Voluntary Consensus Standards for perinatal care 2008: a consensus report. Washington, DC: National Quality Forum (NQF); 2009.
OECD. Health at a glance 2019: OECD indicators. Paris: OECD Publishing; 2019. https://doi.org/10.1787/4dd50c09-en. Accessed 3 June 2020.
Romano PS, Yasmeen S, Schembri ME, Keyzer JM, Gilbert WM. Coding of perineal lacerations and other complications of obstetric care in hospital discharge data. Obstet Gynecol. 2005;106(4):717–25.
Brubaker L, Bradley CS, Handa VL, et al. Anal sphincter laceration at vaginal delivery: is this event coded accurately? Obstet Gynecol. 2007;109(5):1141–5.
Grobman WA, Feinglass J, Murthy S. Are the Agency for Healthcare Research and Quality obstetric trauma indicators valid measures of hospital safety? Am J Obstet Gynecol. 2006;195(3):868–74.
Core Team, R. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015.
2015 ICD-9-CM Diagnosis Code 664.0-664.4. 2015; Available from: https://www.icd9data.com/2015/Volume1/630-679/default.htm. Accessed 31 Jul 2020.
Committee on Patient Safety and Quality Improvement; Committee on Practice Management.Committee opinion no. 621: patient safety and health information technology. Obstet Gynecol. 2015;125(1):282–3.
Maxwell AE. Comparing the classification of subjects by two independent judges. Br J Psychiatry. 1970;116(535):651–5.
Gamer M, et al. Irr: various coefficients of interrater reliability and agreement; 2012.
Højsgaard S, Halekoh U, Yan J. Geepack: generalized estimating equation package; 2014.
Taylor LK, Travis S, Pym M, Olive E, Henderson-Smart DJ. How useful are hospital morbidity data for monitoring conditions occurring in the perinatal period? Aust N Z J Obstet Gynaecol. 2005;45(1):36–41.
Boggs EW, Berger H, Urquia M, McDermott CD. Recurrence of obstetric third-degree and fourth-degree anal sphincter injuries. Obstet Gynecol. 2014;124(6):1128–34.
Jango H, Langhoff-Roos J, Rosthøj S, Sakse A. Recurrent obstetric anal sphincter injury and the risk of long-term anal incontinence. Am J Obstet Gynecol. 2017;216(6):610.e1–8.
Ramm O, Woo VG, Hung Y-Y, Chen H-C, Ritterman Weintraub ML. Risk factors for the development of obstetric anal sphincter injuries in modern obstetric practice. Obstet Gynecol. 2018;131(2):290–6.
Ogrinc G, Davies L, Goodman D, Batalden PB, Davidoff F, Stevens D. SQUIRE 2.0 (standards for QUality improvement reporting excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25:986–92.
Nair M, Kurinczuk JJ, Knight M. Establishing a National Maternal Morbidity Outcome Indicator in England: a population-based study using routine hospital data. PLoS One. 2016;11(4):e0153370.
OECD/EU. Health at a glance: Europe 2018: state of health in the EU cycle. Paris: OECD Publishing; 2018. https://doi.org/10.1787/health_glance_eur-2018-en. Accessed 3 June 2020.
Morris A, Berg M, Dencker A. Professional’s skills in assessment of perineal tears after childbirth—a systematic review. Open J Obstet Gynecol. 2013;3:7–15.
Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries--myth or reality? BJOG. 2006;113(2):195–200.
Diko S, Guiahi M, Nacht A, et al. Prevention and management of severe obstetric anal sphincter injuries (OASIs): a national survey of nurse-midwives. Int Urogynecol J. 2020;31(3):591–604.
Diko S, Sheeder J, Guiahi M, et al. Identification of obstetric anal sphincter injuries (OASIs) and other lacerations: a national survey of nurse-midwives. Int Urogynecol J. 2020. https://doi.org/10.1007/s00192-020-04304-6.
Jansson MH, Nilsson K, Franzén K. Development and validation of a protocol for documentation of obstetric perineal lacerations. Int Urogynecol J. 2019;30(12):2069–76.
Acknowledgements/funding
This publication was supported by the UCDenver Department of Obstetrics and Gynecology and an unrestricted quality improvement grant from Pfizer Pharmaceuticals. KJH was supported by a Society for Maternal Fetal Medicine/American Association of Obstetricians and Gynecologists Foundation Scholar award. REDCap use was supported in part by NIH/NCRR Colorado CTSI Grant Number UL1 RR025780. Data analysis was supported by NIH/NCATS Colorado CTSI Grant Number UL1 TR000154. The contents of this publication are the authors’ sole responsibility and do not necessarily represent official NIH views.
Author information
Authors and Affiliations
Contributions
B. Wakefield: project development, manuscript writing. S. Diko: manuscript writing, manuscript editing; R. Gilmer: project development, data collection, data analysis, manuscript editing; K.A. Connell: project development, manuscript editing; P.E. DeWitt: project development, data analysis, manuscript editing; K.J. Hurt: project development, data collection, manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wakefield, B., Diko, S., Gilmer, R. et al. Accuracy of obstetric laceration diagnoses in the electronic medical record. Int Urogynecol J 32, 1907–1915 (2021). https://doi.org/10.1007/s00192-020-04450-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04450-x