Abstract
Introduction and hypothesis
Clinical quality improvement relies on accurate understanding of current practice. We performed a cross-sectional national survey of certified nurse-midwives (CNMs) assessing classification and identification of obstetric anal sphincter injury (OASI) and other delivery lacerations. We hypothesized laceration diagnoses are frequently inaccurate, and delivery records for obstetric lacerations may be of questionable quality.
Methods
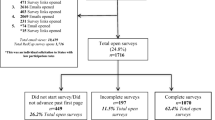
We emailed 6909 American College of Nurse Midwives members an internet-based survey link. Of respondents, we included clinically active CNMs who perform at least one delivery per month. We evaluated laceration knowledge and application using standard descriptive text and images and asked about processes for recording lacerations in the delivery record.
Results
We received 1070 (15.5%) completed surveys and 832 (77.8%) met inclusion criteria. Over 50% characterized their OASI training and ability to identify OASI as good/excellent. Most (79%) had never attended education review on OASI. The overall accuracy for classification and identification of perineal lacerations ranged from 49 to 99%. Non-perineal lacerations were frequently categorized using the perineal/OASI system. Half of respondents (51%) document their deliveries in an electronic medical record but a quarter (28%) are not personally responsible for approving delivery data. Younger participants without a doctoral degree, with self-assessed good/excellent laceration training, and caring for < 50% publicly insured patients had higher accuracy for laceration identification and diagnosis.
Conclusions
We found high rates of inaccurate laceration diagnosis and inappropriate application of the perineal OASI degree system, suggesting education and training are needed. Clinical studies that rely on delivery diagnosis of OASI may not be reliable.
Similar content being viewed by others
References
Practice Bulletin No. 198: Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstet Gynecol. 2018;132(3):e87–e102. https://doi.org/10.1097/AOG.0000000000002841.
Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927–37. https://doi.org/10.1097/AOG.0000000000000720.
Marsh F, Lynne R, Christine L, Alison W. Obstetric anal sphincter injury in the UK and its effect on bowel, bladder and sexual function. Eur J Obstet Gynecol Reprod Biol. 2011;154(2):223–7. https://doi.org/10.1016/j.ejogrb.2010.09.006.
Chescheir N, Meints L. Prospective study of coding practices for cesarean deliveries. Obstet Gynecol. 2009;114(2 Pt 1):217–23. https://doi.org/10.1097/AOG.0b013e3181ad9533.
Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148(1):99–104. https://doi.org/10.1016/j.ahj.2004.02.013.
Losina E, Barrett J, Baron JA, Katz JN. Accuracy of Medicare claims data for rheumatologic diagnoses in total hip replacement recipients. J Clin Epidemiol. 2003;56(6):515–9. https://doi.org/10.1016/s0895-4356(03)00056-8.
Fernando RJ, Sultan AH, Radley S, Jones PW, Johanson RB. Management of obstetric anal sphincter injury: a systematic review & national practice survey. BMC Health Serv Res. 2002;2(1):9.
Sultan AHKM, Hudson CN. Obstetric perineal trauma: an audit of training. J Obstet Gynecol. 1995;15:19–23.
Mutema EK. A tale of two cities: auditing midwifery practice and perineal trauma. Br J Midwifery. 2007;15:511–3.
Brubaker L, Bradley CS, Handa VL, Richter HE, Visco A, Brown MB, Weber AM (2007) Anal sphincter laceration at vaginal delivery: is this event coded accurately? http://www.ncbi.nlm.nih.gov/pubmed/17470596.
Diko S, Guiahi M, Nacht A, Connell KA, Reeves S, Bailey BA, et al. Prevention and Management of Severe Obstetric Anal Sphincter Injuries (OASIs): a National Survey of nurse- midwives. Int Urogynecol J. 2019. https://doi.org/10.1007/s00192-019-03897-x.
Harris PATR, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Nair R, Aggarwal R, Khanna D. Methods of formal consensus in classification/diagnostic criteria and guideline development. Semin Arthritis Rheum. 2011;41(2):95–105. https://doi.org/10.1016/j.semarthrit.2010.12.001.
Hamilton BEMJ, Osterman MJK, Curtin SC, Mathews TJ (2015) Births: Final Data for 2014. National Center for Health Statistics. https://www.midwife.org/acnm/files/cclibraryfiles/filename/000000007531/EssentialFactsAboutMidwives-UPDATED.pdf. Accessed Dec 20 2019.
Leeman L, Rogers R, Borders N, Teaf D, Qualls C. The effect of perineal lacerations on pelvic floor function and anatomy at 6 months postpartum in a prospective cohort of nulliparous women. Birth. 2016;43(4):293–302. https://doi.org/10.1111/birt.12258.
Handa VL, Blomquist JL, McDermott KC, Friedman S, Munoz A. Pelvic floor disorders after vaginal birth: effect of episiotomy, perineal laceration, and operative birth. Obstet Gynecol. 2012;119(2 Pt 1):233–9. https://doi.org/10.1097/AOG.0b013e318240df4f.
Yadav S, Kazanji N, Narayan KC, Paudel S, Falatko J, Shoichet S, et al. Comparison of accuracy of physical examination findings in initial progress notes between paper charts and a newly implemented electronic health record. J Am Med Inform Assoc. 2017;24(1):140–4.
Hollenbeck SM, Bomar JD, Wenger DR, Yaszay B. Electronic medical record adoption: the effect on efficiency, completeness, and accuracy in an academic Orthopaedic practice. J Pediatr Orthop. 2017;37(6):424–8. https://doi.org/10.1097/BPO.0000000000000679.
Sioutis D, Thakar R, Sultan AH. Overdiagnosis and rising rate of obstetric anal sphincter injuries (OASIS): time for reappraisal. Ultrasound Obstet Gynecol. 2017;50(5):642–7. https://doi.org/10.1002/uog.17306.
Agency for Healthcare Research and Quality. Guide to Patient Safety Indicators. (2007) U.S. Department of Health and Human Services http://www.qualityindicators.ahrq.gov/downloads/modules/psi/v31/psi_guide_v31.pdf. Accessed Dec 20 2019.
Agency for Healthcare Research and Quality. (2014) U.S. Department of Health and Human Services https://nhqrnet.ahrq.gov/inhqrdr/data/submit. Accessed Dec 20 2019.
Agency for Healthcare Research and Quality. PSI 18 and 19: Obstetric Trauma Rate – Vaginal Delivery With and Without Instrument. http://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/qitoolkit/d4k-laceration-bestpractices.pdf. Accessed Dec 20 2019.
ACOG (2015) Patient Safety and Quality Improvement http://www.acog.org/About_ACOG/ACOG_Departments/Patient_Safety_and_Quality_Improvement/~/media/Departments/PatientSafetyandQualityImprovement/201213IssuesandRationale-Delivery.pdf Accessed Jan 5 2015.
2015 ICD-9-CM Diagnosis Code 664.0-664.4. (2015). http://www.icd9data.com/2015/Volume1/630-679/660-669/664/664.0.htm. Accessed Nov 8 2019.
Bernheim SM, Ross JS, Krumholz HM, Bradley EH. Influence of patients' socioeconomic status on clinical management decisions: a qualitative study. Ann Fam Med. 2008;6(1):53–9. https://doi.org/10.1370/afm.749.
Pamuk E, Makuc D, Heck K, Reuben C, Lochner K (1998) Socioeconomic status and health chartbook. Health, United States 1998.
Kim MK, Lee SM, Bae SH, Kim HJ, Lim NG, Yoon SJ, Lee JY, Jo MW (2018) Socioeconomic status can affect pregnancy outcomes and complications, even with a universal healthcare system. Int J Equity Health 17. doi:https://doi.org/10.1186/s12939-017-0715-7.
Silva LM, Coolman M, Steegers EA, Jaddoe VW, Moll HA, Hofman A, et al. Low socioeconomic status is a risk factor for preeclampsia: the generation R study. J Hypertens. 2008;26(6):1200–8. https://doi.org/10.1097/HJH.0b013e3282fcc36e.
Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41(5):545–7. https://doi.org/10.1188/14.ONF.545-547.
Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. https://doi.org/10.2196/jmir.6.3.e34.
Acknowledgements
We thank the ACNM staff and all the participant members without whom we could not have done this work. We appreciate the fine work of Tim Phelps, Associate Professor/Medical Illustrator, from the Department of Art as Applied to Medicine at Johns Hopkins University School of Medicine for creating the laceration images. We thank Beth Bailey for statistical advice and Brian W. Wakefield and Jason G. Bunn for helpful manuscript review.
Funding
This work was supported by the Rocky Vista University College of Osteopathic Medicine Intramural Research Grant (SD), the Society of Family Planning Junior Investigator Career Grant SFPRF10-JI1 (MG), the University of Colorado Department of OB-Gyn, and the Society for Maternal Fetal Medicine/American Association of Obstetricians and Gynecologists Scholar Award (KJH). The RedCap resource is supported by the NIH/NCRR Colorado CTSI Grant Number UL1 RR025780. The contents of this manuscript are the authors’ sole responsibility and do not necessarily represent official UC Denver, Rocky Vista University, or NIH views.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 323 kb)
Rights and permissions
About this article
Cite this article
Diko, S., Sheeder, J., Guiahi, M. et al. Identification of obstetric anal sphincter injuries (OASIs) and other lacerations: a national survey of nurse-midwives. Int Urogynecol J 32, 1745–1753 (2021). https://doi.org/10.1007/s00192-020-04304-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04304-6