Abstract
Aim
To compare urethral sphincter measurements in women with different urodynamic diagnoses using three-dimensional transperineal ultrasound (TPU).
Methods
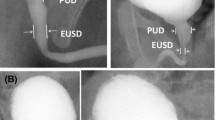
Women with lower urinary tract dysfunction having urodynamic studies (UDS) were prospectively recruited to this study. A detailed history and vaginal examination were conducted. Saline cystometry was performed and the women were divided into groups according to their urodynamic diagnosis, which were nondiagnostic urodynamics (NUDS), pure detrusor overactivity (PureDO), pure urodynamic stress incontinence (PureUSI) and mixed urinary incontinence (MUDS). Three-dimensional TPU was performed to measure total urethral sphincter volume, striated sphincter volume, core volume, sphincter length and maximum cross-sectional area. The ultrasound measurements were compared with the diagnostic urodynamics.
Results
One hundred fifty women were included in the study. There were 37, 53, 22 and 38 women in the groups of NUDS, PureDO, PureUSI and MUDS respectively. The average striated sphincter volumes in these groups were 1.84 ml, 2.24 ml, 1.32 ml and 1.98 ml respectively. There was no difference in average age, body mass index or presence of prolapse in these groups. All measurements were larger in the PureDO and smaller in the PureUSI group compared with the NUDS group. The measurements in the MUDS group were larger than in the NUDS group and smaller than in the PureDO group but this difference was not statistically significant.
Conclusion
The urethral sphincter of women with PureDO is larger than in women with PureUSI. The value in women with MUDS was between the two. The size of the urethral sphincter appears to be related to the pathophysiology.



Similar content being viewed by others
References
Mistry MA, Klarskov N, DeLancey JO, Lose G. A structured review on the female urethral anatomy and innervation with an emphasis on the role of the urethral longitudinal smooth muscle. Int Urogynecol J. 2019.
Rud T. The effects of estrogens and gestagens on the urethral pressure profile in urinary continent and stress incontinent women. Acta Obstet Gynecol Scand. 1980;59:265–70.
Khayyami Y, Lose G, Klarskov N. The urethral closure mechanism is deteriorated after anterior colporrhaphy. Int Urogynecol J. 2018;29:1311–6.
Khullar V, Athanasiou S, Cardozo L, Boos K, Salvatore S, Young M. Histological correlates of the urethral sphincter and surrounding structures with ultrasound imaging, 21st Annual meeting of International Urogynaecology Association, abstract 47. 1996.
Athanasiou S, Khullar V, Boos K, Salvatore S, Cardozo L. Imaging the urethral sphincter with three-dimensional ultrasound. Obstet Gynecol. 1999;94:295–301.
Shui W, Luo Y, Ying T, Li Q, Dou C, Zhou M. Assessment of female pelvic floor support to the urethra using 3D transperineal ultrasound. Int Urogynecol J. 2019.
Kirschner-Hermanns R, Klein HM, Muller U, Schafer W, Jakse G. Intra-urethral ultrasound in women with stress incontinence. Br J Urol. 1994;74:315–8.
Frauscher F, Helweg G, Strasser H, Enna B, Klauser A, Knapp R, et al. Intraurethral ultrasound: diagnostic evaluation of the striated urethral sphincter in incontinent females. Eur Radiol. 1998;8:50–3.
van de Waarsenburg MK, van Hoogenhuijze NE, Grob ATM, Schweitzer KJ, Withagen MIJ, van der Vaart CH. Method and reliability of measuring midurethral area and echogenicity, and changes during and after pregnancy. Int Urogynecol J. 2018;29:1379–85.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Delancey JO. Correlative study of paraurethral anatomy. Obstet Gynecol. 1986;68:91–7.
Digesu GA, Calandrini N, Derpapas A, Gallo P, Ahmed S, Khullar V. Intraobserver and interobserver reliability of the three-dimensional ultrasound imaging of female urethral sphincter using a translabial technique. Int Urogynecol J. 2012;23:1063–8.
Altman DG. Statistics and ethics in medical research: III how large a sample? Br Med J. 1980;281:1336–8.
Blaganje M, Lukanovic A. Ultrasound-guided autologous myoblast injections into the extrinsic urethral sphincter: tissue engineering for the treatment of stress urinary incontinence. Int Urogynecol J. 2013;24:533–5.
Athanasiou S, Chaliha C, Digesu GA, Sotiropoulou M, Georgoulias N, Khullar V, et al. The effects of duloxetine on urethral function and sphincter morphology. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:763–7.
Madill SJ, Pontbriand-Drolet S, Tang A, Dumoulin C. Changes in urethral sphincter size following rehabilitation in older women with stress urinary incontinence. Int Urogynecol J. 2015;26:277–83.
Noble JG, Dixon PJ, Rickards D, Fowler CJ. Urethral sphincter volumes in women with obstructed voiding and abnormal sphincter electromyographic activity. Br J Urol. 1995;76:741–6.
Malallah MA, Al-Shaiji TF. Pharmacological treatment of pure stress urinary incontinence: a narrative review. Int Urogynecol J. 2015;26:477–85.
Duckett J, Patil A, Aggarwal I. The effect of duloxetine on urethral sphincter morphology. Ultrasound Obstet Gynecol. 2008;31:206–9.
Duckett J, Basu M. The effect of solifenacin on urethral sphincter morphology. Int Urogynecol J. 2011;22:971–4.
Bodner-Adler B, Alarab M, Ruiz-Zapata AM, Latthe P. Effectiveness of hormones in postmenopausal pelvic floor dysfunction-International Urogynecology Association research and development-committee opinion. Int Urogynecol J. 2019.
Dietz HP, Socha M, Atan IK, Subramaniam N. Does estrogen deprivation affect pelvic floor muscle contractility? Int Urogynecol J. 2019. Dietz HP, Socha M, Atan IK, Subramaniam N. Does estrogen deprivation affect pelvic floor muscle contractility? Int Urogynecol J. 2019.
Cassado Garriga J, Pessarrodona Isern A, Rodriguez Carballeira M, Pallarols Badia M, Moya Del Corral M, Valls Esteve M, et al. Three-dimensional translabial ultrasound assessment of urethral supports and the urethral sphincter complex in stress urinary incontinence. Neurourol Urodyn. 2017;36:1839–45.
Robinson D, Toozs-Hobson P, Cardozo L, Digesu A. Correlating structure and function: three-dimensional ultrasound of the urethral sphincter. Ultrasound Obstet Gynecol. 2004;23:272–6.
Bump R, Huang KC, McClish D, Fantl JA. Effect of narcotic anaesthesia and skeletal muscle paralysis on passive and dynamic urethral function of stress continent and incontinent women. Neurourol Urodyn. 1991;10:523–32.
Haeusler G, Sam C, Chiari A, Tempfer C, Hanzal E, Koelbl H. Effect of spinal anaesthesia on the lower urinary tract in continent women. Br J Obstet Gynaecol. 1998;105:103–6.
Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol. 2012;3:260.
Robinson D, Akervall S, Wagg A, Chapple C, Milsom I, Gyhagen M. Prevalence and predictors of overactive bladder in nonpregnant nulliparous women below 65 years of age. Int Urogynecol J. 2018;29:531–7.
Juliato CR, Baccaro LF, Pedro AO, Gabiatti JR, Lui-Filho JF, Costa-Paiva L. Factors associated with urinary incontinence in middle-aged women: a population-based household survey. Int Urogynecol J. 2017;28:423–9.
Author information
Authors and Affiliations
Contributions
R Karmarkar: Project development, Data collection, Data analysis, Manuscript writing.
A Digesu: Manuscript review.
R Fernando: Manuscript review.
V Khullar: Project supervision, Manuscript editing.
Part of this work was presented at the International Continence Society’s Annual Conference in Tokyo on 14/09/2016.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare for any authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karmarkar, R., Digesu, A., Fernando, R. et al. Urethral sphincter volume and urodynamic diagnosis. Int Urogynecol J 31, 2589–2594 (2020). https://doi.org/10.1007/s00192-020-04409-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04409-y