Abstract
Introduction and hypothesis
The objective was to determine the prevalence of urinary incontinence (UI) and factors associated in a sample of Brazilian middle-aged women.
Methods
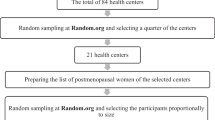
A cross-sectional study was conducted between September 2012 and June 2013 with 749 women. UI was defined as any complaint of involuntary loss of urine. The independent variables were sociodemographic data and health-related habits and problems. Statistical analysis was carried out using Chi-squared test and Poisson regression.
Results
The mean age was 52.5 (±4.4) years. The prevalence of UI was 23.6 %. Of these, 48 (6.4 %) had stress urinary incontinence, 59 (7.8 %) urinary urgency, and 70 (9.5 %) had mixed urinary incontinence. In the final statistical model, self-perception of health as fair/poor/very poor (PR: 1.90; 95 % CI, 1.45–2.49; P < 0.001), ≥1 vaginal deliveries (PR: 1.84; 95 % CI, 1.35–2.50; P < 0.001), higher body mass index (PR: 1.04; 95 % CI, 1.02–1.06; P = 0.001), vaginal dryness (PR: 1.60; 95 % CI, 1.23–2.08; P = 0.001), current or previous hormone therapy (PR: 1.38; 95 % CI, 1.06–1.81; P = 0.019), pre-/perimenopause (PR: 1.42; 95 % CI, 1.06–1.91; P = 0.021), and previous hysterectomy (PR: 1.41; 95 % CI, 1.03–1.92; P = 0.031) were associated with a greater prevalence of UI. Current or previous use of soy products to treat menopausal symptoms was associated with a lower prevalence of UI (PR: 0.43; 95 % CI, 0.24–0.78; P = 0.006).
Conclusions
Several factors are associated with UI in middle-aged Brazilian women. The results highlight the importance of carrying out interventions aimed at reducing modifiable factors.
Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(10):4–120.
Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011;29(2):185–90.
Quinn SD, Domoney C. The effects of hormones on urinary incontinence in postmenopausal women. Climacteric. 2009;12(2):106–13.
Sherburn M, Guthrie JR, Dudley EC, O’Connell HE, Dennerstein L. Is incontinence associated with menopause? Obstet Gynecol. 2001;98(4):628–33.
Juliato CRT, Baccaro LF, Pedro AO, Costa-Paiva L, Lui-Filho J, Pinto-Neto AM. Subjective urinary urgency in middle age women: a population-based study. Maturitas. 2016;85:82–7.
Instituto Brasileiro de Geografia e Estatística (IBGE). Censo 2010. Available from: http://www.ibge.gov.br. Accessed March 2011.
Pedro AO, Pinto-Neto AM, Costa-Paiva LH, et al. [Climacteric syndrome: a population-based study in Campinas, SP, Brazil.] Rev Saude Publica. 2003;37:735–42.
Kish L. Survey sampling. New York: Wiley; 1965.
Tamanini JT, Dambros M, D’Ancona CA, Palma PC, Rodrigues Netto N. [Validation of the “International Consultation on Incontinence Questionnaire—Short Form” (ICIQ-SF) for Portuguese.] Rev Saude Publica. 2004;38(3):438–44.
Pereira SB, Thiel RRC, Riccetto C, da Silva JM, Pereira LC, Herrmann V, et al. Validação do International Consultation on incontinence questionnaire overactive bladder (ICIQ-OAB) para língua portuguesa. Rev Bras Ginecol Obstet. 2010;32(6):273–8.
Heinemann LA, Potthoff P, Schneider HP. International versions of the Menopause Rating Scale (MRS). Health Qual Life Outcomes. 2003;1:282.
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag. J Clin Epidemiol. 2000;53(11):1150–7.
Guarisi T, Pinto Neto AM, Osis MJ, Pedro AO, Paiva LH, Faúndes A. Urinary incontinence among climateric Brazilian women: household survey. Rev Saude Publica. 2001;35(5):428–35.
Reigota RB, Pedro AO, de Souza Santos Machado V, Costa-Paiva L, Pinto-Neto AM. Prevalence of urinary incontinence and its association with multimorbidity in women aged 50 years or older: a population-based study. Neurourol Urodyn. 2014;35(1):62–8.
Danforth KN, Townsend MK, Lifford K, Curhan GC, Resnick NM, Grodstein F. Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol. 2006;194(2):339–45.
Waetjen LE, Ye J, Feng WY, Johnson WO, Greendale GA, Sampselle CM, et al. Association between menopausal transition stages and developing urinary incontinence. Obstet Gynecol. 2009;114(5):989–98.
Teleman PM, Persson J, Mattiasson A, Samsioe G. The relation between urinary incontinence and steroid hormone levels in perimenopausal women. A report from the Women’s Health in the Lund Area (WHILA) study. Acta Obstet Gynecol Scand. 2009;88(8):927–32.
Hendrix SL, Cochrane BB, Nygaard IE, Handa VL, Barnabei VM, Iglesia C, et al. Effects of estrogen with and without progestin on urinary incontinence. JAMA. 2005;293(8):935–48.
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012; 10:CD001405. doi:10.1002/14651858.CD001405.
Reed SD, Newton KM, LaCroix AZ, Grothaus LC, Grieco VS, Erlich K. Vaginal, endometrial, and reproductive hormone findings: randomized placebo-controlled trial of black cohosh, multibotanical herbs, and dietary soy for vasomotor symptoms: the Herbal Alternatives for Menopause (HALT) Study. Menopause. 2008;15:51–8.
Findik RB, Unluer AN, Sahin E, Bozkurt OF, Karakaya J, Unsal A. Urinary incontinence in women and Its relation with pregnancy, mode of delivery, connective tissue disease and other factors. Adv Clin Exp Med. 2012;21(2):207–13.
Faúndes A, Guarisi T, Pinto-Neto AM. The risk of urinary incontinence of parous women who delivered only by cesarean section. Int J Gynaecol Obstet. 2001;72(1):41–6.
Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand. 2010;89(12):1511–22.
Kudish BI, Shveiky D, Gutman RE, Jacoby V, Sokol AI, Rodabough R, et al. Hysterectomy and urinary incontinence in postmenopausal women. Int Urogynecol J. 2014;25(11):1523–31.
Basak T, Kok G, Guvenc G. Prevalence, risk factors and quality of life in Turkish women with urinary incontinence: a synthesis of the literature. Int Nurs Rev. 2013;60(4):448–60.
Pakgohar M, Sabetghadam S, Vasegh Rahimparvar SF, Kazemnejad A. Quality of life (QoL) and help-seeking in postmenopausal women with urinary incontinence (UI): A population based study. Arch Gerontol Geriatr. 2014;59(2):403–7.
Sturdee DW, Panay N. Recommendations for the management of postmenopausal vaginal atrophy. Climacteric. 2010;13(6):509–22.
Rud T. Urethral pressure profile in continent women from childhood to old age. Acta Obstet Gynecol Scand. 1980;59(4):331–5.
Cardozo L, Robinson D. Especial considerations in premenopausal and postmenopausal women with symptoms of overactive bladder. Urology. 2002;60(5):64–71.
Simon JA, Kokot-Kierepa M, Goldstein J, Nappi RE. Vaginal health in the United States: results from the Vaginal Health: Insights, Views & Attitudes survey. Menopause. 2013;20(10):1043–8.
Castelo-Branco C, Biglia N, Nappi RE, Schwenkhagen A, Palacios S. Characteristics of post-menopausal women with genitourinary syndrome of menopause: implications for vulvovaginal atrophy diagnosis and treatment selection. Maturitas. 2015;30:1–5.
Acknowledgements
This work was supported by the Fundação de Apoio a Pesquisa do estado de São Paulo (FAPESP), process number 2011/14526–9.
Prof Aarão Mendes Pinto-Neto is acknowledged (in memoriam) for his contributiion to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Juliato, C.R.T., Baccaro, L.F., Pedro, A.O. et al. Factors associated with urinary incontinence in middle-aged women: a population-based household survey. Int Urogynecol J 28, 423–429 (2017). https://doi.org/10.1007/s00192-016-3139-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3139-9