Abstract
Introduction and hypothesis
The purpose of our study was to describe the surgical trend and time-frame comparison between 1997–2005 (1stperiod) and 2006–2013 (2nd period) of hystero-preservation for uterine prolapse, based upon a nationwide population-based National Health Insurance (NHI) claim data in Taiwan.
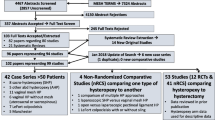
Methods
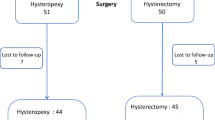
Women, who underwent primary surgeries for uterine prolapse, either uterine suspension with hystero-preservation or hysterectomy during 1997–2013, were identified from National Health Insurance Research Database (NHIRD).We analyzed the related variables including surgical types (hystero-preservation or hysterectomy), patient age and concomitant anti-incontinence surgery, surgeon age, gender, and service volume; and hospital accreditation level, and service volume.
Results
We identified a total of 46,968 inpatients, 6629 (14.11%) hystero-preservation group, and 40,339 (85.89%) hysterectomy group. Hystero-preservation significantly increased during the 17 year follow-up study period (1997 to 2013) (P value =0.0147). The overall surgeries for uterine prolapse increased among patients ≥70 years, with concomitant anti-incontinence surgery, surgeons ≥45 years, high volume surgeons, and hospitals. Multiple logistic regression revealed hysterectomy was less used in 2nd period (OR 0.45, 95%, confidence interval (CI) 0.43–0.48). Hysterectomy was more often used in patient aged ≥50 years, surgeon aged ≥45 years, and low volume hospitals. In case of concomitant anti-incontinence surgery (OR 0.48, CI 0.45–0.52), high volume surgeons (more than 30 surgeries) and hospitals (more than 73 surgeries) hystero-preservation was more often used.
Conclusions
Time-frames, younger patients, concomitant anti-incontinence surgery, younger surgeons, and high volume surgeons and hospitals increase hystero-preservation for uterine prolapse. Surgeons and hospitals should be ready to respond to the wishes of female patients who want to preserve the uterus.




Similar content being viewed by others
References
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the women's health initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6.
de Oliveira SA, Fonseca MCM, Bortolini MAT, Girao M, Roque MT, Castro RA. Hysteropreservation versus hysterectomy in the surgical treatment of uterine prolapse: systematic review and meta-analysis. Int Urogynecol J. 2017;28(11):1617–30.
Kurkijarvi K, Aaltonen R, Gissler M, Makinen J. Pelvic organ prolapse surgery in Finland from 1987 to 2009: a national register based study. Eur J Obstet Gynecol Reprod Biol. 2017;214:71–7.
Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189:372–7.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Blandon RE, Bharucha AE, Melton LJ 3rd, et al. Incidence of pelvic floor repair after hysterectomy: a population-based cohort study. Am J Obstet Gynecol. 2007;197(6):664 e1–7.
Wu MP, Long CY, Huang KH, Chu CC, Liang CC, Tang CH. Changing trends of surgical approaches for uterine prolapse: an 11-year population-based nationwide descriptive study. Int Urogynecol J. 2012;23(7):865–72.
Wu MP, Wu CJ, Weng SF. The choice of reoperation after primary surgeries for uterine prolapse: a nationwide study. Gynecol Minim Invasive Ther. 2015;4(4):120–5.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. The Cochrane database of systematic reviews. 2016;11:CD004014.
Anglim B, O'Sullivan O, O'Reilly B. How do patients and surgeons decide on uterine preservation or hysterectomy in apical prolapse? Int Urogynecol J. 2018;29(8):1075–9.
Huang LY, Chu LC, Chiang HJ, Chuang FC, Kung FT, Huang KH. Medium-term comparison of uterus preservation versus hysterectomy in pelvic organ prolapse treatment with Prolift mesh. Int Urogynecol J. 2015;26(7):1013–20.
Komisaruk BR, Frangos E, Whipple B. Hysterectomy improves sexual response? Addressing a crucial omission in the literature. J Minim Invasive Gynecol. 2011;18(3):288–95.
Kow N, Goldman HB, Ridgeway B. Management options for women with uterine prolapse interested in uterine preservation. Current urology reports. 2013;14(5):395–402.
Samuelsson EC, Victor FT, Tibblin G, Svardsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180(2 Pt 1):299–305.
Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215(1):21–33.
Bedford ND, Seman EI, O'Shea RT, Keirse MJ. Effect of uterine preservation on outcome of laparoscopic uterosacral suspension. J Minim Invasive Gynecol. 2013;20(2):172–7.
Glazener CM, Breeman S, Elders A, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet. 2017;389(10067):381–92.
Zucchi A, Lazzeri M, Porena M, Mearini L, Costantini E. Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol. 2010;7(11):626–33.
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female pelvic medicine & reconstructive surgery. 2013;19(2):103–9.
Wu MP, Long CY, Liang CC, Weng SF, Tong YC. Trends in reoperation for female stress urinary incontinence: a nationwide study. Neurourol Urodyn. 2015;34(7):693–8.
van IJsselmuiden NM, Detollenaere RJ, et al. Dutch women's attitudes towards hysterectomy and uterus preservation in surgical treatment of pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol. 2018;220:79–83.
Khan AA, Eilber KS, Clemens JQ, Wu N, Pashos CL, Anger JT. Trends in management of pelvic organ prolapse among female Medicare beneficiaries. Am J Obstet Gynecol. 2015;212(4):463 e1–8.
Food and Drug Administration. Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. July, 13, 2011. https://www.fdagov/medical-devices/implants-and-prosthetics. 2011.
Food and Drug Administration. Urogynecologic surgical mesh implants. April, 16, 2019. https://www.fdagov/medical-devices/implants-and-prosthetics. 2019.
Korbly NB, Kassis NC, Good MM, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470 e1–6.
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013;24(9):1481–7.
Altman D, Granath F, Cnattingius S, Falconer C. Hysterectomy and risk of stress-urinary-incontinence surgery: nationwide cohort study. Lancet. 2007;370(9597):1494–9.
Brubaker L, Nygaard I, Richter HE, et al. Two-year outcomes after sacrocolpopexy with and without burch to prevent stress urinary incontinence. Obstet Gynecol. 2008;112(1):49–55.
Anger JT, Rodriguez LV, Wang Q, Pashos CL, Litwin MS. The role of provider volume on outcomes after sling surgery for stress urinary incontinence. J Urol. 2007;177(4):1457–62.
Healy MA, Mullard AJ, Campbell DA Jr, Dimick JB. Hospital and payer costs associated with surgical complications. JAMA Surg. 2016;151(9):823–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, YL., Lo, TS., Long, CY. et al. Time-frame comparison of hystero-preservation in the surgical treatment of uterine prolapse: a population-based nation-wide follow-up descriptive study, 2006–2013 versus 1997–2005. Int Urogynecol J 31, 1839–1850 (2020). https://doi.org/10.1007/s00192-019-04128-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04128-z